Korean J Ophthalmol.
2017 Apr;31(2):123-131. 10.3341/kjo.2017.31.2.123.
Oral Administration of Cilostazol Increases Ocular Blood Flow in Patients with Diabetic Retinopathy
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. hgonyu@snu.ac.kr
- 2HanGil Eye Hospital, Incheon, Korea.
- KMID: 2373468
- DOI: http://doi.org/10.3341/kjo.2017.31.2.123
Abstract
- PURPOSE
To investigate the effect of cilostazol on ocular hemodynamics and to determine whether the administration of cilostazol increases the ocular blood flow in patients with diabetic retinopathy.
METHODS
This prospective observational study investigated the effect of orally administered cilostazol on diabetic retinopathy. Before and after administration for 1 week, pulsatile ocular blood flow (POBF) and retrobulbar hemodynamics were measured using a POBF analyzer and transcranial Doppler imaging, respectively. Visual acuity, intraocular pressure, and blood pressure were also evaluated before and after treatment.
RESULTS
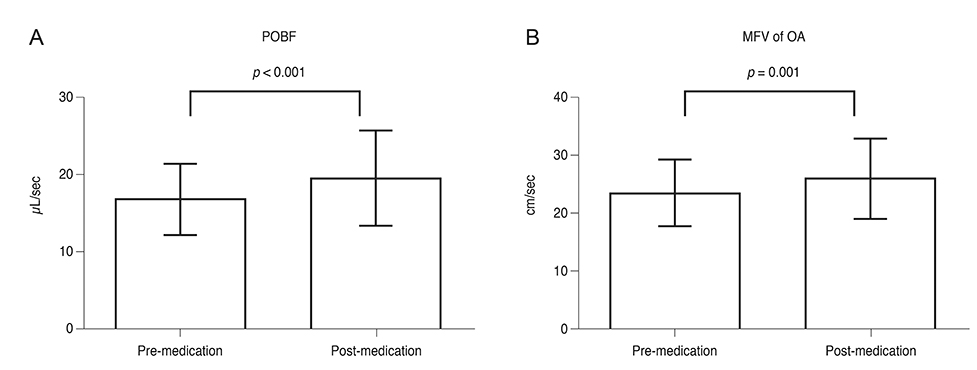
Twenty-five eyes of 25 patients were included in this study. POBF increased significantly (16.8 ± 4.6 µL/sec vs. 19.6 ± 6.2 µL/sec, p < 0.001) after administration of cilostazol, while no significant change was identified in visual acuity, intraocular pressure, and blood pressure. Mean flow velocity in the ophthalmic artery as measured with transcranial Doppler imaging also increased significantly after medication (23.5 ± 5.6 cm/sec vs. 26.0 ± 6.9 cm/sec, p = 0.001). The change in POBF directly correlated with the change in mean flow velocity (r = 0.419, p = 0.007).
CONCLUSIONS
Cilostazol was effective in increasing ocular blood flow in patients with diabetic retinopathy, possibly by modulating retrobulbar circulation.
MeSH Terms
Figure
Reference
-
1. Patton N, Aslam T, Macgillivray T, et al. Retinal vascular image analysis as a potential screening tool for cerebrovascular disease: a rationale based on homology between cerebral and retinal microvasculatures. J Anat. 2005; 206:319–348.2. Delaey C, Van De Voorde J. Regulatory mechanisms in the retinal and choroidal circulation. Ophthalmic Res. 2000; 32:249–256.3. Li G, Shih YY, Kiel JW, et al. MRI study of cerebral, retinal and choroidal blood flow responses to acute hypertension. Exp Eye Res. 2013; 112:118–124.4. Yoshida Y, Sugiyama T, Utsunomiya K, et al. A pilot study for the effects of donepezil therapy on cerebral and optic nerve head blood flow, visual field defect in normal-tension glaucoma. J Ocul Pharmacol Ther. 2010; 26:187–192.5. Uchiyama S, Demaerschalk BM, Goto S, et al. Stroke prevention by cilostazol in patients with atherothrombosis: meta-analysis of placebo-controlled randomized trials. J Stroke Cerebrovasc Dis. 2009; 18:482–490.6. Goto S. Cilostazol: potential mechanism of action for antithrombotic effects accompanied by a low rate of bleeding. Atheroscler Suppl. 2005; 6:3–11.7. Tanaka T, Ishikawa T, Hagiwara M, et al. Effects of cilostazol, a selective cAMP phosphodiesterase inhibitor on the contraction of vascular smooth muscle. Pharmacology. 1988; 36:313–320.8. Schror K. The pharmacology of cilostazol. Diabetes Obes Metab. 2002; 4:Suppl 2. S14–S19.9. Langham ME, Farrell RA, O'Brien V, et al. Blood flow in the human eye. Acta Ophthalmol Suppl. 1989; 191:9–13.10. Silver DM, Farrell RA, Langham ME, et al. Estimation of pulsatile ocular blood flow from intraocular pressure. Acta Ophthalmol Suppl. 1989; 191:25–29.11. Krakau CE. Calculation of the pulsatile ocular blood flow. Invest Ophthalmol Vis Sci. 1992; 33:2754–2756.12. Sakata K, Funatsu H, Harino S, et al. Relationship between macular microcirculation and progression of diabetic macular edema. Ophthalmology. 2006; 113:1385–1391.13. Mendivil A, Cuartero V, Mendivil MP. Ocular blood flow velocities in patients with proliferative diabetic retinopathy and healthy volunteers: a prospective study. Br J Ophthalmol. 1995; 79:413–416.14. Cuypers MH, Kasanardjo JS, Polak BC. Retinal blood flow changes in diabetic retinopathy measured with the Heidelberg scanning laser Doppler flowmeter. Graefes Arch Clin Exp Ophthalmol. 2000; 238:935–941.15. Aiello LP, Gardner TW, King GL, et al. Diabetic retinopathy. Diabetes Care. 1998; 21:143–156.16. Bursell SE, Clermont AC, Kinsley BT, et al. Retinal blood flow changes in patients with insulin-dependent diabetes mellitus and no diabetic retinopathy. Invest Ophthalmol Vis Sci. 1996; 37:886–897.17. Feke GT, Tagawa H, Yoshida A, et al. Retinal circulatory changes related to retinopathy progression in insulin-dependent diabetes mellitus. Ophthalmology. 1985; 92:1517–1522.18. Geyer O, Neudorfer M, Snir T, et al. Pulsatile ocular blood flow in diabetic retinopathy. Acta Ophthalmol Scand. 1999; 77:522–525.19. Savage HI, Hendrix JW, Peterson DC, et al. Differences in pulsatile ocular blood flow among three classifications of diabetic retinopathy. Invest Ophthalmol Vis Sci. 2004; 45:4504–4509.20. Campochiaro PA. C99-PKC412-003 Study Group. Reduction of diabetic macular edema by oral administration of the kinase inhibitor PKC412. Invest Ophthalmol Vis Sci. 2004; 45:922–931.21. Aiello LP, Cahill MT, Cavallerano JD. Growth factors and protein kinase C inhibitors as novel therapies for the medical management diabetic retinopathy. Eye (Lond). 2004; 18:117–125.22. Yokota T, Ma RC, Park JY, et al. Role of protein kinase C on the expression of platelet-derived growth factor and endothelin-1 in the retina of diabetic rats and cultured retinal capillary pericytes. Diabetes. 2003; 52:838–845.23. Butt Z, O'brien C. Reproducibility of pulsatile ocular blood flow measurements. J Glaucoma. 1995; 4:214–218.24. Morgan A, Hosking S. Ocular blood flow tonometer reproducibility: the effect of operator experience and mode of application. Ophthalmic Physiol Opt. 2001; 21:401–406.25. Baxter GM, Williamson TH. Color Doppler imaging of the eye: normal ranges, reproducibility, and observer variation. J Ultrasound Med. 1995; 14:91–96.26. Schmetterer L, Dallinger S, Findl O, et al. Noninvasive investigations of the normal ocular circulation in humans. Invest Ophthalmol Vis Sci. 1998; 39:1210–1220.27. Aydin A, Wollstein G, Price LL, Schuman JS. Evaluating pulsatile ocular blood flow analysis in normal and treated glaucomatous eyes. Am J Ophthalmol. 2003; 136:448–453.28. Gekkieva M, Orgul S, Gherghel D, et al. The influence of sex difference in measurements with the Langham ocular blood flow system. Jpn J Ophthalmol. 2001; 45:528–532.29. Hayreh SS. The ophthalmic artery: III. branches. Br J Ophthalmol. 1962; 46:212–247.30. Perrott RL, Drasdo N, Owens DR, North RV. Can pulsatile ocular blood flow distinguish between patients with and without diabetic retinopathy? Clin Exp Optom. 2007; 90:445–450.31. Kim SH, Chang HW, Choi TH, et al. Cilostazol effectively reduces the decrease of flow volume in a thrombotic anastomosis model in a rat: a novel application of ultrasonography for evaluation. Ann Plast Surg. 2010; 64:482–486.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Macular Blood Flows in Diabetic Patients
- The Effect of Oral Calcium Channel Blockers on the Ocular Blood Flow
- The Change of Tear Film in Classification of Diabetic Retinopathy
- The Influence of Axial Myopia on Diabetic Retinopathy
- Changes in Cutaneous Blood Flow in Type 2 Diabetics with or without Neuropathy and Retinopathy