J Korean Soc Transplant.
2017 Mar;31(1):25-33. 10.4285/jkstn.2017.31.1.25.
Non-invasive Myocardial Strain Imaging to Evaluate Graft Failure in Cardiac Xenotransplantation
- Affiliations
-
- 1Department of Cardiology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 2Department of Thoracic and Cardiovascular Surgery, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 3Department of Pathology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 4Department of Nephrology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 5Department of Ophthalmology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 6Department of Surgery, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea. ijyun@kuh.ac.kr
- 7Haeen Biomedical Research Institute, Genia Inc., Seongnam, Korea.
- 8Animal Biotechnology Division, National Institute of Animal Science, Suwon, Korea.
- 9Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2375677
- DOI: http://doi.org/10.4285/jkstn.2017.31.1.25
Abstract
- BACKGROUND
The shortage of human hearts for allotransplantation makes xenotransplantation a possible option for controllable organ providers. To detect acute xenograft rejection, invasive biopsy seems inevitable; however, this occasionally results in poor incision wound healing or infection. To date, no method of noninvasive imaging for early detection of xenograft rejection has been established. We hypothesized that ultrasound speckle tracking would better detect xenograft failure than routine left ventricular ejection fractions (EF).
METHODS
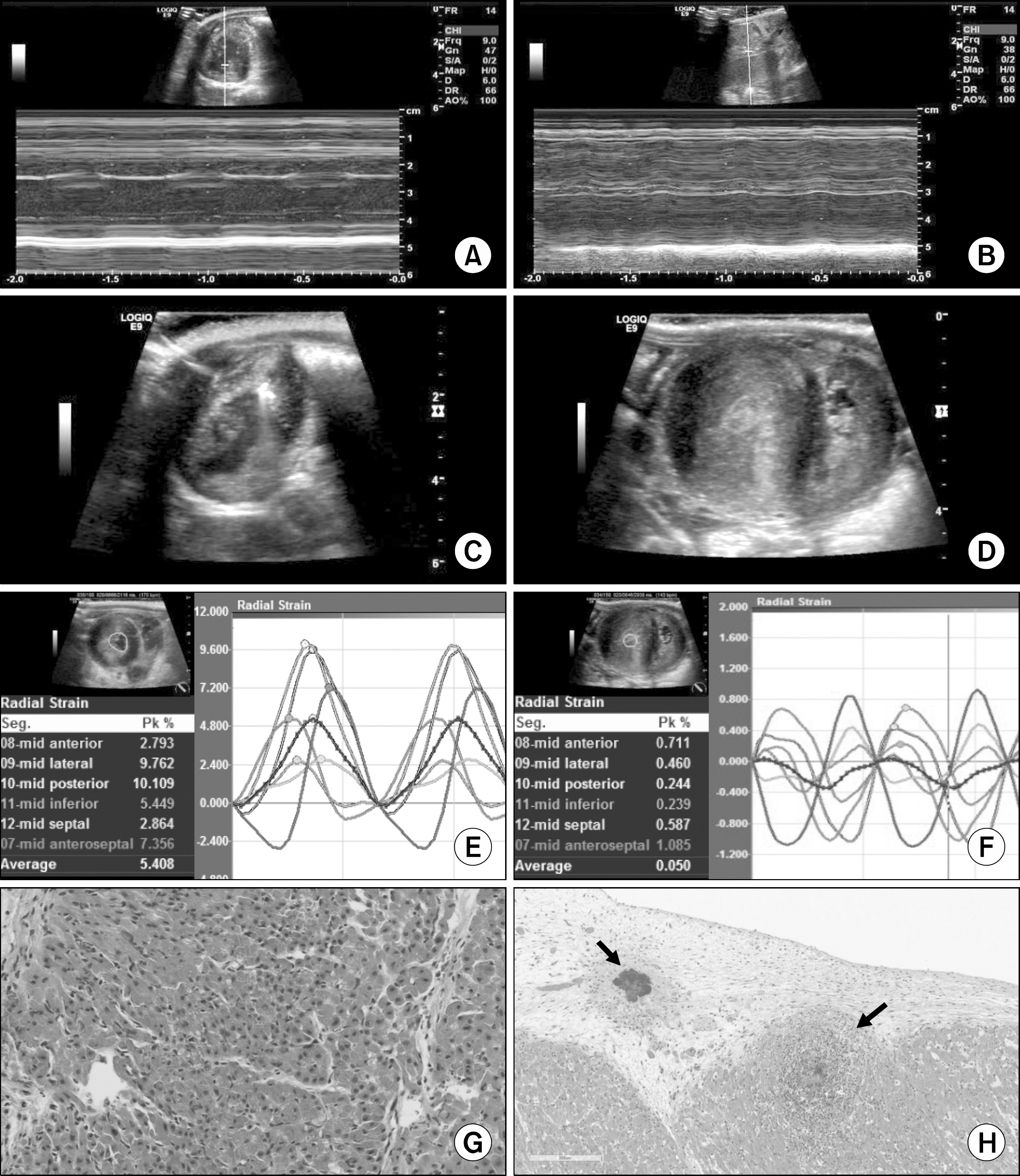
From August 2013 to July 2015, a total of six cardiac heterotopic xenotransplants (α 1, 3-galactosyltransferase gene-knockout porcine heart) into cynomolgus monkeys were monitored with echocardiography every 3 to 7 days. M-mode and two-dimensional (2D)-EF measurements and myocardial strain analyses were performed. Cardiac xenograft pathology was reviewed from the immediate postoperative biopsy, as well as the necropsy.
RESULTS
Myocardial speckle tracking analysis was feasible in all six cases. The longest survival was 43 days. Only one pathology-proven immunologic rejection occurred. Cardiac xenograft failure appeared as two types: a dilated pattern with decreased EF or a myocardial-thickening pattern with preserved EF. Both antibody-mediated rejection (n=1) and sepsis-induced myocardial dysfunction (n=2) revealed decreased radial or circumferential strains, but normal-range EF. Xenograft functional decline was significant with respect to radial or circumferential strain (P=0.028), but not to conventional M-mode or 2D-EFs (P=0.600, P=0.340, respectively).
CONCLUSIONS
Radial and circumferential strains were significantly decreased in both types of xenograft failure, regardless of EF. Further studies are warranted to correlate the strain analysis and immunopathological details.
MeSH Terms
Figure
Reference
-
1). Kuwaki K., Tseng YL., Dor FJ., Shimizu A., Houser SL., Sanderson TM, et al. Heart transplantation in baboons using alpha1,3-galactosyltransferase gene-knockout pigs as donors: initial experience. Nat Med. 2005. 11:29–31.2). Mohiuddin MM., Corcoran PC., Singh AK., Azimzadeh A., Hoyt RF Jr., Thomas ML, et al. B-cell depletion extends the survival of GTKO.hCD46Tg pig heart xenografts in baboons for up to 8 months. Am J Transplant. 2012. 12:763–71.3). Mohiuddin MM., Singh AK., Corcoran PC., Hoyt RF., Thomas ML 3rd., Ayares D, et al. Genetically engineered pigs and target-specific immunomodulation provide significant graft survival and hope for clinical cardiac xenotransplantation. J Thorac Cardiovasc Surg. 2014. 148:1106–13.
Article4). Ferferieva V., Van den Bergh A., Claus P., Jasaityte R., La Gerche A., Rademakers F, et al. Assessment of strain and strain rate by two-dimensional speckle tracking in mice: comparison with tissue Doppler echocardiography and conductance catheter measurements. Eur Heart J Cardiovasc Imaging. 2013. 14:765–73.
Article5). Shi J., Pan C., Shu X., Sun M., Yang Z., Zhu S, et al. The role of speckle tracking imaging in the noninvasive detection of acute rejection after heterotopic cardiac transplantation in rats. Acta Cardiol. 2011. 66:779–85.
Article6). Pieper GM., Shah A., Harmann L., Cooley BC., Ionova IA., Migrino RQ. Speckle-tracking 2-dimensional strain echocardiography: a new noninvasive imaging tool to evaluate acute rejection in cardiac transplantation. J Heart Lung Transplant. 2010. 29:1039–46.
Article7). Mingo-Santos S., Monivas-Palomero V., Garcia-Lunar I., Mitroi CD., Goirigolzarri-Artaza J., Rivero B, et al. Usefulness of two-dimensional strain parameters to diagnose acute rejection after heart transplantation. J Am Soc Echocardiogr. 2015. 28:1149–56.8). Ambardekar AV., Alluri N., Patel AC., Lindenfeld J., Dorosz JL. Myocardial strain and strain rate from speckle-tracking echocardiography are unable to differentiate asymptomatic biopsy-proven cellular rejection in the first year after cardiac transplantation. J Am Soc Echocardiogr. 2015. 28:478–85.
Article9). Kim H., Chee HK., Yang J., Hwang S., Han KH., Kang J, et al. Outcomes of alpha 1,3-GT-knockout porcine heart transplants into a preclinical nonhuman primate model. Transplant Proc. 2013. 45:3085–91.
Article10). Mohiuddin MM., Reichart B., Byrne GW., McGregor CG. Current status of pig heart xenotransplantation. Int J Surg. 2015. 23(Pt B):234–9.
Article11). Stewart S., Winters GL., Fishbein MC., Tazelaar HD., Kobashi-gawa J., Abrams J, et al. Revision of the 1990 working formulation for the standardization of nomenclature in the diagnosis of heart rejection. J Heart Lung Transplant. 2005. 24:1710–20.
Article12). Behr TM., Feucht HE., Richter K., Reiter C., Spes CH., Pongratz D, et al. Detection of humoral rejection in human cardiac allografts by assessing the capillary deposition of complement fragment C4d in endomyocardial biopsies. J Heart Lung Transplant. 1999. 18:904–12.
Article13). Lang RM., Badano LP., Mor-Avi V., Afilalo J., Armstrong A., Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015. 28:1–39. .e14.
Article14). Devereux RB., Alonso DR., Lutas EM., Gottlieb GJ., Campo E., Sachs I, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986. 57:450–8.
Article15). Cameli M., Mondillo S., Solari M., Righini FM., Andrei V., Contaldi C, et al. Echocardiographic assessment of left ventricular systolic function: from ejection fraction to torsion. Heart Fail Rev. 2016. 21:77–94.
Article16). Abbott CP., Dewitt CW., Creech O Jr. The transplanted rat heart: histologic and electrocardiographic changes. Transplantation. 1965. 3:432–45.17). Chen RH., Kadner A., Adams DH. Monitoring pig-to-primate cardiac xenografts with live Internet images of recipients and xenograft telemetric signals: histologic and immunohistochemical correlations. J Heart Lung Transplant. 2000. 19:591–7.
Article18). Horvath KA., Corcoran PC., Singh AK., Hoyt RF., Carrier C., Thomas ML 3rd, et al. Left ventricular pressure measurement by telemetry is an effective means to evaluate transplanted heart function in experimental heterotopic cardiac xenotransplantation. Transplant Proc. 2010. 42:2152–5.
Article19). Zhou M., Hara H., Dai Y., Mou L., Cooper DK., Wu C, et al. Circulating organ-specific microRNAs serve as biomarkers in organ-specific diseases: implications for organ allo- and xeno-transplantation. Int J Mol Sci. 2016. 17:E1232.
Article20). Badano LP., Miglioranza MH., Edvardsen T., Colafranceschi AS., Muraru D., Bacal F, et al. European Association of Cardiovascular Imaging/Cardiovascular Imaging Department of the Brazilian Society of Cardiology recommendations for the use of cardiac imaging to assess and follow patients after heart transplantation. Eur Heart J Cardiovasc Imaging. 2015. 16:919–48.
Article21). Abicht JM., Mayr T., Reichart B., Buchholz S., Werner F., Lutzmann I, et al. Pre-clinical heterotopic intrathoracic heart xenotransplantation: a possibly useful clinical technique. Xenotransplantation. 2015. 22:427–42.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiac Strain Analysis Using Cine Magnetic Resonance Imaging and Computed Tomography
- Principles and Clinical Applications of Feature-Tracking Cardiac Magnetic Resonance Imaging: A Literature Review
- Role of cardiac imaging in management of heart failure
- Correlation Between Functional Myocardial Perfusion Imaging and Anatomical Cardiac CT in a Case of Myocardial Bridging
- Role of strain echocardiography in patients with hypertension