J Korean Soc Radiol.
2017 May;76(5):303-309. 10.3348/jksr.2017.76.5.303.
Ultrasound-Guided Percutaneous Core Needle Biopsy of Splenic Lesions
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. cjimage@amc.seoul.kr
- KMID: 2377031
- DOI: http://doi.org/10.3348/jksr.2017.76.5.303
Abstract
- PURPOSE
To evaluate the safety and efficacy of ultrasound-guided percutaneous core needle biopsy of splenic lesions.
MATERIALS AND METHODS
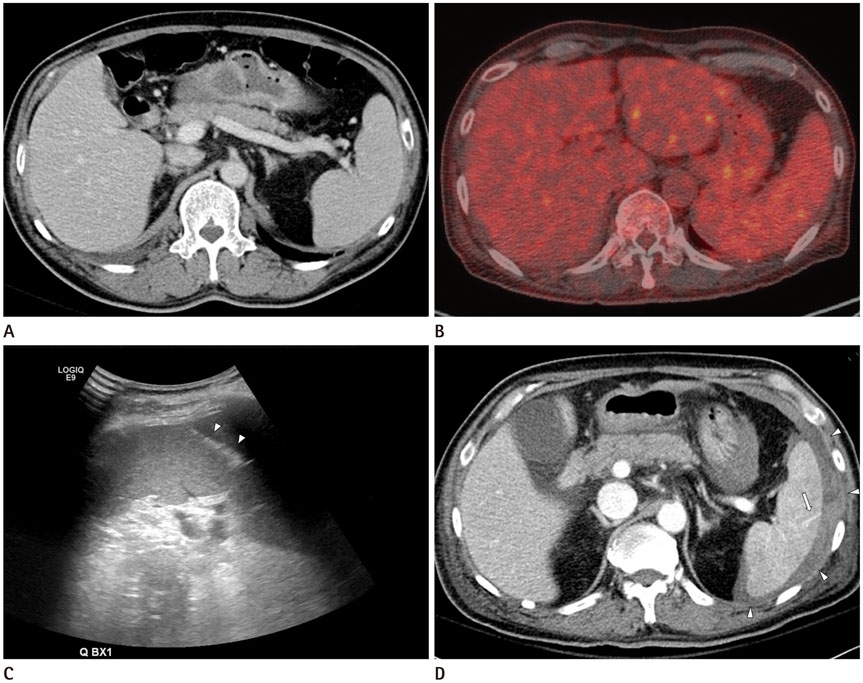
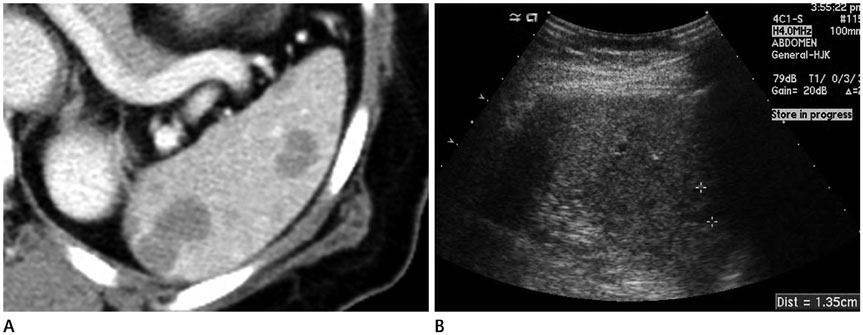
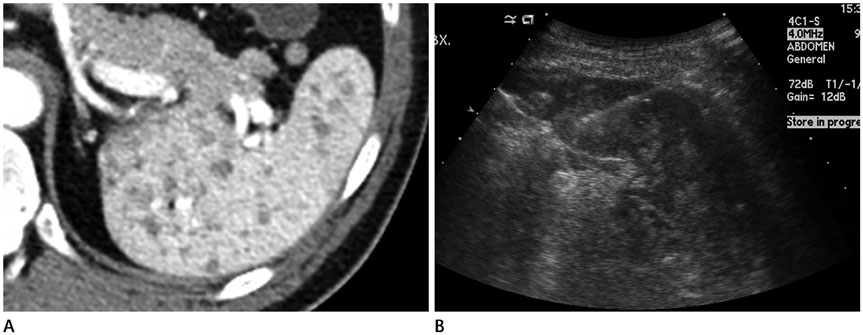
This retrospective study included 30 patients who underwent percutaneous core needle biopsy of their splenic lesions using 18- or 20-gauge needles between January 2001 and July 2016 in a single tertiary care center. The characteristics of the splenic lesions were determined by reviewing the ultrasound and computed tomography examinations. Acquisition rate and diagnostic accuracy were calculated, using pathologic results of the splenectomy specimen, clinical course and/or imaging follow-up as a reference standard. Post-procedure complications were identified from electronic medical records, laboratory findings and computed tomography images. Seventy-three specimens were obtained from the 30 patients and splenectomy was performed in 2 patients.
RESULTS
Twenty-nine of the 30 patients had focal splenic lesions, while the remaining patient had homogeneous splenomegaly. Acquisition rate and diagnostic accuracy were 80.0% (24/30) and 76.7% (23/30), respectively. Perisplenic hemorrhage without hemodynamic instability developed in one patient.
CONCLUSION
Ultrasound-guided percutaneous core needle biopsy of splenic lesions is a safe method for achieving a histopathologic diagnosis and can be considered as an alternative to splenectomy in patients with a high risk of splenectomy-related complications.
MeSH Terms
Figure
Reference
-
1. Compérat E, Bardier-Dupas A, Camparo P, Capron F, Charlotte F. Splenic metastases: clinicopathologic presentation, differential diagnosis, and pathogenesis. Arch Pathol Lab Med. 2007; 131:965–969.2. Cadili A, de Gara C. Complications of splenectomy. Am J Med. 2008; 121:371–375.3. Lehne G, Hannisdal E, Langholm R, Nome O. A 10-year experience with splenectomy in patients with malignant non-Hodgkin's lymphoma at the Norwegian Radium Hospital. Cancer. 1994; 74:933–939.4. Machado NO, Grant CS, Alkindi S, Daar S, Al-Kindy N, Al Lamki Z, et al. Splenectomy for haematological disorders: a single center study in 150 patients from Oman. Int J Surg. 2009; 7:476–481.5. Keogan MT, Freed KS, Paulson EK, Nelson RC, Dodd LG. Imaging-guided percutaneous biopsy of focal splenic lesions: update on safety and effectiveness. AJR Am J Roentgenol. 1999; 172:933–937.6. Quinn SF, vanSonnenberg E, Casola G, Wittich GR, Neff CC. Interventional radiology in the spleen. Radiology. 1986; 161:289–291.7. Solbiati L, Bossi MC, Bellotti E, Ravetto C, Montali G. Focal lesions in the spleen: sonographic patterns and guided biopsy. AJR Am J Roentgenol. 1983; 140:59–65.8. Gómez-Rubio M, López-Cano A, Rendón P, Muñoz-Benvenuty A, Macías M, Garre C, et al. Safety and diagnostic accuracy of percutaneous ultrasound-guided biopsy of the spleen: a multicenter study. J Clin Ultrasound. 2009; 37:445–450.9. Lieberman S, Libson E, Maly B, Lebensart P, Ben-Yehuda D, Bloom AI. Imaging-guided percutaneous splenic biopsy using a 20- or 22-gauge cutting-edge core biopsy needle for the diagnosis of malignant lymphoma. AJR Am J Roentgenol. 2003; 181:1025–1027.10. Muraca S, Chait PG, Connolly BL, Baskin KM, Temple MJ. US-guided core biopsy of the spleen in children. Radiology. 2001; 218:200–206.11. Venkataramu NK, Gupta S, Sood BP, Gulati M, Rajawanshi A, Gupta SK, et al. Ultrasound guided fine needle aspiration biopsy of splenic lesions. Br J Radiol. 1999; 72:953–956.12. Olson MC, Atwell TD, Harmsen WS, Konrad A, King RL, Lin Y, et al. Safety and accuracy of percutaneous image-guided core biopsy of the spleen. AJR Am J Roentgenol. 2016; 206:655–659.13. McInnes MD, Kielar AZ, Macdonald DB. Percutaneous image-guided biopsy of the spleen: systematic review and meta-analysis of the complication rate and diagnostic accuracy. Radiology. 2011; 260:699–708.14. Liang P, Gao Y, Wang Y, Yu X, Yu D, Dong B. US-guided percutaneous needle biopsy of the spleen using 18-gauge versus 21-gauge needles. J Clin Ultrasound. 2007; 35:477–482.15. Patel N, Dawe G, Tung K. Ultrasound-guided percutaneous splenic biopsy using an 18-G core biopsy needle: our experience with 52 cases. Br J Radiol. 2015; 88:20150400.16. Civardi G, Vallisa D, Bertè R, Giorgio A, Filice C, Caremani M, et al. Ultrasound-guided fine needle biopsy of the spleen: high clinical efficacy and low risk in a multicenter Italian study. Am J Hematol. 2001; 67:93–99.17. Kim SH, Min YI, Lee IC, Lee MG, Auh YH, Hyun CD. Fine-needle aspiration of splenic lesions. J Korean Radiol Soc. 1994; 31:921–924.18. Lindgren PG, Hagberg H, Eriksson B, Glimelius B, Magnusson A, Sundström C. Excision biopsy of the spleen by ultrasonic guidance. Br J Radiol. 1985; 58:853–857.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of Ultrasound-Guided Automated Core Biopsy of Nonpalpable Breast Lesions
- Breast Lesions with Discordant Results on Ultrasound-guided Core Needle Biopsy
- Endoscopic Ultrasound-Fine Needle Aspiration versus Core Biopsy for the Diagnosis of Subepithelial Tumors
- Clinical Application of Ultrasound-guided Core Needle Biopsy of the Breast
- Fine-Needle Biopsy: Should This Be the First Choice in Endoscopic Ultrasound-Guided Tissue Acquisition?