J Breast Cancer.
2013 Mar;16(1):55-59.
Usefulness of Pretreatment Neutrophil to Lymphocyte Ratio in Predicting Disease-Specific Survival in Breast Cancer Patients
- Affiliations
-
- 1Department of Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea. airihan@yonsei.ac.kr
- 2Department of Pathology, Yonsei University Wonju College of Medicine, Wonju, Korea.
Abstract
- PURPOSE
The purpose of this study was to investigate the prognostic impact of pretreatment neutrophil to lymphocyte ratio (NLR) on breast cancer in view of disease-specific survival and the intrinsic subtype.
METHODS
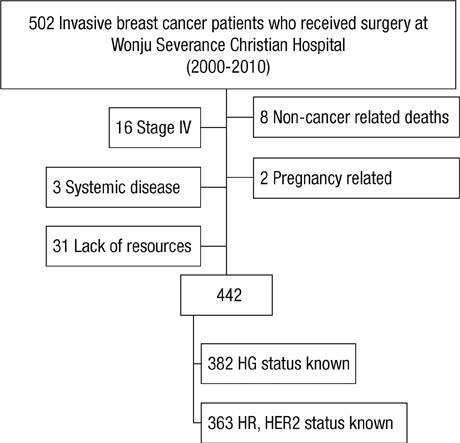
We retrospectively studied patients diagnosed with primary breast cancer that had completed all phases of primary treatment from 2000 to 2010. The association between pretreatment NLR and disease-specific survival was analyzed.
RESULTS
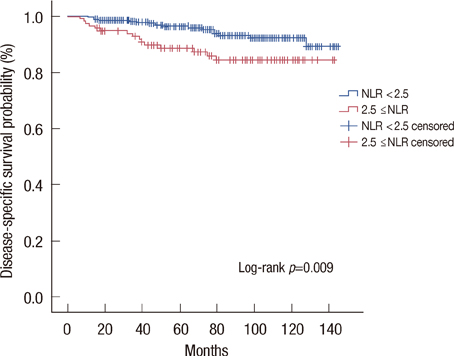
A total of 442 patients were eligible for analysis. Patients with higher NLR (2.5 < or =NLR) showed significantly lower disease-specific survival rate than those with lower NLR (NLR <2.5). Higher NLR along with negative estrogen receptor status and positive nodal status were independently correlated with poor prognosis, with hazard ratio 4.08 (95% confidence interval [CI], 1.62-10.28), 9.93 (95% CI, 3.51-28.13), and 11.23 (95% CI, 3.34-37.83), respectively. Luminal A subtype was the only intrinsic subtype in which higher NLR patients showed significantly poor prognosis (87.7% vs. 96.7%, p=0.009).
CONCLUSION
Patients with an elevated pretreatment NLR showed poorer disease-specific survival than patients without elevated NLR, most evident in the luminal A subtype. Further validation and a feasibility study are required before it can be considered for clinical use.
Keyword
MeSH Terms
Figure
Reference
-
1. Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000. 406:747–752.
Article2. Saez RA, McGuire WL, Clark GM. Prognostic factors in breast cancer. Semin Surg Oncol. 1989. 5:102–110.
Article3. Fisher B, Bauer M, Wickerham DL, Redmond CK, Fisher ER, Cruz AB, et al. Relation of number of positive axillary nodes to the prognosis of patients with primary breast cancer. An NSABP update. Cancer. 1983. 52:1551–1557.
Article4. Hassett MJ, Silver SM, Hughes ME, Blayney DW, Edge SB, Herman JG, et al. Adoption of gene expression profile testing and association with use of chemotherapy among women with breast cancer. J Clin Oncol. 2012. 30:2218–2226.
Article5. Balkwill FR, Mantovani A. Cancer-related inflammation: common themes and therapeutic opportunities. Semin Cancer Biol. 2012. 22:33–40.
Article6. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008. 454:436–444.
Article7. Aizawa M, Gotohda N, Takahashi S, Konishi M, Kinoshita T. Predictive value of baseline neutrophil/lymphocyte ratio for T4 disease in wall-penetrating gastric cancer. World J Surg. 2011. 35:2717–2722.
Article8. Halazun KJ, Hardy MA, Rana AA, Woodland DC 4th, Luyten EJ, Mahadev S, et al. Negative impact of neutrophil-lymphocyte ratio on outcome after liver transplantation for hepatocellular carcinoma. Ann Surg. 2009. 250:141–151.
Article9. Bhatti I, Peacock O, Lloyd G, Larvin M, Hall RI. Preoperative hematologic markers as independent predictors of prognosis in resected pancreatic ductal adenocarcinoma: neutrophil-lymphocyte versus platelet-lymphocyte ratio. Am J Surg. 2010. 200:197–203.
Article10. Tomita M, Shimizu T, Ayabe T, Yonei A, Onitsuka T. Preoperative neutrophil to lymphocyte ratio as a prognostic predictor after curative resection for non-small cell lung cancer. Anticancer Res. 2011. 31:2995–2998.11. Lee YY, Choi CH, Kim HJ, Kim TJ, Lee JW, Lee JH, et al. Pretreatment neutrophil:lymphocyte ratio as a prognostic factor in cervical carcinoma. Anticancer Res. 2012. 32:1555–1561.12. Yamanaka T, Matsumoto S, Teramukai S, Ishiwata R, Nagai Y, Fukushima M. The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology. 2007. 73:215–220.
Article13. Azab B, Bhatt VR, Phookan J, Murukutla S, Kohn N, Terjanian T, et al. Usefulness of the neutrophil-to-lymphocyte ratio in predicting short- and long-term mortality in breast cancer patients. Ann Surg Oncol. 2012. 19:217–224.
Article14. Fogar P, Sperti C, Basso D, Sanzari MC, Greco E, Davoli C, et al. Decreased total lymphocyte counts in pancreatic cancer: an index of adverse outcome. Pancreas. 2006. 32:22–28.
Article15. Sarraf KM, Belcher E, Raevsky E, Nicholson AG, Goldstraw P, Lim E. Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J Thorac Cardiovasc Surg. 2009. 137:425–428.
Article16. Eroles P, Bosch A, Pérez-Fidalgo JA, Lluch A. Molecular biology in breast cancer: intrinsic subtypes and signaling pathways. Cancer Treat Rev. 2012. 38:698–707.
Article17. Parker JS, Mullins M, Cheang MC, Leung S, Voduc D, Vickery T, et al. Supervised risk predictor of breast cancer based on intrinsic subtypes. J Clin Oncol. 2009. 27:1160–1167.
Article18. Kennecke H, Yerushalmi R, Woods R, Cheang MC, Voduc D, Speers CH, et al. Metastatic behavior of breast cancer subtypes. J Clin Oncol. 2010. 28:3271–3277.19. Place AE, Jin Huh S, Polyak K. The microenvironment in breast cancer progression: biology and implications for treatment. Breast Cancer Res. 2011. 13:227.
Article20. Chlebowski RT, Anderson GL, Gass M, Lane DS, Aragaki AK, Kuller LH, et al. Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA. 2010. 304:1684–1692.
Article21. Collaborative Group on Hormonal Factors in Breast Cancer. Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer. Lancet. 1997. 350:1047–1059.22. Feigelson HS, Jonas CR, Teras LR, Thun MJ, Calle EE. Weight gain, body mass index, hormone replacement therapy, and postmenopausal breast cancer in a large prospective study. Cancer Epidemiol Biomarkers Prev. 2004. 13:220–224.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Can pretreatment platelet-to-lymphocyte and neutrophil-to-lymphocyte ratios predict long-term oncologic outcomes after preoperative chemoradiation followed by surgery for locally advanced rectal cancer?
- Clinical Significance of Preoperative Inflammatory Parameters in Gastric Cancer Patients
- Pretreatment inflammatory markers predicting treatment outcomes in colorectal cancer
- Neutrophil to Lymphocyte Ratio May Predict Mortality in Breast Cancer Patients
- The Role of Neutrophil-lymphocyte Ratio and Platelet-lymphocyte Ratio in Predicting Neoadjuvant Chemotherapy Response in Breast Cancer