J Breast Cancer.
2017 Mar;20(1):65-73. 10.4048/jbc.2017.20.1.65.
A Prognostic Model for Patients with Triple-Negative Breast Cancer: Importance of the Modified Nottingham Prognostic Index and Age
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University Bundang Hospital, Seongnam, Korea. inah228@snu.ac.kr
- 2Breast Care Center, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- KMID: 2379400
- DOI: http://doi.org/10.4048/jbc.2017.20.1.65
Abstract
- PURPOSE
Considering the distinctive biology of triple-negative breast cancer (TNBC), this study aimed to identify TNBC-specific prognostic factors and determine the prognostic value of the Nottingham Prognostic Index (NPI) and its variant indices.
METHODS
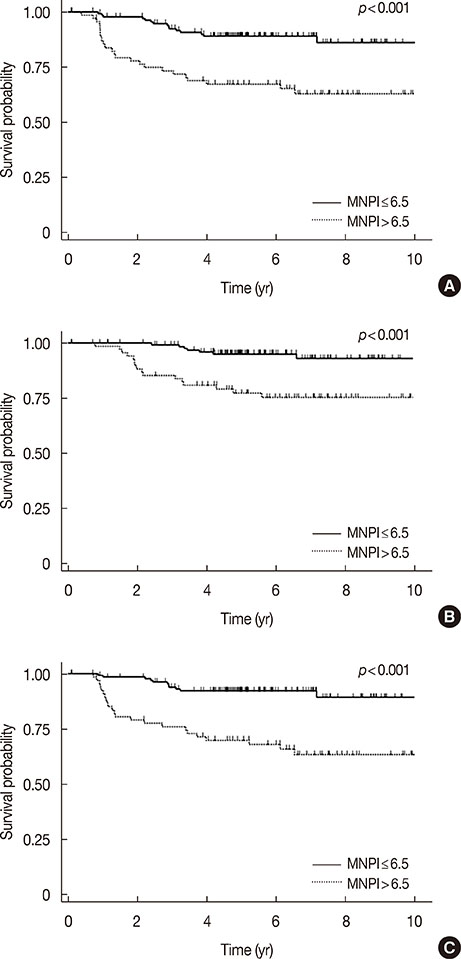
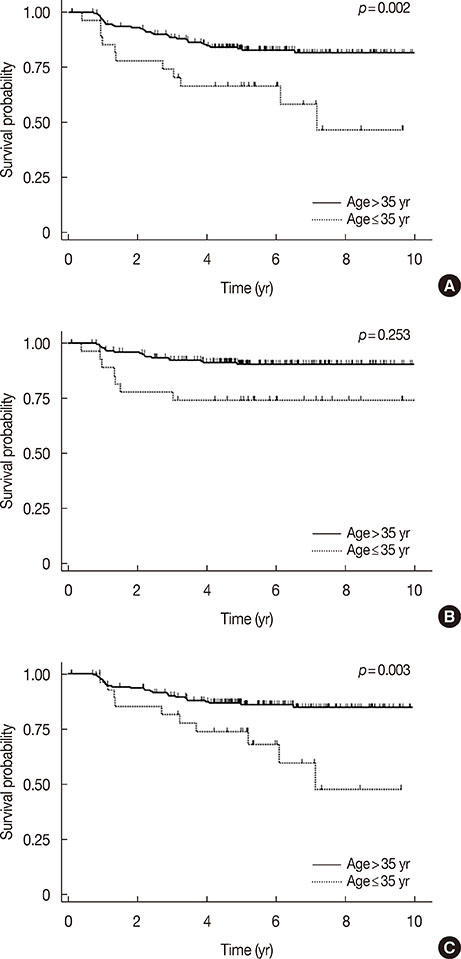
A total of 233 patients with newly diagnosed stage I to III TNBC from 2003 to 2012 were reviewed. We retrospectively analyzed the patients' demographics, clinicopathologic parameters, treatment, and survival outcomes. The NPI was calculated as follows: tumor size (cm)×0.2+node status+Scarff-Bloom-Richardson (SBR) grade. The modified NPI (MNPI) was obtained by adding the modified SBR grade rather than the SBR grade.
RESULTS
The median follow-up was 67.8 months. Five-year disease-free survival (DFS) and overall survival (OS) were 81.4% and 89.9%, respectively. Multivariate analyses showed that the MNPI was the most significant and common prognostic factor of DFS (p=0.001) and OS (p=0.019). Young age (≤35 years) was also correlated with poor DFS (p=0.006). A recursive partitioning for establishing the prognostic model for DFS was performed based on the results of multivariate analysis. Patients with a low MNPI (≤6.5) were stratified into the low-risk group (p<0.001), and patients with a high MNPI (>6.5) were subdivided into the intermediate (>35 years) and high-risk (≤35 years) groups. Age was not a prognostic factor in patients with a low MNPI, whereas in patients with a high MNPI, it was the second key factor in subdividing patients according to prognosis (p=0.023).
CONCLUSION
The MNPI could be used to stratify patients with stage I to III TNBC according to prognosis. It was the most important prognosticator for both DFS and OS. The prognostic significance of young age for DFS differed by MNPI.
MeSH Terms
Figure
Reference
-
1. Foulkes WD, Smith IE, Reis-Filho JS. Triple-negative breast cancer. N Engl J Med. 2010; 363:1938–1948.
Article2. Criscitiello C, Azim HA Jr, Schouten PC, Linn SC, Sotiriou C. Understanding the biology of triple-negative breast cancer. Ann Oncol. 2012; 23:Suppl 6. vi13–vi18.
Article3. Brewster AM, Chavez-MacGregor M, Brown P. Epidemiology, biology, and treatment of triple-negative breast cancer in women of African ancestry. Lancet Oncol. 2014; 15:e625–e634.
Article4. Gogia A, Raina V, Deo SV, Shukla NK, Mohanti BK. Triple-negative breast cancer: an institutional analysis. Indian J Cancer. 2014; 51:163–166.
Article5. Haybittle JL, Blamey RW, Elston CW, Johnson J, Doyle PJ, Campbell FC, et al. A prognostic index in primary breast cancer. Br J Cancer. 1982; 45:361–366.
Article6. Galea MH, Blamey RW, Elston CE, Ellis IO. The Nottingham Prognostic Index in primary breast cancer. Breast Cancer Res Treat. 1992; 22:207–219.
Article7. Blamey RW, Ellis IO, Pinder SE, Lee AH, Macmillan RD, Morgan DA, et al. Survival of invasive breast cancer according to the Nottingham Prognostic Index in cases diagnosed in 1990-1999. Eur J Cancer. 2007; 43:1548–1555.
Article8. Balslev I, Axelsson CK, Zedeler K, Rasmussen BB, Carstensen B, Mouridsen HT. The Nottingham Prognostic Index applied to 9,149 patients from the studies of the Danish Breast Cancer Cooperative Group (DBCG). Breast Cancer Res Treat. 1994; 32:281–290.
Article9. Chollet P, Amat S, Belembaogo E, Curé H, de Latour M, Dauplat J, et al. Is Nottingham Prognostic Index useful after induction chemotherapy in operable breast cancer? Br J Cancer. 2003; 89:1185–1191.
Article10. Albergaria A, Ricardo S, Milanezi F, Carneiro V, Amendoeira I, Vieira D, et al. Nottingham Prognostic Index in triple-negative breast cancer: a reliable prognostic tool? BMC Cancer. 2011; 11:299.
Article11. Koo TR, Eom KY, Kang EY, Kim YJ, Kim SW, Kim JH, et al. Prognostic value of the nodal ratio and Ki-67 expression in breast cancer patients treated with postmastectomy radiotherapy. J Breast Cancer. 2013; 16:274–284.
Article12. Le Doussal V, Tubiana-Hulin M, Friedman S, Hacene K, Spyratos F, Brunet M. Prognostic value of histologic grade nuclear components of Scarff-Bloom-Richardson (SBR): an improved score modification based on a multivariate analysis of 1262 invasive ductal breast carcinomas. Cancer. 1989; 64:1914–1921.
Article13. Abrial SC, Penault-Llorca F, Delva R, Bougnoux P, Leduc B, Mouret-Reynier MA, et al. High prognostic significance of residual disease after neoadjuvant chemotherapy: a retrospective study in 710 patients with operable breast cancer. Breast Cancer Res Treat. 2005; 94:255–263.
Article14. Lee JA, Kim KI, Bae JW, Jung YH, An H, Lee ES, et al. Triple negative breast cancer in Korea-distinct biology with different impact of prognostic factors on survival. Breast Cancer Res Treat. 2010; 123:177–187.
Article15. Fayaz MS, Demian GA, El-Sherify M, Abuzalouf S, George T, Samir S, et al. Is young age a poor prognostic factor in triple-negative breast cancer patients? Analysis of 363 patients from single institution registry. J Clin Oncol. 2013; 31:5 Suppl. e12023.
Article16. Ovcaricek T, Frkovic SG, Matos E, Mozina B, Borstnar S. Triple negative breast cancer: prognostic factors and survival. Radiol Oncol. 2011; 45:46–52.17. Dawson SJ, Provenzano E, Caldas C. Triple negative breast cancers: clinical and prognostic implications. Eur J Cancer. 2009; 45:Suppl 1. 27–40.
Article18. Dings PJ, Elferink MA, Strobbe LJ, de Wilt JH. The prognostic value of lymph node ratio in node-positive breast cancer: a Dutch nationwide population-based study. Ann Surg Oncol. 2013; 20:2607–2614.
Article19. Liu D, Chen Y, Deng M, Xie G, Wang J, Zhang L, et al. Lymph node ratio and breast cancer prognosis: a meta-analysis. Breast Cancer. 2014; 21:1–9.
Article20. Huang L, Liu Z, Chen S, Liu Y, Shao Z. A prognostic model for triple-negative breast cancer patients based on node status, cathepsin-D and Ki-67 index. PLoS One. 2013; 8:e83081.
Article21. Asaga S, Kinoshita T, Hojo T, Suzuki J, Jimbo K, Tsuda H. Prognostic factors for triple-negative breast cancer patients receiving preoperative systemic chemotherapy. Clin Breast Cancer. 2013; 13:40–46.
Article22. Solak M, Turkoz FP, Keskin O, Aksoy S, Babacan T, Sarici F, et al. The lymph node ratio as an independent prognostic factor for non-metastatic node-positive breast cancer recurrence and mortality. J BUON. 2015; 20:737–745.23. Yerushalmi R, Woods R, Ravdin PM, Hayes MM, Gelmon KA. Ki67 in breast cancer: prognostic and predictive potential. Lancet Oncol. 2010; 11:174–183.
Article24. Nishimura R, Osako T, Okumura Y, Hayashi M, Toyozumi Y, Arima N. Ki-67 as a prognostic marker according to breast cancer subtype and a predictor of recurrence time in primary breast cancer. Exp Ther Med. 2010; 1:747–754.
Article25. Keam B, Im SA, Lee KH, Han SW, Oh DY, Kim JH, et al. Ki-67 can be used for further classification of triple negative breast cancer into two subtypes with different response and prognosis. Breast Cancer Res. 2011; 13:R22.
Article26. Li H, Han X, Liu Y, Liu G, Dong G. Ki67 as a predictor of poor prognosis in patients with triple-negative breast cancer. Oncol Lett. 2015; 9:149–152.
Article27. Mosalpuria K. COX-2 expression in operable triple negative breast cancer: a hospital based cross-sectional study [dissertation]. [Houston, USA]: The University of Texas School of Public Health;2010.28. Kim HS, Moon HG, Han W, Yom CK, Kim WH, Kim JH, et al. COX2 overexpression is a prognostic marker for Stage III breast cancer. Breast Cancer Res Treat. 2012; 132:51–59.
Article29. Chikman B, Vasyanovich S, Lavy R, Habler L, Tolstov G, Kapiev A, et al. COX2 expression in high-grade breast cancer: evidence for prognostic significance in the subset of triple-negative breast cancer patients. Med Oncol. 2014; 31:989.
Article30. Rakha EA, Soria D, Green AR, Lemetre C, Powe DG, Nolan CC, et al. Nottingham Prognostic Index plus (NPI+): a modern clinical decision making tool in breast cancer. Br J Cancer. 2014; 110:1688–1697.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The different prognostic impact of age according to individual molecular subtypes in breast cancer
- The Nottingham and Immunohistochemical Prognostic Index in Breast Carcinomas
- Biologic subtype is a more important prognostic factor than nodal involvement in patients with stages I and II breast carcinoma
- Prognostic Influence of BCL2 on Molecular Subtypes of Breast Cancer
- Clinicopathologic Characteristics and Prognosis of Early Stage Triple Negative Breast Cancer: Comparison with Non-triple Negative Group