Intest Res.
2016 Oct;14(4):351-357. 10.5217/ir.2016.14.4.351.
A wide variation of the quality of colonoscopy reporting system in the real clinical practice in southeastern area of Korea
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea.
- 2Division of Gastroenterology and Hepatology, Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea. dandy813@hanmail.net
- 3Division of Gastroenterology and Hepatology, Department of Internal Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea.
- 4Division of Gastroenterology and Hepatology, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea.
- 5Division of Gastroenterology, Department of Internal Medicine, Fatima Hospital of Daegu, Daegu, Korea.
- 6Division of Gastroenterology and Hepatology, Department of Internal Medicine, Dongguk University School of Medicine, Gyeongju, Korea.
- KMID: 2354953
- DOI: http://doi.org/10.5217/ir.2016.14.4.351
Abstract
- BACKGROUND/AIMS
Establishment of a colonoscopy reporting system is a prerequisite to determining and improving quality. This study aimed to investigate colonoscopists' opinions and the actual situation of a colonoscopy reporting system in a clinical practice in southeastern area of Korea and to assess the factors predictive of an inadequate reporting system.
METHODS
Physicians who performed colonoscopies in the Daegu-Gyeongbuk province of Korea and were registered with the Korean Society of Gastrointestinal Endoscopy (KSGE) were interviewed via mail about colonoscopy reporting systems using a standardized questionnaire.
RESULTS
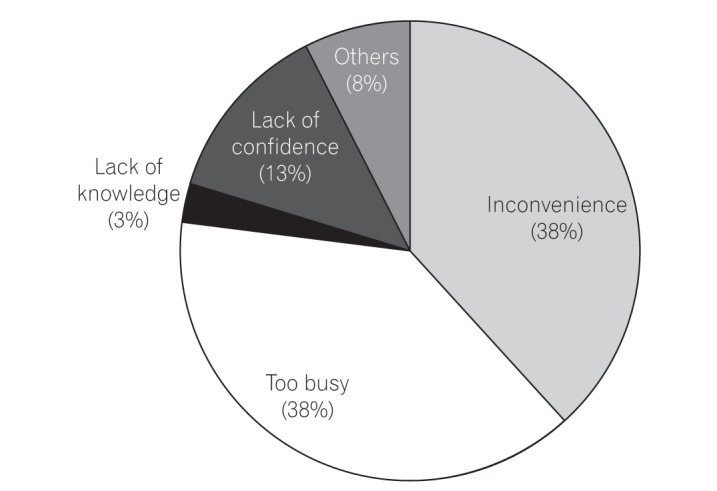
Of 181 endoscopists invited to participate, 125 responded to the questionnaires (response rate, 69%). Most responders were internists (105/125, 84%) and worked in primary clinics (88/125, 70.4%). Seventy-one specialists (56.8%) held board certifications for endoscopy from the KSGE. A median of 20 colonoscopies (interquartile range, 10-47) was performed per month. Although 88.8% of responders agreed that a colonoscopy reporting system is necessary, only 18.4% (23/125) had achieved the optimal reporting system level recommended by the Quality Assurance Task Group of the National Colorectal Cancer Roundtable. One-third of endoscopists replied that they did not use a reporting document for the main reasons of "too busy" and "inconvenience." Non-endoscopy specialists and primary care centers were independent predictive factors for failure to use a colonoscopy reporting system.
CONCLUSIONS
The quality of colonoscopy reporting systems varies widely and is considerably suboptimal in actual clinical practice settings in southeastern Korea, indicating considerable room for quality improvements in this field.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Screening strategy for colorectal cancer according to risk
Dong Soo Han
J Korean Med Assoc. 2017;60(11):893-898. doi: 10.5124/jkma.2017.60.11.893.
Reference
-
1. Lin OS, Kozarek RA, Cha JM. Impact of sigmoidoscopy and colonoscopy on colorectal cancer incidence and mortality: an evidence-based review of published prospective and retrospective studies. Intest Res. 2014; 12:268–274. PMID: 25374491.
Article2. Parente F, Marino B, Ardizzoia A, et al. Impact of a population-based colorectal cancer screening program on local health services demand in Italy: a 7-year survey in a northern province. Am J Gastroenterol. 2011; 106:1986–1993. PMID: 21670773.
Article3. Zauber AG, Winawer SJ, O'Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012; 366:687–696. PMID: 22356322.
Article4. Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010; 139:1128–1137. PMID: 20600026.
Article5. Bressler B, Paszat LF, Vinden C, Li C, He J, Rabeneck L. Colonoscopic miss rates for right-sided colon cancer: a population-based analysis. Gastroenterology. 2004; 127:452–456. PMID: 15300577.
Article6. Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009; 150:1–8. PMID: 19075198.
Article7. Brenner H, Hoffmeister M, Arndt V, Stegmaier C, Altenhofen L, Haug U. Protection from right- and left-sided colorectal neoplasms after colonoscopy: population-based study. J Natl Cancer Inst. 2010; 102:89–95. PMID: 20042716.
Article8. Barclay RL, Vicari JJ, Doughty AS, Johanson JF, Greenlaw RL. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med. 2006; 355:2533–2541. PMID: 17167136.
Article9. Kaminski MF, Regula J, Kraszewska E, et al. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med. 2010; 362:1795–1803. PMID: 20463339.
Article10. Rex DK, Petrini JL, Baron TH, et al. Quality indicators for colonoscopy. Am J Gastroenterol. 2006; 101:873–885. PMID: 16635231.
Article11. Lieberman D, Nadel M, Smith RA, et al. Standardized colonoscopy reporting and data system: report of the Quality Assurance Task Group of the National Colorectal Cancer Roundtable. Gastrointest Endosc. 2007; 65:757–766. PMID: 17466195.
Article12. Lieberman DA, Faigel DO, Logan JR, et al. Assessment of the quality of colonoscopy reports: results from a multicenter consortium. Gastrointest Endosc. 2009; 69(3 Pt 2):645–653. PMID: 19251005.
Article13. Robertson DJ, Lawrence LB, Shaheen NJ, et al. Quality of colonoscopy reporting: a process of care study. Am J Gastroenterol. 2002; 97:2651–2656. PMID: 12385455.
Article14. Li J, Nadel MR, Poppell CF, Dwyer DM, Lieberman DA, Steinberger EK. Quality assessment of colonoscopy reporting: results from a statewide cancer screening program. Diagn Ther Endosc. 2010; (2010):pii: 419796.
Article15. Cha JM. Quality improvement of gastrointestinal endoscopy in Korea: past, present, and future. Korean J Gastroenterol. 2014; 64:320–332. PMID: 25530583.
Article16. Cha JM, Han DS, Lee HL, et al. Endoscopist specialty is associated with high-quality endoscopy in Korea. Yonsei Med J. 2012; 53:310–317. PMID: 22318818.
Article17. Martînez ME, Sampliner R, Marshall JR, Bhattacharyya AK, Reid ME, Alberts DS. Adenoma characteristics as risk factors for recurrence of advanced adenomas. Gastroenterology. 2001; 120:1077–1083. PMID: 11266371.
Article18. Lee YJ, Kim ES, Park KS, et al. Inter-observer agreement in the endoscopic classification of colorectal laterally spreading tumors: a multicenter study between experts and trainees. Dig Dis Sci. 2014; 59:2550–2556. PMID: 24828919.
Article19. de Jonge V, Sint Nicolaas J, Cahen DL, et al. Quality evaluation of colonoscopy reporting and colonoscopy performance in daily clinical practice. Gastrointest Endosc. 2012; 75:98–106. PMID: 21907986.
Article20. Bressler B, Paszat LF, Chen Z, Rothwell DM, Vinden C, Rabeneck L. Rates of new or missed colorectal cancers after colonoscopy and their risk factors: a population-based analysis. Gastroenterology. 2007; 132:96–102. PMID: 17241863.
Article21. Rabeneck L, Paszat LF, Saskin R. Endoscopist specialty is associated with incident colorectal cancer after a negative colonoscopy. Clin Gastroenterol Hepatol. 2010; 8:275–279. PMID: 19879970.
Article22. Singh H, Nugent Z, Demers AA, Bernstein CN. Rate and predictors of early/missed colorectal cancers after colonoscopy in Manitoba: a population-based study. Am J Gastroenterol. 2010; 105:2588–2596. PMID: 20877348.
Article23. Aabakken L. Quality reporting: finally achievable? Endoscopy. 2014; 46:188–189. PMID: 24573729.24. Colonoscopy report. Korean Society of Gastrointestinal Endoscopy;2015. Accessed Jul 14. http://gie.or.kr/bbs/?code=file.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quality indicators in colonoscopy: the chasm between ideal and reality
- The current capacity and quality of colonoscopy in Korea
- Effectiveness of a novel artificial intelligence-assisted colonoscopy system for adenoma detection: a prospective, propensity score-matched, non-randomized controlled study in Korea
- Strategies to improve screening colonoscopy quality for the prevention of colorectal cancer
- Quality is the Key for Emerging Issues of Population-based Colonoscopy Screening