Effectiveness of Implantable Cardioverter-Defibrillator Therapy for Heart Failure Patients according to Ischemic or Non-Ischemic Etiology in Korea
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Yeungnam University Medical Center, Daegu, Korea. dgshin@med.yu.ac.kr
- 2Division of Cardiology, Department of Internal Medicine, Daegu Fatima Hospital, Daegu, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea.
- 4Division of Cardiology, Department of Internal Medicine, Keimyung University Dongsan Medical Center, Daegu, Korea.
- 5Division of Cardiology, Department of Internal Medicine, Catholic University Medical Center, Daegu, Korea.
- 6Cardiovascular Center, Andong Medical Group, Andong, Korea.
- 7Division of Cardiology, Department of Internal Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 8Division of Cardiology, Department of Internal Medicine, Inje University Busan Paik Hospital, Busan, Korea.
- 9Division of Cardiology, Department of Internal Medicine, Kosin University Gospel Hospital, Busan, Korea.
- KMID: 2365285
- DOI: http://doi.org/10.4070/kcj.2016.0242
Abstract
- BACKGROUND AND OBJECTIVES
This study was performed to describe clinical characteristics of patients with left ventriculars (LV) dysfunction and implantable cardioverter-defibrillator (ICD), and to evaluate the effect of ICD therapy on survival in Yeongnam province of Korea.
SUBJECTS AND METHODS
From a community-based device registry (9 centers, Yeongnam province, from November 1999 to September 2012), 146 patients with LV dysfunction and an ICD implanted for primary or secondary prophylaxis, were analyzed. The patients were divided into two groups, based on the etiology (73 with ischemic cardiomyopathy and 73 with non-ischemic cardiomyopathy), and indication for the device implantation (36 for primary prevention and 110 for secondary prevention). The cumulative first shock rate, all cause death, and type and mode of death, were determined according to the etiology and indication.
RESULTS
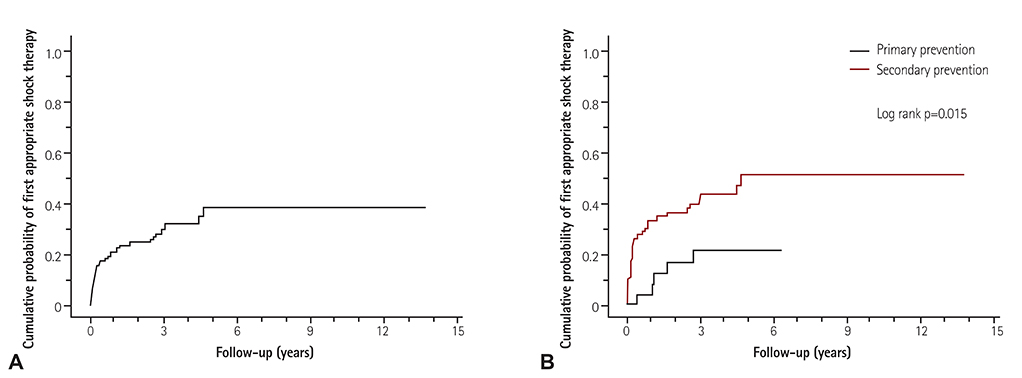
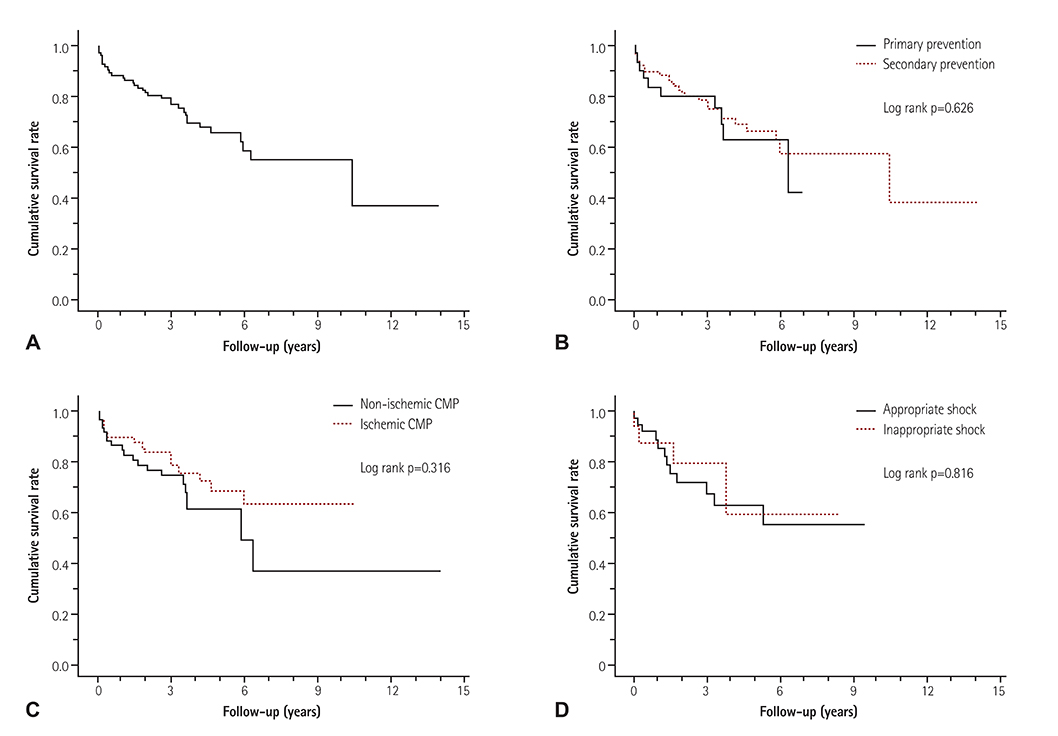
Over a mean follow-up of 3.5 years, the overall ICD shock rate was about 39.0%. ICD shock therapy was significantly more frequent in the secondary prevention group (46.4% vs. 16.7%, p=0.002). The cumulative probability of a first appropriate shock was higher in the secondary prevention group (p=0.015). There was no significant difference in the all-cause death, cardiac death, and mode of death between the groups according to the etiology and indication.
CONCLUSION
Studies from this multicenter regional registry data shows that in both ischemic and non-ischemic cardiomyopathy patients, the ICD shock therapy rate was higher in the secondary prevention group than primary prevention group.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Implantable Cardioverter-defibrillator Utilization and Its Outcomes in Korea: Data from Korean Acute Heart Failure Registry
Youngjin Cho, Sang-Yeong Cho, Il-Young Oh, Ji Hyun Lee, Jin Joo Park, Hae-Young Lee, Kye Hun Kim, Byung-Su Yoo, Seok-Min Kang, Sang Hong Baek, Eun-Seok Jeon, Jae-Joong Kim, Myeong-Chan Cho, Shung Chull Chae, Byung-Hee Oh, Dong-Ju Choi
J Korean Med Sci. 2020;35(46):e397. doi: 10.3346/jkms.2020.35.e397.Cardiac Implantable Electronic Device Therapy in Korea: Increasing but Still Quite Low
Myung Hwan Bae
Korean Circ J. 2019;49(9):853-855. doi: 10.4070/kcj.2019.0131.Clinical Impact of Implantable Cardioverter-Defibrillator Therapy and Mortality Prediction Model for Effective Primary Prevention in Korean Patients
Myung Hwan Bae, Yongkeun Cho, Jongmin Hwang, Hyoung-Seob Park, Seongwook Han, Young Soo Lee, Hyun Jun Cho, Byung Chun Jung, Chan-Hee Lee, Dae-Woo Hyun, Jong Sung Park, Jinhee Ahn, Ki-Hun Kim, Dong-Gu Shin
J Korean Med Sci. 2020;35(9):. doi: 10.3346/jkms.2020.35.e49.
Reference
-
1. Epstein AE, DiMarco JP, Ellenbogen KA, et al. 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2013; 61:e6–e75.2. Mann DL, Zipes DP, Libby P, Bonow RO, Braunwald E. Braunwald's heart disease: a textbook of cardiovascular medicine. 10th ed. Philadelphia: Elsevier Saunders;2015. p. 724–725.3. Moss AJ, Hall WJ, Cannom DS, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter automatic defibrillator implantation trial investigators. N Engl J Med. 1996; 335:1933–1940.4. The Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators. A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N Engl J Med. 1997; 337:1576–1583.5. Bigger JT Jr. Coronary Artery Bypass Graft (CABG) Patch Trial Investigators. Prophylactic use of implanted cardiac defibrillators in patients at high risk for ventricular arrhythmias after coronary-artery bypass graft surgery. N Engl J Med. 1997; 337:1569–1575.6. Connolly SJ, Gent M, Roberts RS, et al. Canadian implantable defibrillator study (CIDS): a randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation. 2000; 101:1297–1302.7. Bänsch D, Antz M, Boczor S, et al. Primary prevention of sudden cardiac death in idiopathic dilated cardiomyopathy: the Cardiomyopathy Trial (CAT). Circulation. 2002; 105:1453–1458.8. Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002; 346:877–883.9. Kadish A, Dyer A, Daubert JP, et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med. 2004; 350:2151–2158.10. Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005; 352:225–237.11. Daubert JP, Zareba W, Cannom DS, et al. Inappropriate implantable cardioverter-defibrillator shocks in MADIT II: frequency, mechanisms, predictors, and survival impact. J Am Coll Cardiol. 2008; 51:1357–1365.12. Koneru JN, Swerdlow CD, Wood MA, Ellenbogen KA. Minimizing inappropriate or “unnecessary” implantable cardioverter-defibrillator shocks: appropriate programming. Circ Arrhythm Electrophysiol. 2011; 4:778–790.13. Lee SW, Kim HC, Lee HS, Suh I. Thirty-year trends in mortality from cardiovascular diseases in Korea. Korean Circ J. 2015; 45:202–209.14. Kim J, Choi EK, Lee MH, et al. The relevance of the primary prevention criteria for implantable cardioverter defibrillator implantation in korean symptomatic severe heart failure patients. Korean Circ J. 2012; 42:173–183.15. Yang JH, Byeon K, Yim HR, et al. Predictors and clinical impact of inappropriate implantable cardioverter-defibrillator shocks in Korean patients. J Korean Med Sci. 2012; 27:619–624.16. Kutyifa V, Daubert JP, Schuger C, et al. Novel ICD programming and inappropriate ICD therapy in CRT-D versus ICD patients: a MADIT-RIT sub-study. Circ Arrhythm Electrophysiol. 2016; 9:e001965.17. Verma A, Sarak B, Kaplan AJ, et al. Predictors of appropriate implantable cardioverter defibrillator (ICD) therapy in primary prevention patients with ischemic and nonischemic cardiomyopathy. Pacing Clin Electrophysiol. 2010; 33:320–329.18. Moss AJ, Schuger C, Beck CA, et al. Reduction in inappropriate therapy and mortality through ICD programming. N Engl J Med. 2012; 367:2275–2283.19. Gracieux J, Sanders GD, Pokorney SD, Lopes RD, Thomas K, Al-Khatib SM. Incidence and predictors of appropriate therapies delivered by the implantable cardioverter defibrillator in patients with ischemic cardiomyopathy: a systematic review. Int J Cardiol. 2014; 177:990–994.20. Klein RC, Raitt MH, Wilkoff BL, et al. Analysis of implantable cardioverter defibrillator therapy in the Antiarrhythmics Versus Implantable Defibrillators (AVID) trial. J Cardiovasc Electrophysiol. 2003; 14:940–948.21. Sedlacek K, Ruwald AC, Kutyifa V, et al. The effect of ICD programming on inappropriate and appropriate ICD Therapies in ischemic and nonischemic cardiomyopathy: the MADIT-RIT trial. J Cardiovasc Electrophysiol. 2015; 26:424–433.22. Auricchio A, Schloss EJ, Kurita T, et al. Low inappropriate shock rates in patients with single-and dual/triple-chamber implantable cardioverter-defibrillators using a novel suite of detection algorithms: PainFree SST trial primary results. Heart Rhythm. 2015; 12:926–936.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Implantable Cardioverter-defibrillator for Primary Prevention of Sudden Cardiac Death in Non-ischemic Cardiomyopathy
- Transvenous Implantation of an Implantable Cardioverter Defibrillator in a Patient Who Had Undergone Tricuspid Valve Replacement
- Implantable Cardioverter-Defibrillator and Cardiac Resynchronization Therapy
- A Case Report of the Patient Implanted with Automatic Implantable Cardioverter Defibrillator (AICD) Subject to 3rd Molar Extraction using Target Controlled Infusion of Propofol and Remifentanil: A Case Report
- Early Detection of Subclinical Atrial Flutter-Fibrillation in Patients with Unexplained Palpitation Using a Novel VDD Defibrillator with Integrated Atrial-Sensing Rings