Ann Surg Treat Res.
2017 Mar;92(3):156-163. 10.4174/astr.2017.92.3.156.
Radiation hazards to vascular surgeon and scrub nurse in mobile fluoroscopy equipped hybrid vascular room
- Affiliations
-
- 1Division of Vascular Surgery, Department of Surgery, Catholic University of Daegu School of Medicine, Daegu, Korea. khpark@cu.ac.kr
- KMID: 2377558
- DOI: http://doi.org/10.4174/astr.2017.92.3.156
Abstract
- PURPOSE
The aim of the present study was to identify the radiation hazards to vascular surgeons and scrub nurses working in mobile fluoroscopy equipped hybrid vascular operation rooms; additionally, to estimate cumulative cancer risk due to certain exposure dosages.
METHODS
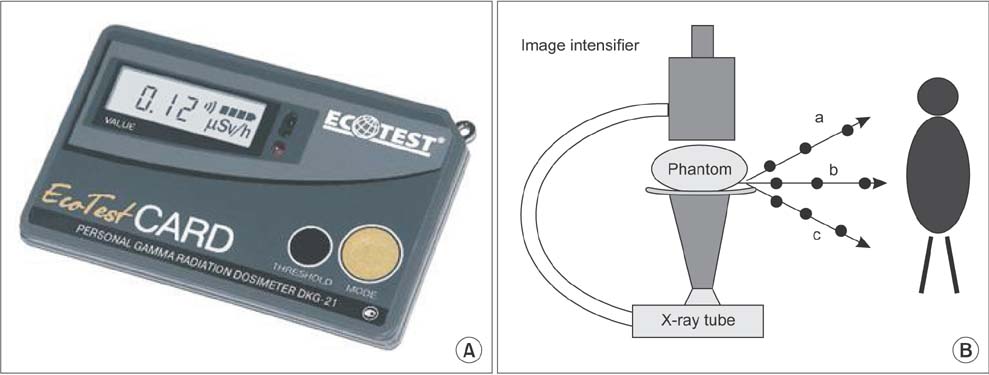
The study was conducted prospectively in 71 patients (53 men and 18 women) who had undergone vascular intervention at our hybrid vascular theater for 6 months. OEC 9900 fluoroscopy was used as mobile C-arm. Exposure dose (ED) was measured by attaching optically stimulated luminescence at in and outside of the radiation protectors. To measure X-ray scatter with the anthropomorphic phantom model, the dose was measured at 3 distances (20, 50, 100 cm) and 3 angles (horizontal, upward 45°, downward 45°) using a personal gamma radiation dosimeter, Ecotest CARD DKG-21, for 1, 3, 5, 10 minutes.
RESULTS
Lifetime attributable risk of cancer was estimated using the approach of the Biological Effects of Ionizing Radiation report VII. The 6-month ED of vascular surgeons and scrub nurses were 3.85, 1.31 mSv, respectively. The attenuation rate of lead apron, neck protector and goggle were 74.6%, 60.6%, and 70.1%, respectively. All cancer incidences among surgeons and scrub nurses correspond to 2,355 and 795 per 100,000 persons. The 10-minute dose at 100-cm distance was 0.004 mSv at horizontal, 0.009 mSv at downward 45°, 0.003 mSv at upward 45°.
CONCLUSION
Although yearly radiation hazards for vascular surgeons and scrub nurses are still within safety guidelines, protection principles can never be too stringent when aiming to minimize the cumulative harmful effects.
Keyword
MeSH Terms
Figure
Reference
-
1. Goodney PP, Beck AW, Nagle J, Welch HG, Zwolak RM. National trends in lower extremity bypass surgery, endovascular interventions, and major amputations. J Vasc Surg. 2009; 50:54–60.2. Giles KA, Pomposelli F, Hamdan A, Wyers M, Jhaveri A, Schermerhorn ML. Decrease in total aneurysm-related deaths in the era of endovascular aneurysm repair. J Vasc Surg. 2009; 49:543–550.3. Park YY, Joh JH, Han SA, Kim SH, Cho S, Park HC, et al. National trends for the treatment of peripheral arterial disease in Korea between 2004 and 2013. Ann Surg Treat Res. 2015; 89:319–324.4. Kim MS, Joo YS, Park KH. Results of simultaneous hybrid operation in multi-level arterial occlusive disease. J Korean Surg Soc. 2010; 79:386–392.5. Reed AB. Introduction. Radiation safety in vascular surgery. J Vasc Surg. 2011; 53:1 Suppl. 1S–2S.6. Bordoli SJ, Carsten CG 3rd, Cull DL, Johnson BL, Taylor SM. Radiation safety education in vascular surgery training. J Vasc Surg. 2014; 59:860–864.7. Niklason LT, Marx MV, Chan HP. The estimation of occupational effective dose in diagnostic radiology with two dosimeters. Health Phys. 1994; 67:611–615.8. Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation, Board on Radiation Effects, Research Division on Earth and Life Studies, National Research Council of the National Academies. Health risks from exposure to low levels of ionizing radiation, BEIR VII phase 2. Washington, DC: The National Academies Press;2006.9. Wrixon AD. New ICRP recommendations. J Radiol Prot. 2008; 28:161–168.10. Schanzer A, Steppacher R, Eslami M, Arous E, Messina L, Belkin M. Vascular surgery training trends from 2001-2007: A substantial increase in total procedure volume is driven by escalating endovascular procedure volume and stable open procedure volume. J Vasc Surg. 2009; 49:1339–1344.11. Wakeford R. Radiation in the workplace-a review of studies of the risks of occupational exposure to ionising radiation. J Radiol Prot. 2009; 29(2A):A61–A79.12. Greenhalgh RM, Brown LC, Kwong GP, Powell JT, Thompson SG. EVAR trial participants. Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomised controlled trial. Lancet. 2004; 364:843–848.13. Bannazadeh M, Altinel O, Kashyap VS, Sun Z, Clair D, Sarac TP. Patterns of procedure-specific radiation exposure in the endovascular era: impetus for further innovation. J Vasc Surg. 2009; 49:1520–1524.14. Ho P, Cheng SW, Wu PM, Ting AC, Poon JT, Cheng CK, et al. Ionizing radiation absorption of vascular surgeons during endovascular procedures. J Vasc Surg. 2007; 46:455–459.15. Lipsitz EC, Veith FJ, Ohki T, Heller S, Wain RA, Suggs WD, et al. Does the endovascular repair of aortoiliac aneurysms pose a radiation safety hazard to vascular surgeons? J Vasc Surg. 2000; 32:704–710.16. Venneri L, Rossi F, Botto N, Andreassi MG, Salcone N, Emad A, et al. Cancer risk from professional exposure in staff working in cardiac catheterization laboratory: insights from the National Research Council's Biological Effects of Ionizing Radiation VII Report. Am Heart J. 2009; 157:118–124.17. Scott DF. A study of logger fatalities from 1992-2000. Inj Prev. 2004; 10:239–243.18. Brown KR, Rzucidlo E. Acute and chronic radiation injury. J Vasc Surg. 2011; 53:1 Suppl. 15S–21S.19. ICRP Publication 60: 1990 Recommendations of the International Commission on Radiological Protection. Oxford: Pergamon Press;1991.20. Haskal ZJ. Interventional radiology carries occupational risk for cataracts. RSNA News. 2004; 14:5–6.21. Vano E, Gonzalez L, Beneytez F, Moreno F. Lens injuries induced by occupational exposure in non-optimized interventional radiology laboratories. Br J Radiol. 1998; 71:728–733.22. Johnson DR, Kyriou J, Morton EJ, Clifton A, Fitzgerald M, Macsweeney E. Radiation protection in interventional radiology. Clin Radiol. 2001; 56:99–106.23. Amis ES Jr, Butler PF, Applegate KE, Birnbaum SB, Brateman LF, Hevezi JM, et al. American College of Radiology white paper on radiation dose in medicine. J Am Coll Radiol. 2007; 4:272–284.24. Limacher MC, Douglas PS, Germano G, Laskey WK, Lindsay BD, McKetty MH, et al. ACC expert consensus document. Radiation safety in the practice of cardiology. American College of Cardiology. J Am Coll Cardiol. 1998; 31:892–913.25. Fossaceca R, Brambilla M, Guzzardi G, Cerini P, Renghi A, Valzano S, et al. The impact of radiological equipment on patient radiation exposure during endovascular aortic aneurysm repair. Eur Radiol. 2012; 22:2424–2431.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pattern and degree of radiation exposure during endovascular surgery performed using a mobile C-arm or in a hybrid room
- Endovascular Intervention with a Mobile C-Arm in the Operating Room
- Radiation Exposure from Fluoroscopy during Orthopaedic Surgical Procedures
- Radiation Exposure Over the Course of a Year from an Image Intensifier in the Orthopaedic Operating Room
- Results of Simultaneous Hybrid Operation in Multi-level Arterial Occlusive Disease