J Korean Orthop Assoc.
2017 Feb;52(1):73-82. 10.4055/jkoa.2017.52.1.73.
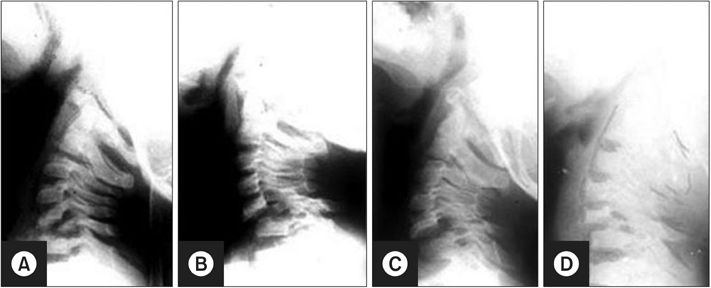
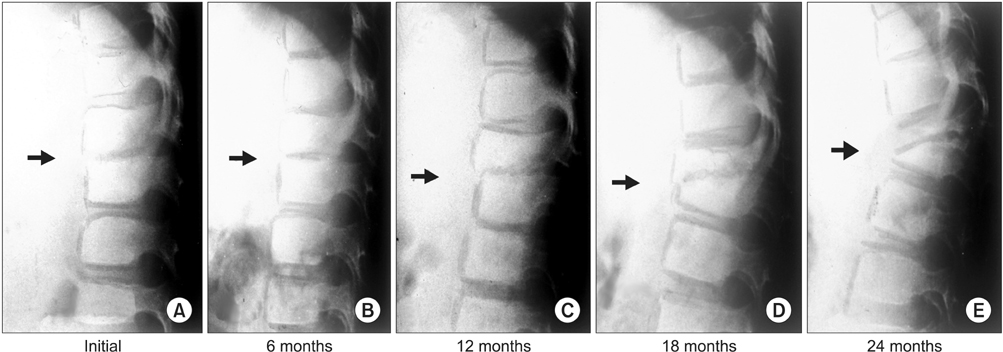
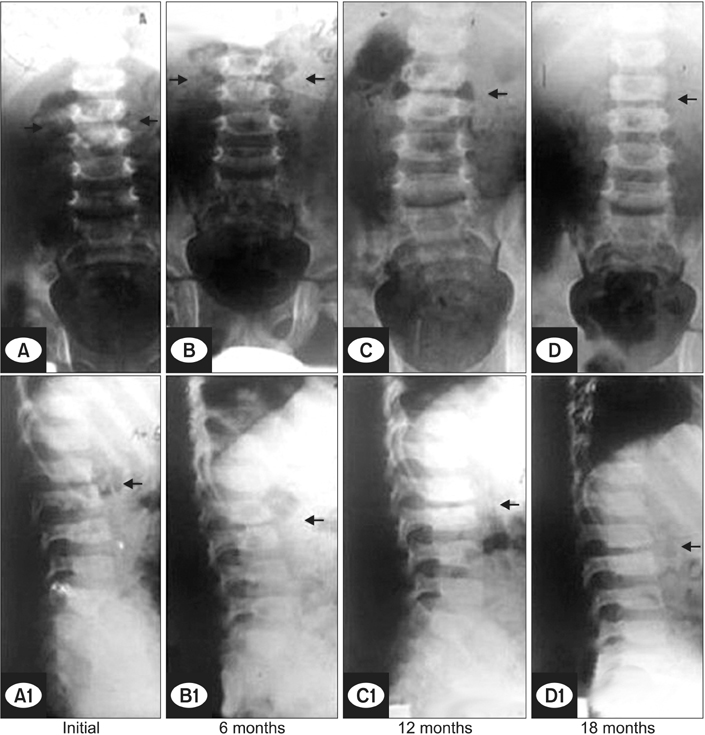
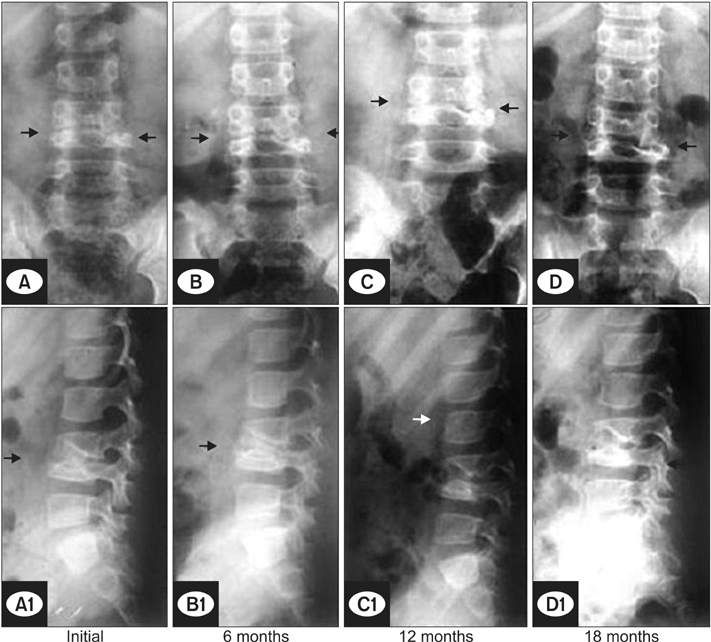
Spinal Tuberculosis in Children: Predictable Kyphotic Deformity after Cure of the Tuberculosis
- Affiliations
-
- 1Department of Orthopedic Surgery and Traumatology, Cheju Halla General Hospital, Jeju, Korea. msmoonos@hotmail.com
- 2CUREnCARE Research, Seoul, Korea.
- KMID: 2369574
- DOI: http://doi.org/10.4055/jkoa.2017.52.1.73
Abstract
- PURPOSE
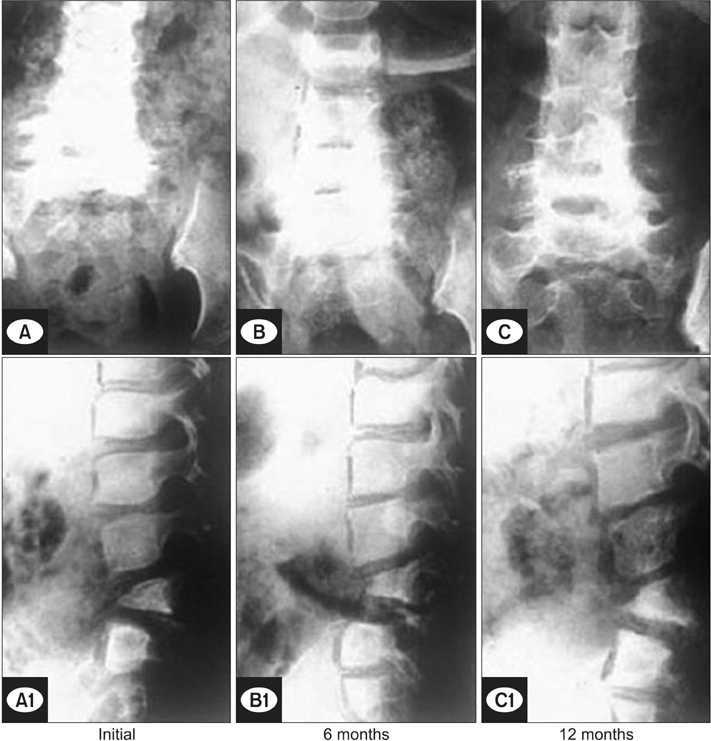
To assess the chronological changes of disease-related kyphosis after chemotherapy alone.
MATERIALS AND METHODS
A total of 101 children aged 2 to 15 years with spinal tuberculosis, accompanied by various stages of disease processes were enrolled for analysis. By utilizing the images in them, the growth plate condition and chronological changes of kyphosis after chemotherapy were analyzed at two points in time; the first assessment was at post-chemotherapy one-year and second at the final discharge.
RESULTS
Complete disc destruction in the cervical, dorsal and lumbosacral spines was observed in 2 out of 40 children (5.0%), 8 out of 30 children (26.7%), and 6 out of 31 children (19.4%), respectively. In those cases, the residual kyphosis inevitably developed. In the remaining children, the discs were intact or partially damaged. Among the 101 children kyphotic deformity was maintained without change in 20 children (19.8%). Kyphosis decreased in 14 children (13.9%), while it increased in 67 children (66.3%) with non-recoverably damaged growth plate.
CONCLUSION
Although it is tentatively possible to predict the deformity progress or non-progress and spontaneous correction at the time of the initial treatment, its predictive accuracy is low. Therefore, assessment of the chronological changes should be performed at the end of chemotherapy. In children with progressive curve change, assessment of deformity should be continued until maturity.
Keyword
MeSH Terms
Figure
Reference
-
1. Schulitz KP, Kothe R, Leong JC, Wehling P. Growth changes of solidly fused kyphotic bloc after surgery for tuberculosis. Comparison of four procedures. Spine (Phila Pa 1976). 1997; 22:1150–1155.2. Moon MS, Kim I, Woo YK, Park YO. Conservative treatment of tuberculosis of the thoracic and lumbar spine in adults and children. Int Orthop. 1987; 11:315–322.3. Moon MS. Tuberculosis of the spine. Controversies and a new challenge. Spine (Phila Pa 1976). 1997; 22:1791–1797.4. A 10-year assessment of controlled trials of inpatient and outpatient treatment and of plaster-of-Paris jackets for tuberculosis of the spine in children on standard chemotherapy. Studies in Masan and Pusan, Korea. Ninth report of the Medical Research Council Working Party on Tuberculosis of the Spine. J Bone Joint Surg Br. 1985; 67:103–110.5. Moon MS, Moon YW, Moon JL, Kim SS, Sun DH. Conservative treatment of tuberculosis of the lumbar and lumbosacral spine. Clin Orthop Relat Res. 2002; (398):40–49.6. Moon MS, Moon JL, Kim SS, Moon YW. Treatment of tuberculosis of the cervical spine: operative versus nonoperative. Clin Orthop Relat Res. 2007; 460:67–77.7. Moon MS, Lee BJ, Kim SS, Lin JF. Evolution of management of spinal deformity: controversial issues and current concept review. J Spinal Surg. 2010; 2:295–305.8. Moon MS, Kim JM. The effect of mechanical forces on vertebral growth preliminary report. J Western Pacif Orthop Assoc. 1974; 11:1–26.9. Rajasekaran S. The problem of deformity in spinal tuberculosis. Clin Orthop Relat Res. 2002; (398):85–92.10. Rajasekaran S. The natural history of post-tubercular kyphosis in children. Radiological signs which predict late increase in deformity. J Bone Joint Surg Br. 2001; 83:954–956.11. Moon MS, Kim SS, Lee BJ, Moon JL. Spinal tuberculosis in children: retrospective analysis of 124 patients. Indian J Orthop. 2012; 46:150–158.12. Bailey HL, Gabriel M, Hodgson AR, Shin JS. Tuberculosis of the spine in children. J Bone Joint Surg Am. 1972; 54:1633–1657.13. Five-year assessments of controlled trials of ambulatory treatment, debridement and anterior spinal fusion in the management of tuberculosis of the spine. Studies in Bulawayo (Rhodesia) and in Hong Kong. Sixth report of the Medical Research Council Working Party on Tuberculosis of the Spine. J Bone Joint Surg Br. 1978; 60:163–177.14. Schulitz KP, Kothe R, Leong JC, Wehling P. Growth changes of solidly fused kyphotic bloc after surgery for tuberculosis. Comparison of four procedures. Spine (Phila Pa 1976). 1997; 22:1150–1155.15. Upadhyay SS, Saji MJ, Sell P, Sell B, Hsu LC. Spinal deformity after childhood surgery for tuberculosis of the spine. A comparison of radical surgery and debridement. J Bone Joint Surg Br. 1994; 76:91–98.16. Tuli SM. Tuberculosis of the skeletal system: bones, joints, spine, and bursal sheaths. 3rd ed. New Delli: Jaypee Brothers Medical Publishers;2004.17. Jain AK, Aggarwal PK, Arora A, Singh S. Behaviour of the kyphotic angle in spinal tuberculosis. Int Orthop. 2004; 28:110–114.18. Masini M, Maranhão V. Experimental determination of the effect of progressive sharp-angle spinal deformity on the spinal cord. Eur Spine J. 1997; 6:89–92.19. Moon MS, Kim SS, Shin JC. Tuberculous kyphosis Evolving concepts in prevention and treatment. J Musculoskelet Res. 2015; 18:1–14.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes of kyphotic angle in children and adults after anterior intervertebral fusion in spinal tuberculosis
- Results of Single-Staged Posterior Decompression and Circumferential Fusion Using a Transpedicular Approach to Correct a Kyphotic Deformity due to Thoracolumbar Spinal Tuberculosis
- Evaluation of the Behavior of Spinal Deformities in Tuberculosis of the Spine in Adults
- The Correction of Severe Spinal Kyphotic Deformities with Halo-pelvic Apparatus
- Clinical Study on Progression of Kyphosis in Spinal Tuberculosis Treated by Anterior Arthrodesis