Clin Endosc.
2016 Sep;49(5):425-433. 10.5946/ce.2016.065.
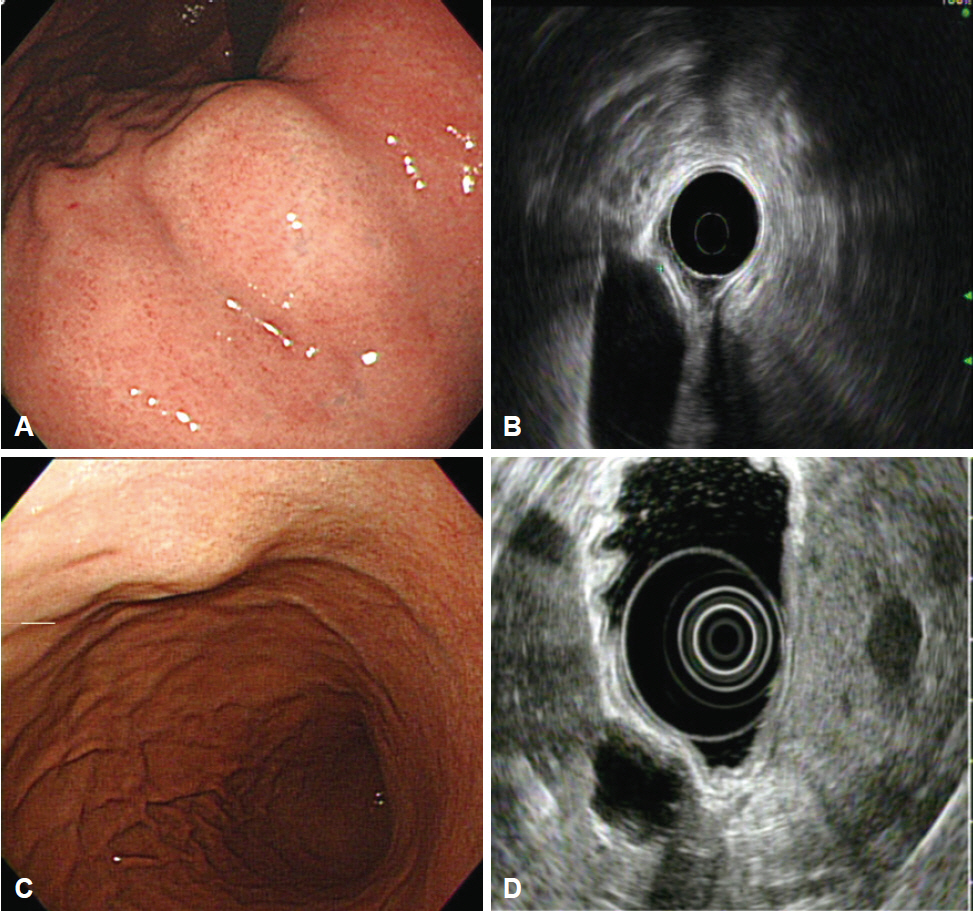
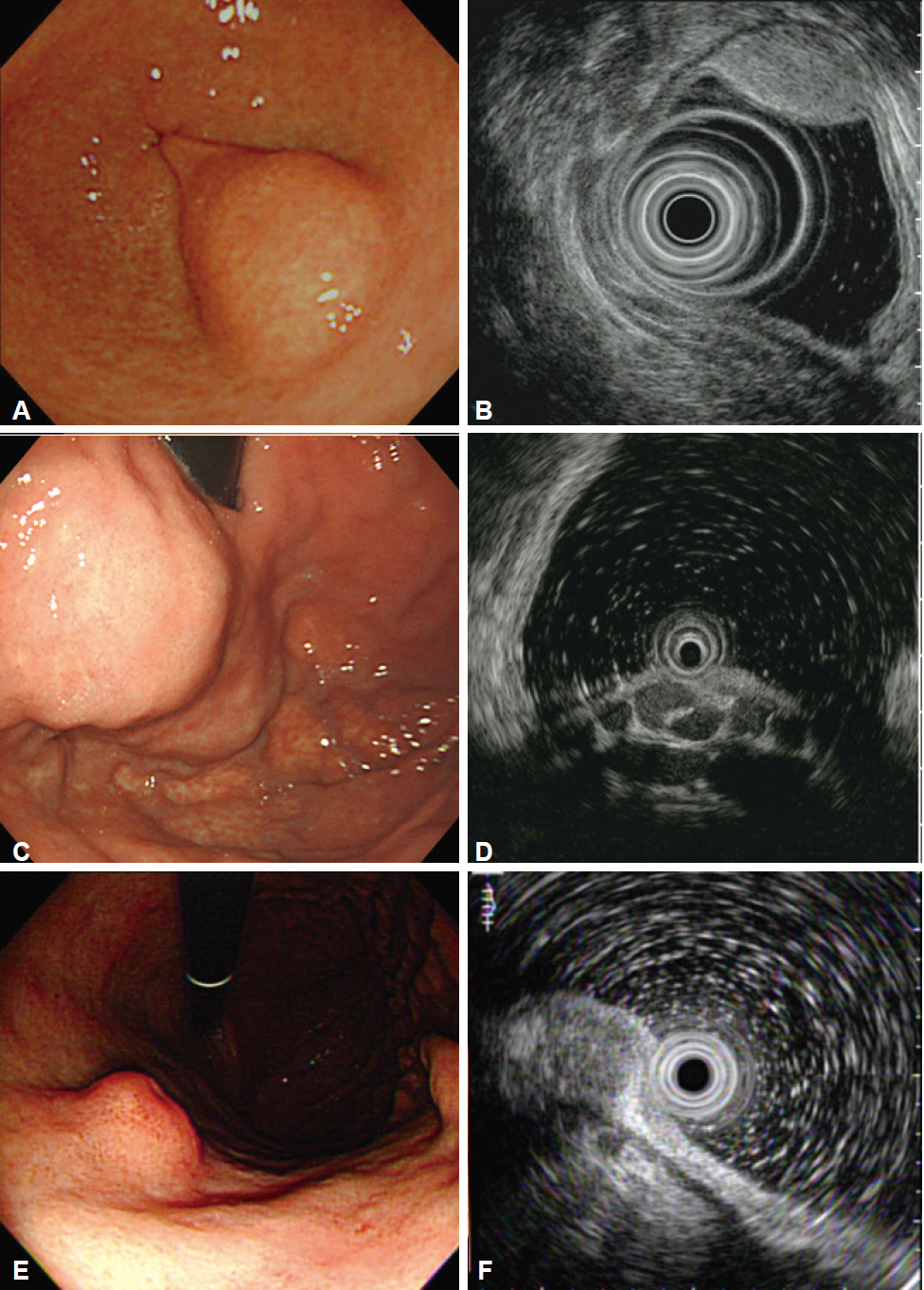
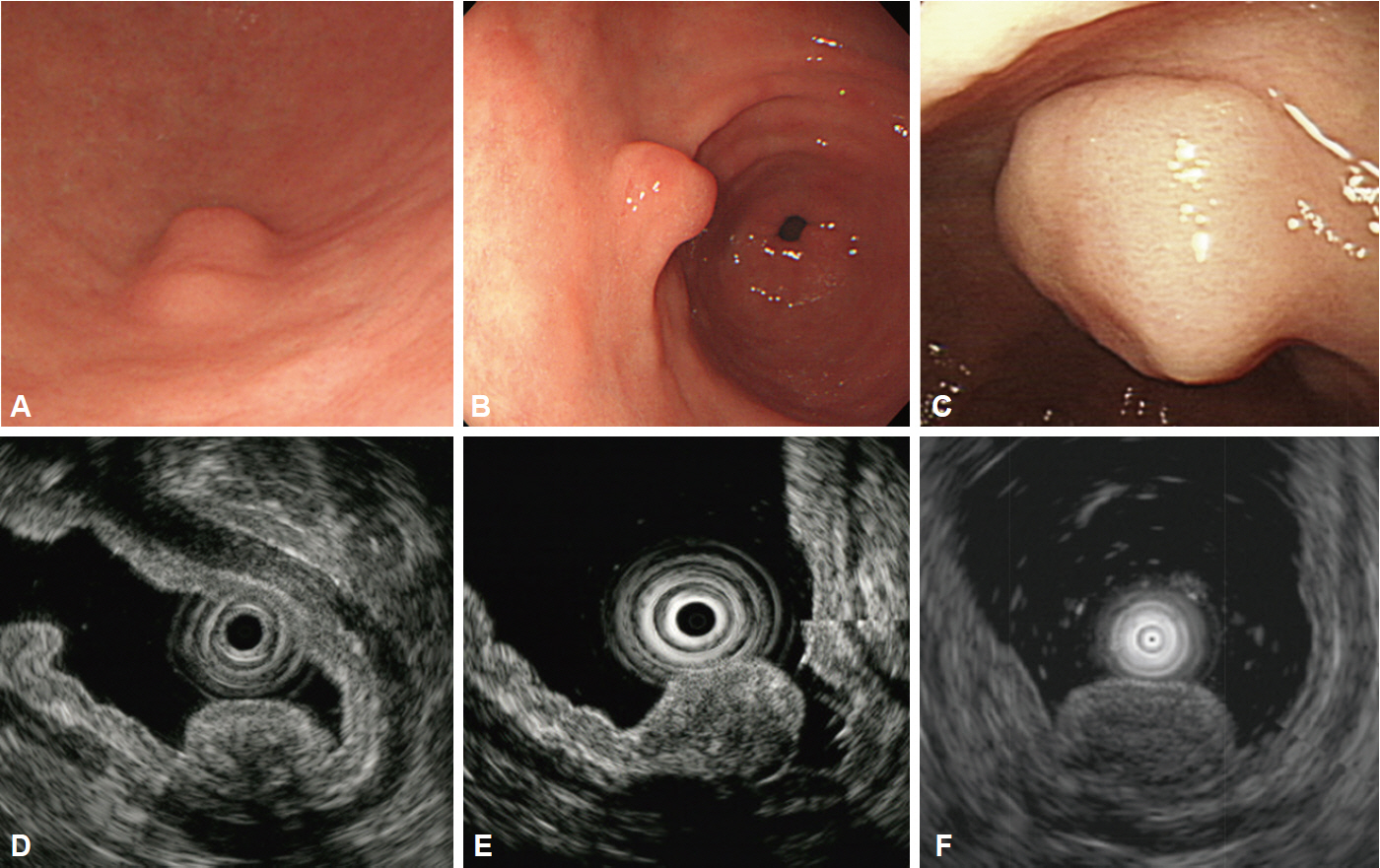
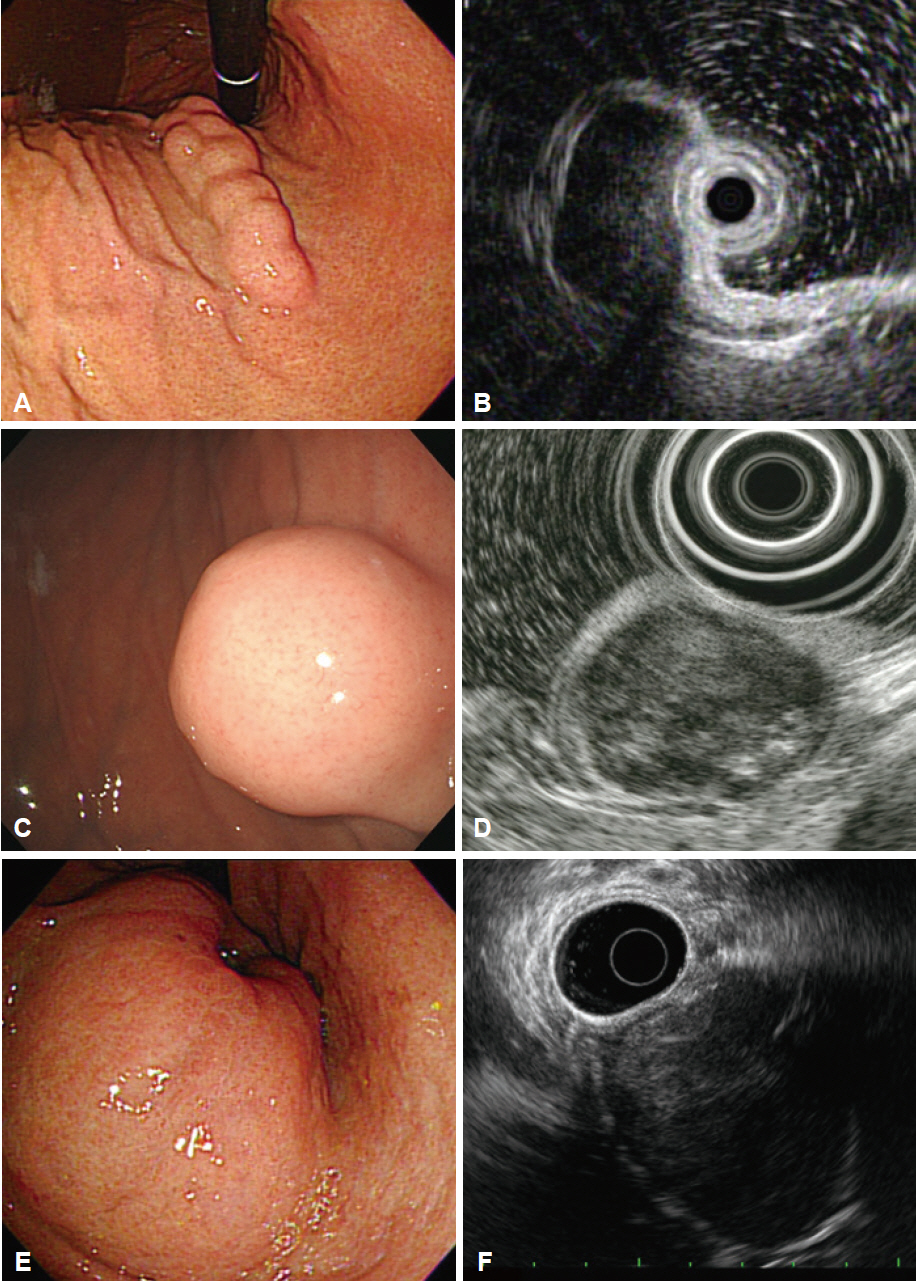
Endoscopic Ultrasonography in the Diagnosis of Gastric Subepithelial Lesions
- Affiliations
-
- 1Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. dohoon.md@gmail.com
- KMID: 2356047
- DOI: http://doi.org/10.5946/ce.2016.065
Abstract
- Subepithelial lesions occasionally found in the stomach of patients undergoing endoscopy may be either benign lesions or tumors with malignant potential. They may also appear due to extrinsic compression. Discrimination of gastric subepithelial lesions begins with meticulous endoscopic examination for size, shape, color, mobility, consistency, and appearance of the overlying mucosa. Accurate diagnosis can be achieved with endoscopic ultrasonography, which provides useful information on the exact size, layer-of-origin, and characteristic morphologic features to support a definitive diagnosis. Endoscopic ultrasonography also aids in the prediction of malignant potential, especially in gastrointestinal stromal tumors. Features of subepithelial lesions identified on endoscopic ultrasonography can be used to determine whether further diagnostic procedures such as endoscopic resection, fine needle aspiration, or core biopsy are required. Endoscopic ultrasonography is a valuable tool for diagnosis and clinical decision making during follow-up of gastric subepithelial lesions.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Current Status of Endoscopic Ultrasonography in Gastrointestinal Subepithelial Tumors
Sang Gyun Kim, Ji Hyun Song, Joo Ha Hwang
Clin Endosc. 2019;52(4):301-305. doi: 10.5946/ce.2019.024.Endoscopically resected duodenal lipoma as an uncommon cause of upper gastrointestinal bleeding: a case report
Dong Chan Joo, Gwang Ha Kim, Bong Eun Lee, Moon Won Lee, Cheolung Kim
Ewha Med J. 2024;47(1):e8. doi: 10.12771/emj.2024.e8.
Reference
-
1. Hedenbro JL, Ekelund M, Wetterberg P. Endoscopic diagnosis of submucosal gastric lesions. The results after routine endoscopy. Surg Endosc. 1991; 5:20–23.2. Lim YJ, Son HJ, Lee JS, et al. Clinical course of subepithelial lesions detected on upper gastrointestinal endoscopy. World J Gastroenterol. 2010; 16:439–444.
Article3. Song JH, Kim SG, Chung SJ, Kang HY, Yang SY, Kim YS. Risk of progression for incidental small subepithelial tumors in the upper gastrointestinal tract. Endoscopy. 2015; 47:675–679.
Article4. Hwang JH, Saunders MD, Rulyak SJ, Shaw S, Nietsch H, Kimmey MB. A prospective study comparing endoscopy and EUS in the evaluation of GI subepithelial masses. Gastrointest Endosc. 2005; 62:202–208.
Article5. Rosch T, Kapfer B, Will U, et al. Accuracy of endoscopic ultrasonography in upper gastrointestinal submucosal lesions: a prospective multicenter study. Scand J Gastroenterol. 2002; 37:856–862.6. Oztas E, Oguz D, Kurt M, et al. Endosonographic evaluation of patients with suspected extraluminal compression or subepithelial lesions during upper gastrointestinal endoscopy. Eur J Gastroenterol Hepatol. 2011; 23:586–592.
Article7. Motoo Y, Okai T, Ohta H, et al. Endoscopic ultrasonography in the diagnosis of extraluminal compressions mimicking gastric submucosal tumors. Endoscopy. 1994; 26:239–242.
Article8. Matsushita M, Hajiro K, Okazaki K, Takakuwa H. Gastric aberrant pancreas: EUS analysis in comparison with the histology. Gastrointest Endosc. 1999; 49(4 Pt 1):493–497.
Article9. Matsushita M, Okazaki K. Characteristic endoscopic features of gastric inflammatory fibroid polyps. J Gastroenterol Hepatol. 2005; 20:1310.
Article10. Matsushita M, Hajiro K, Okazaki K, Takakuwa H. Gastric inflammatory fibroid polyps: endoscopic ultrasonographic analysis in comparison with the histology. Gastrointest Endosc. 1997; 46:53–57.
Article11. Soga J. Early-stage carcinoids of the gastrointestinal tract: an analysis of 1914 reported cases. Cancer. 2005; 103:1587–1595.12. Nakamura S, Iida M, Yao T, Fujishima M. Endoscopic features of gastric carcinoids. Gastrointest Endosc. 1991; 37:535–538.
Article13. Miettinen M, Lasota J. Gastrointestinal stromal tumors: definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch. 2001; 438:1–12.14. Miettinen M, Sarlomo-Rikala M, Lasota J. Gastrointestinal stromal tumors: recent advances in understanding of their biology. Hum Pathol. 1999; 30:1213–1220.
Article15. Fletcher CD, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol. 2002; 33:459–465.
Article16. Palazzo L, Landi B, Cellier C, Cuillerier E, Roseau G, Barbier JP. Endosonographic features predictive of benign and malignant gastrointestinal stromal cell tumours. Gut. 2000; 46:88–92.
Article17. Shah P, Gao F, Edmundowicz SA, Azar RR, Early DS. Predicting malignant potential of gastrointestinal stromal tumors using endoscopic ultrasound. Dig Dis Sci. 2009; 54:1265–1269.
Article18. Reddymasu SC, Oropeza-Vail M, Pakseresht K, et al. Are endoscopic ultrasonography imaging characteristics reliable for the diagnosis of small upper gastrointestinal subepithelial lesions? J Clin Gastroenterol. 2012; 46:42–45.
Article19. Gill KR, Camellini L, Conigliaro R, et al. The natural history of upper gastrointestinal subepithelial tumors: a multicenter endoscopic ultrasound survey. J Clin Gastroenterol. 2009; 43:723–726.20. Voltaggio L, Murray R, Lasota J, Miettinen M. Gastric schwannoma: a clinicopathologic study of 51 cases and critical review of the literature. Hum Pathol. 2012; 43:650–659.
Article21. Okai T, Minamoto T, Ohtsubo K, et al. Endosonographic evaluation of c-kit-positive gastrointestinal stromal tumor. Abdom Imaging. 2003; 28:301–307.
Article22. Jung MK, Jeon SW, Cho CM, et al. Gastric schwannomas: endosonographic characteristics. Abdom Imaging. 2008; 33:388–390.
Article23. Zhong DD, Wang CH, Xu JH, Chen MY, Cai JT. Endoscopic ultrasound features of gastric schwannomas with radiological correlation: a case series report. World J Gastroenterol. 2012; 18:7397–7401.
Article24. Imamura A, Tochihara M, Natsui K, et al. Glomus tumor of the stomach: endoscopic ultrasonographic findings. Am J Gastroenterol. 1994; 89:271–272.25. Baek YH, Choi SR, Lee BE, Kim GH. Gastric glomus tumor: analysis of endosonographic characteristics and computed tomographic findings. Dig Endosc. 2013; 25:80–83.
Article26. Debol SM, Stanley MW, Mallery S, Sawinski E, Bardales RH. Glomus tumor of the stomach: cytologic diagnosis by endoscopic ultrasound-guided fine-needle aspiration. Diagn Cytopathol. 2003; 28:316–321.
Article27. Morrison JG, Gray GF Jr, Dao AH, Adkins RB Jr. Granular cell tumors. Am Surg. 1987; 53:156–160.28. Lack EE, Worsham GF, Callihan MD, et al. Granular cell tumor: a clinicopathologic study of 110 patients. J Surg Oncol. 1980; 13:301–316.
Article29. Matsumoto H, Kojima Y, Inoue T, et al. A malignant granular cell tumor of the stomach: report of a case. Surg Today. 1996; 26:119–122.
Article30. Ensari A. Granular cell tumor: what’s new in diagnosis and treatment? Turk J Gastroenterol. 2007; 18:135–138.31. Kume K, Yoshikawa I, Yamazaki M, Abe S, Murata I, Otsuki M. A case of gastric cancer with features of submucosal tumor. Gastrointest Endosc. 2001; 53:247–249.
Article32. Hosoda Y, Hanai H, Arai H, et al. Early gastric cancer exhibiting the features of submucosal tumor: report of a case. Endoscopy. 1999; 31:S11.33. Wiech T, Walch A, Werner M. Histopathological classification of nonneoplastic and neoplastic gastrointestinal submucosal lesions. Endoscopy. 2005; 37:630–634.
Article34. Cho JW; Korean ESD Study Group. Current guidelines in the management of upper gastrointestinal subepithelial tumors. Clin Endosc. 2016; 49:235–240.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Common Gastric Subepithelial Tumors in Koreans
- Gastric Subepithelial Tumor Diagnosed by Transabdominal Ultrasonography
- Endoscopic Full-Thickness Resection for Gastric Subepithelial Lesions Arising from the Muscularis Propria
- Incidental Gastrointestinal Subepithelial Mass
- Diagnosis of Gastric Subepithelial Tumor: Focusing on Endoscopic Ultrasonography