J Korean Assoc Pediatr Surg.
2016 Dec;22(2):42-48. 10.13029/jkaps.2016.22.2.42.
Trend of Pediatric Cholecystectomy: Clinical Characteristics and Indications for Cholecystectomy
- Affiliations
-
- 1Department of Pediatric Surgery, Seoul National University Children's Hospital, Seoul, Korea. spkhy02@snu.ac.kr
- 2Department of Pediatric Surgery, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2363023
- DOI: http://doi.org/10.13029/jkaps.2016.22.2.42
Abstract
- PURPOSE
Number of pediatric cholecystectomy has been recently showing a gradually increasing trend. The purpose of this study was to investigate the clinical features of patients who underwent pediatric cholecystectomy, and the latest trend in cholecystectomy.
METHODS
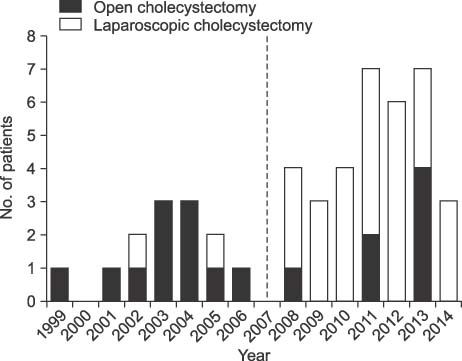
In the present study, we conducted a retrospective chart review on 47 patients who had undergone cholecystectomy at a single center. The entire patient population was divided into two groups, according to the time of cholecystectomy (early group, January 1999 to December 2006; late group, January 2007 to August 2014).
RESULTS
The comparison between the early and late groups showed that the number of cholecystectomy increased from 13 to 34 cases representing a 2.6-fold increase. The mean patient age also increased from 5.94±4.08 years to 10.51±5.57 years (p=0.01). Meanwhile, laparoscopic surgery also increased from 15.4% to 79.4%, respectively (p<0.001). However, sex, mean body mass index, comorbidities, indications of cholecystectomy, and previous total parenteral nutrition were not statistically significant.
CONCLUSION
The results of this study showed that pediatric cholecystectomy cases are increasing, particularly in the 10 to 19 years age group and laparoscopic cholecystectomies are also being performed at an increasing rate. When the patients were compared according to the time of cholecystectomy, there were no differences in other risk factors or indications for cholecystectomy.
Keyword
MeSH Terms
Figure
Reference
-
1. Glenn F. 25-years experience in the surgical treatment of 5037 patients with non-malignant biliary tract disease. Surg Gynecol Obstet. 1959; 109:591–606.2. Shafer AD, Ashley JV, Goodwin CD, Nanagas VN Jr, Elliott D. A new look at the multifactoral etiology of gallbladder disease in children. Am Surg. 1983; 49:314–319.3. Wesdorp I, Bosman D, de Graaff A, Aronson D, van der Blij F, Taminiau J. Clinical presentations and predisposing factors of cholelithiasis and sludge in children. J Pediatr Gastroenterol Nutr. 2000; 31:411–417.
Article4. Calabrese C, Pearlman DM. Gallbladder disease below the age of 21 years. Surgery. 1971; 70:413–415.5. Walker SK, Maki AC, Cannon RM, Foley DS, Wilson KM, Galganski LA, et al. Etiology and incidence of pediatric gallbladder disease. Surgery. 2013; 154:927–931.
Article6. Bailey PV, Connors RH, Tracy TF Jr, Sotelo-Avila C, Lewis JE, Weber TR. Changing spectrum of cholelithiasis and cholecystitis in infants and children. Am J Surg. 1989; 158:585–588.
Article7. Mehta S, Lopez ME, Chumpitazi BP, Mazziotti MV, Brandt ML, Fishman DS. Clinical characteristics and risk factors for symptomatic pediatric gallbladder disease. Pediatrics. 2012; 129:e82–e88.
Article8. Legorreta AP, Silber JH, Costantino GN, Kobylinski RW, Zatz SL. Increased cholecystectomy rate after the introduction of laparoscopic cholecystectomy. JAMA. 1993; 270:1429–1432.
Article9. Moon JS, Lee SY, Nam CM, Choi JM, Choe BK, Seo JW, et al. 2007 Korean National Growth Charts: review of developmental process and an outlook. Korean J Pediatr. 2008; 51:1–25.
Article10. Cirillo DJ, Wallace RB, Rodabough RJ, Greenland P, LaCroix AZ, Limacher MC, et al. Effect of estrogen therapy on gallbladder disease. JAMA. 2005; 293:330–339.
Article11. Ko CW, Beresford SA, Schulte SJ, Matsumoto AM, Lee SP. Incidence, natural history, and risk factors for biliary sludge and stones during pregnancy. Hepatology. 2005; 41:359–365.
Article12. Wang HH, Liu M, Clegg DJ, Portincasa P, Wang DQ. New insights into the molecular mechanisms underlying effects of estrogen on cholesterol gallstone formation. Biochim Biophys Acta. 2009; 1791:1037–1047.
Article13. Von Bergmann K, Becker M, Leiss O. Biliary cholesterol saturation in non-obese women and non-obese men before and after puberty. Eur J Clin Invest. 1986; 16:531–535.
Article14. Kaechele V, Wabitsch M, Thiere D, Kessler AL, Haenle MM, Mayer H, et al. Prevalence of gallbladder stone disease in obese children and adolescents: influence of the degree of obesity, sex, and pubertal development. J Pediatr Gastroenterol Nutr. 2006; 42:66–70.
Article15. Dittrick GW, Thompson JS, Campos D, Bremers D, Sudan D. Gallbladder pathology in morbid obesity. Obes Surg. 2005; 15:238–242.
Article16. Kim HY, Kim SH, Cho YH. Pediatric cholecystectomy: clinical significance of cases unrelated to hematologic disorders. Pediatr Gastroenterol Hepatol Nutr. 2015; 18:115–120.
Article17. Holcomb GW 3rd, Morgan WM 3rd, Neblett WW 3rd, Pietsch JB, O'Neill JA Jr, Shyr Y. Laparoscopic cholecystectomy in children: lessons learned from the first 100 patients. J Pediatr Surg. 1999; 34:1236–1240.
Article18. Kim HS, Nam SH, Kim DY, Kim SC, Kim IG. Laparoscopic cholecystectomy in children. J Korean Assoc Pediatr Surg. 2006; 12:213–220.
Article19. Gowda DJ, Agarwal P, Bagdi R, Subramanian B, Kumar M, Ramasundaram M, et al. Laparoscopic cholecystectomy for cholelithiasis in children. J Indian Assoc Pediatr Surg. 2009; 14:204–206.
Article20. Oh KW, Jang MJ, Lee NY, Moon JS, Lee CG, Yoo MH, et al. Prevalence and trends in obesity among Korean children and adolescents in 1997 and 2005. Korean J Pediatr. 2008; 51:950–955.
Article21. Jeanty C, Derderian SC, Courtier J, Hirose S. Clinical management of infantile cholelithiasis. J Pediatr Surg. 2015; 50:1289–1292.
Article22. Miltenburg DM, Schaffer R 3rd, Breslin T, Brandt ML. Changing indications for pediatric cholecystectomy. Pediatrics. 2000; 105:1250–1253.
Article23. Halpern Z, Vinograd Z, Laufer H, Gilat T, Moskowitz M, Bujanover Y. Characteristics of gallbladder bile of infants and children. J Pediatr Gastroenterol Nutr. 1996; 23:147–150.
Article24. Goncalves RM, Harris JA, Rivera DE. Biliary dyskinesia: natural history and surgical results. Am Surg. 1998; 64:493–497.25. Gollin G, Raschbaum GR, Moorthy C, Santos L. Cholecystectomy for suspected biliary dyskinesia in children with chronic abdominal pain. J Pediatr Surg. 1999; 34:854–857.
Article26. Michail S, Preud'Homme D, Christian J, Nanagas V, Goodwin C, Hitch D, et al. Laparoscopic cholecystectomy: effective treatment for chronic abdominal pain in children with acalculous biliary pain. J Pediatr Surg. 2001; 36:1394–1396.
Article27. Campbell BT, Narasimhan NP, Golladay ES, Hirschl RB. Biliary dyskinesia: a potentially unrecognized cause of abdominal pain in children. Pediatr Surg Int. 2004; 20:579–581.
Article28. Lacher M, Yannam GR, Muensterer OJ, Aprahamian CJ, Haricharan RN, Perger L, et al. Laparoscopic cholecystectomy for biliary dyskinesia in children: frequency increasing. J Pediatr Surg. 2013; 48:1716–1721.
Article29. Srinath AI, Youk AO, Bielefeldt K. Biliary dyskinesia and symptomatic gallstone disease in children: two sides of the same coin? Dig Dis Sci. 2014; 59:1307–1315.
Article30. Fahey F, Zukotynski K, Zurakowski D, Markelewicz R, Falone A, Vitello M, et al. Beyond current guidelines: reduction in minimum administered radiopharmaceutical activity with preserved diagnostic image quality in pediatric hepatobiliary scintigraphy. Eur J Nucl Med Mol Imaging. 2014; 41:2346–2353.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Korea University Experience in Laparoscopic Cholecystectomy
- Laparoscopic Cholecystectomy in the Second Trimester of Pregnancy
- A comparison od clinical results for laparoscopic cholecystectomy versus standard open cholecystectomy
- Comparison of Laparoscopic Cholecystectomy and Minilaparotomy Cholecystectomy
- A Clinical Analysis of 300 Case of Laparoscopic Cholecystectomy