Intest Res.
2016 Jul;14(3):202-210. 10.5217/ir.2016.14.3.202.
Histological inflammation increases the risk of colorectal neoplasia in ulcerative colitis: a systematic review
- Affiliations
-
- 1Inflammatory Bowel Disease Center, The University of Chicago Medicine, Chicago, IL, USA. drubin@medicine.bsd.uchicago.edu
- 2St. Barnabas Hospital Health System, The Bronx, NY, USA.
- KMID: 2354961
- DOI: http://doi.org/10.5217/ir.2016.14.3.202
Abstract
- BACKGROUND/AIMS
Ulcerative colitis (UC) patients are at greater risk for the development of colorectal neoplasia. Several individual studies have demonstrated associations between severity of histologic inflammation and colorectal neoplasia. However, a comprehensive systematic review has not been completed. We performed a systematic review and meta-analysis to explore the relationship between histologic inflammation and risk for neoplasia among available observational studies.
METHODS
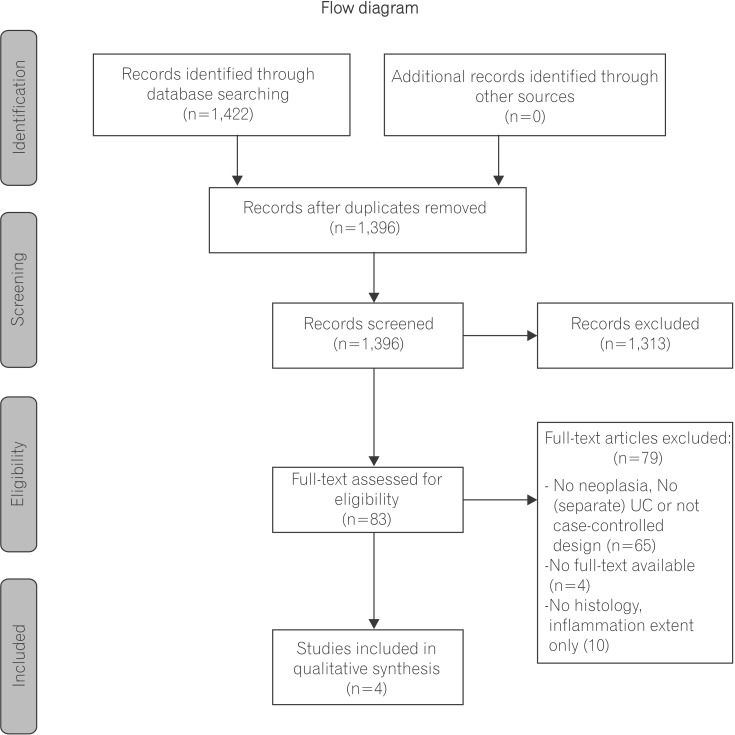
Three databases (EMBASE, MEDLINE and the Cochrane Library) were systematically searched. Studies were included if they included UC patients who underwent colonoscopic assessment and when histologic inflammation and colorectal neoplasia were both reported. Colorectal neoplasia rates were compared. Quantitative meta-analysis was attempted.
RESULTS
Four of 1,422 records found were eligible. Results from 2 case-control studies reported a 3.5-fold increased risk for colorectal neoplasia associated with a single point increase in histologic inflammation. This result was further corroborated by one cohort study that demonstrated increased hazard ratios. The second cohort study reported outcomes for patients with normal gross endoscopy, but had increased histological inflammation when neoplasia was assessed. Finally, this study reported increased risk for neoplastic progression by histological inflammation among patients who were normal by gross endoscopic evaluation. Quantitative meta-analysis was unsuccessful due to heterogeneity between study measures.
CONCLUSIONS
There is strong evidence that histologic inflammation among patients with UC increases the risk of colorectal neoplasia. The depth and nature of assessment of additional clinical variables was varied and may have resulted in greater outcome discrepancy. Additional study related to mechanisms of inflammation-related neoplasia and therapeutic modification is needed.
MeSH Terms
Figure
Cited by 2 articles
-
Endoscopic Submucosal Dissection for Colitis-Associated Dysplasia
Dong-Hoon Yang, Imelda Rey
Clin Endosc. 2019;52(2):120-128. doi: 10.5946/ce.2019.047.Advanced neoplasia detection using chromoendoscopy and white light colonoscopy for surveillance in patients with inflammatory bowel disease
Kyeong Ok Kim, Michael V. Chiorean
Intest Res. 2020;18(4):438-446. doi: 10.5217/ir.2019.00090.
Reference
-
1. Rutter M, Saunders B, Wilkinson K, et al. Severity of inflammation is a risk factor for colorectal neoplasia in ulcerative colitis. Gastroenterology. 2004; 126:451–459. PMID: 14762782.
Article2. Gupta RB, Harpaz N, Itzkowitz S, et al. Histologic inflammation is a risk factor for progression to colorectal neoplasia in ulcerative colitis: a cohort study. Gastroenterology. 2007; 133:1099–1105. PMID: 17919486.
Article3. Korelitz BI, Sultan K, Kothari M, Arapos L, Schneider J, Panagopoulos G. Histological healing favors lower risk of colon carcinoma in extensive ulcerative colitis. World J Gastroenterol. 2014; 20:4980–4986. PMID: 24803809.
Article4. Rubin DT, Huo D, Kinnucan JA, et al. Inflammation is an independent risk factor for colonic neoplasia in patients with ulcerative colitis: a case-control study. Clin Gastroenterol Hepatol. 2013; 11:1601–1608. PMID: 23872237.
Article5. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010; 8:336–341. PMID: 20171303.
Article6. Wells GA, Shea B, O'Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ontario, Canada: Ottawa Hospital Research Institute;2010. Accessed April 1, 2014. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.7. Chapman CG, Rubin DT. The potential for medical therapy to reduce the risk of colorectal cancer and optimize surveillance in inflammatory bowel disease. Gastrointest Endosc Clin N Am. 2014; 24:353–365. PMID: 24975527.
Article8. Cairns SR, Scholefield JH, Steele RJ, et al. Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups (update from 2002). Gut. 2010; 59:666–689. PMID: 20427401.
Article9. Nieminen U, Jussila A, Nordling S, Mustonen H, Färkkilä MA. Inflammation and disease duration have a cumulative effect on the risk of dysplasia and carcinoma in IBD: a case-control observational study based on registry data. Int J Cancer. 2014; 134:189–196. PMID: 23797639.
Article10. Laine L, Kaltenbach T, Barkun A, et al. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastroenterology. 2015; 148:639–651.e28. PMID: 25702852.
Article11. Rubin DT. Why it's time for updated U.S. colorectal cancer prevention guidelines in inflammatory bowel disease. Gastrointest Endosc. 2014; 80:849–851. PMID: 25436396.
Article12. Cleveland NK, Colman RJ, Rodriquez D, et al. Surveillance of IBD using high definition colonoscopes does not miss adenocarcinoma in patients with low-grade dysplasia. Inflamm Bowel Dis. 2016; 22:631–637. PMID: 26658214.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Crossroad between inflammation and carcinogenesis in colon
- Recent Advances in Understanding Colorectal Cancer and Dysplasia Related to Ulcerative Colitis
- A Case of Malignant Lymphoma in Patient with Ulcerative Colitis
- A Case of Non-Hodgkin's Lymphoma in Ulcerative Colitis
- Colorectal Cancer in Inflammatory Bowel Disease