Anesth Pain Med.
2016 Apr;11(2):155-159. 10.17085/apm.2016.11.2.155.
Anesthetic experience of Benedikt syndrome complicating lumbar spine involved multiple myeloma: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Gachon University Gil Medical Center, Incheon, Korea. endless37@gilhospital.com
- 2Department of Anesthesiology and Pain Medicine, Ajou University College of Medicine, Suwon, Korea.
- KMID: 2358477
- DOI: http://doi.org/10.17085/apm.2016.11.2.155
Abstract
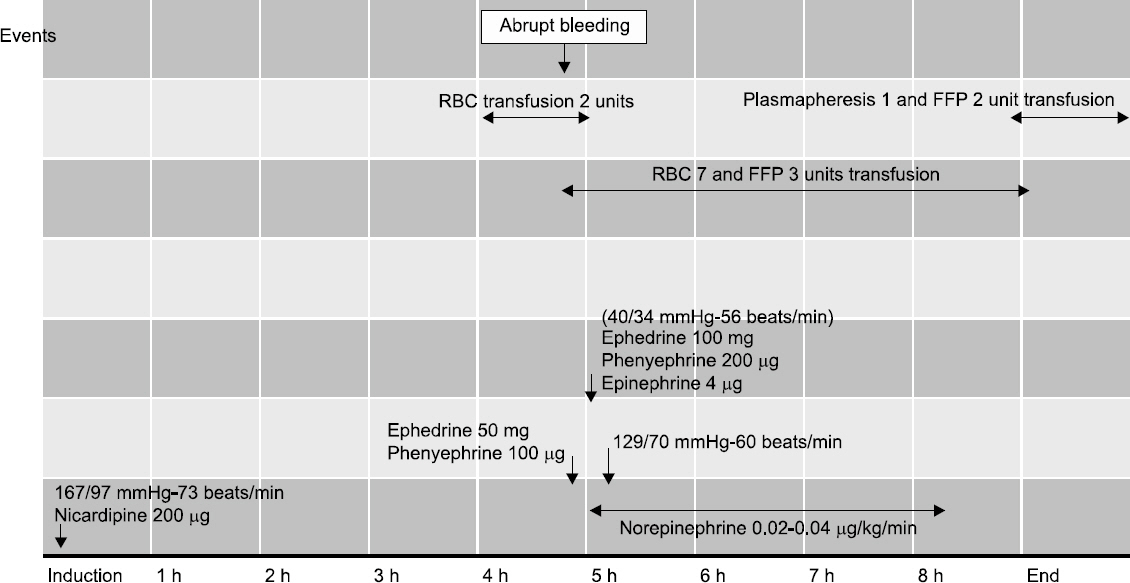
- Benedikt syndrome is characterized by ipsilateral ophthalmoplegia with contralateral hemichorea due to a midbrain lesion. A 67-year-old male with Benedikt syndrome underwent corpectomy at L1 and anterolateral interbody fusion at T12-L2 due to pathologic bursting fracture at L1 involving multiple myeloma. He had a history of traumatic subarachnoid hemorrhage and subdural hemorrhage 8 months before surgery. Magnetic resonance image of the brain revealed intracranial hemorrhage from thalamus to midbrain. Target controlled infusion with propofol and remifentanil were administered for anesthetic induction and maintenance and close hemodynamic and neurologic monitoring led to successful anesthetic management.
Keyword
MeSH Terms
Figure
Reference
-
1. Paidakakos NA, Rokas E, Theodoropoulos S, Dimogerontas G, Konstantinidis E. Posttraumatic Benedikt’s syndrome: a rare entity with unclear anatomopathological correlations. World Neurosurg. 2012; 78:715e13–5. DOI: 10.1016/j.wneu.2012.03.028. PMID: 22484069.
Article2. Itoh H, Shibata K, Nitta E, Takamori M. Hemiballism-hemichorea from marked hypotension during spinal anesthesia. Acta Anaesthesiol Scand. 1998; 42:133–5. DOI: 10.1111/j.1399-6576.1998.tb05095.x. PMID: 9527738.3. Bae H, Jeong D, Doh J, Lee K, Yun I, Byun B. Recurrence of bleeding in patients with hypertensive intracerebral hemorrhage. Cerebrovasc Dis. 1999; 9:102–8. DOI: 10.1159/000015906. PMID: 9973653.
Article4. Ruchalski K, Hathout GM. A medley of midbrain maladies: a brief review of midbrain anatomy and syndromology for radiologists. Radiol Res Pract. 2012; 2012:258–524. DOI: 10.1155/2012/258524.
Article5. Bandt SK, Anderson D, Biller J. Deep brain stimulation as an effective treatment option for post-midbrain infarction-related tremor as it presents with Benedikt syndrome. J Neurosurg. 2008; 109:635–9. DOI: 10.3171/JNS/2008/109/10/0635. PMID: 18826349.
Article6. Etezadi F, Najafi A, Yarandi KK, Moharari RS, Khajavi MR. ICU sedation with haloperidol-propofol infusion versus midazolam-propofol infusion after coronary artery bypass graft surgery: a prospective, double-blind randomized study. Ann Card Anaesth. 2012; 15:185–9. DOI: 10.4103/0971-9784.97974. PMID: 22772512.
Article7. Jo YY, Kim YB, Yang MR, Chang YJ. Extrapyramidal side effects after metoclopramide administration in a post-anesthesia care unit -A case report-. Korean J Anesthesiol. 2012; 63:274–6. DOI: 10.4097/kjae.2012.63.3.274. PMID: 23060988. PMCID: PMC3460160.
Article8. Moleman P, Schmitz PJ, Ladee GA. Extrapyramidal side effects and oral haloperidol: an analysis of explanatory patient and treatment characteristics. J Clin Psychiatry. 1982; 43:492–6. PMID: 7161250.9. Ogawa M. Pharmacological treatments of cerebellar ataxia. Cerebellum. 2004; 3:107–11. DOI: 10.1080/147342204100032331. PMID: 15233578.
Article10. Kim WH, Lee JJ, Lee SM, Park MN, Park SK, Seo DW, et al. Comparison of motor-evoked potentials monitoring in response to transcranial electrical stimulation in subjects undergoing neurosurgery with partial vs no neuromuscular block. Br J Anaesth. 2013; 110:567–76. DOI: 10.1093/bja/aes395. PMID: 23378247.11. Sloan TB, Toleikis JR, Toleikis SC, Koht A. Intraoperative neurophysiological monitoring during spine surgery with total intravenous anesthesia or balanced anesthesia with 3% desflurane. J Clin Monit Comput. 2015; 29:77–85. DOI: 10.1007/s10877-014-9571-9. PMID: 24643708.
Article12. Gokce BM, Ozkose Z, Tuncer B, Pampal K, Arslan D. Hemodynamic effects, recovery profiles, and costs of remifentanil-based anesthesia with propofol or desflurane for septorhinoplasty. Saudi Med J. 2007; 28:358–63. PMID: 17334459.13. Scheufler KM, Zentner J. Total intravenous anesthesia for intraoperative monitoring of the motor pathways: an integral view combining clinical and experimental data. J Neurosurg. 2002; 96:571–9. DOI: 10.3171/jns.2002.96.3.0571. PMID: 11883843.
Article14. O’Riordan S, McGuigan C, Stevens J, Chapman N, Ball J. Reversible hypertensive cerebellar encephalopathy and hydrocephalus. J Neurol Neurosurg Psychiatry. 2007; 78:1008–9. DOI: 10.1136/jnnp.2006.107672. PMID: 17332051. PMCID: PMC2117878.15. Prasad KK. Roizen M, Fleisher L, editors. Multiple myeloma. Essence of anaesthesia practice. 2002. 2nd ed. Philadelphia: WB Saunders Company;p. 229.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rapid Progression of Solitary Plasmacytoma to Multiple Myeloma in Lumbar Vertebra
- A Case of Solitary Myeloma of the Lumbar Spine
- Continuous Multiple Vertebral Compression Fractures in Multiple Myeloma Patient
- Plasma Cell Myeloma: A Report of 2 Cases
- Nonsecretory Multiple Myeloma with Multiple Spine Fracture