Korean J Pain.
2016 Oct;29(4):239-248. 10.3344/kjp.2016.29.4.239.
Chronic persistent post-surgical pain following staging laparotomy for carcinoma of ovary and its relationship to signal transduction genes
- Affiliations
-
- 1Department of Anesthesiology and Critical Care, University College of Medical Sciences and Guru Teg Bahadur Hospital, Shahdara, Delhi, India. geetanjalidr@yahoo.co.in
- 2Department of Biochemistry, University College of Medical Sciences and Guru Teg Bahadur Hospital, Shahdara, Delhi, India.
- KMID: 2354216
- DOI: http://doi.org/10.3344/kjp.2016.29.4.239
Abstract
- BACKGROUND
The present study was undertaken to evaluate the incidence of chronic persistent post-surgical pain (CPPP) and the role of signal transduction genes in patients undergoing staging laparotomy for carcinoma ovary.
METHODS
The present observational study was undertaken following institutional ethical committee approval and informed consent from all the participants. A total 21 patients of ASA grade I to III with age 20−70 years, scheduled for elective staging laparotomy for carcinoma ovary were included. Patients were excluded if had other causes of pain, cognitive dysfunction or chronic neurological disorders. Statistical analysis of pool data was done using SPSS version-17. For various scales like GPE, PDQ, NPSI, the visual analogue scale (VAS), global perceived effect (GPE), the pain DETECT questionnaire (PDQ), and neuropathic pain symptoms inventory (NPSI), one factor repaeted measure ANOVA applied with simple contrast with baseline as on post-operative day 1 (considered as reference and compared with subsequent time-interval), and the P values were adjusted according to "Bonferroni adjustments". In patients with CPPP, the Δct values of mRNA expressions of genes at the end of postoperative day 90 were compared with the baseline control values by one factor repeated ANOVA. P value < 0.005 significant.
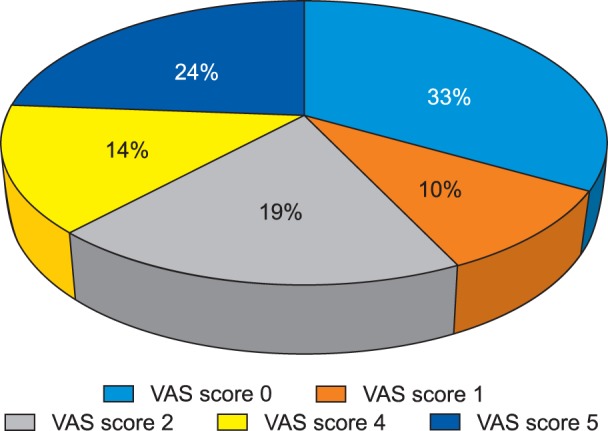
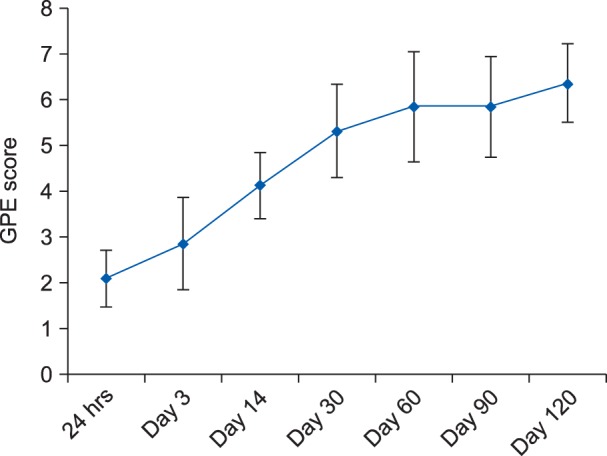
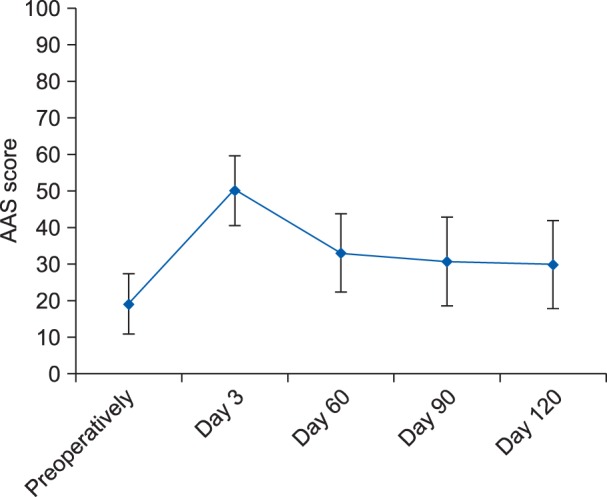
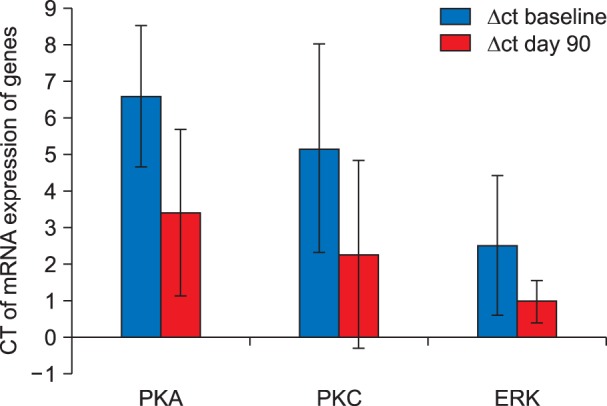
RESULTS
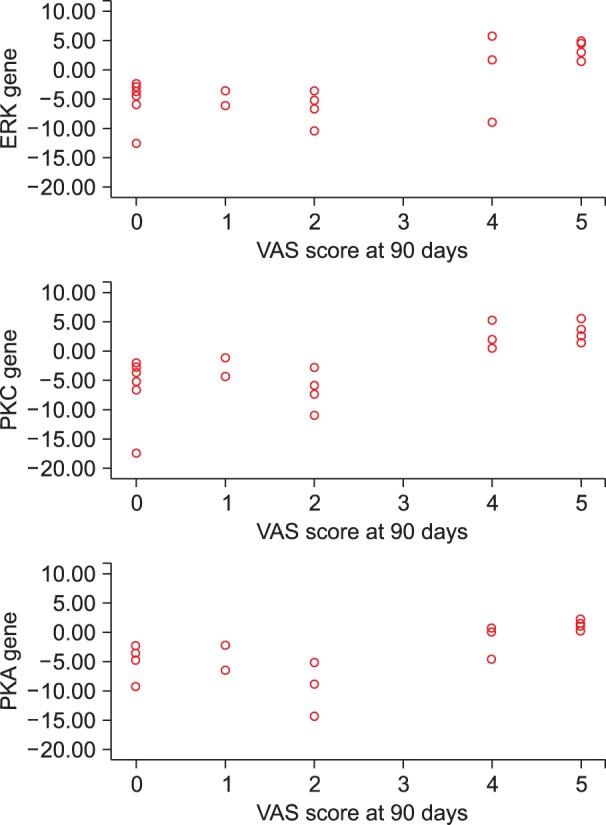
The present study demonstrates 38.1% (8 out of 21 patients) incidence of CPPP. The functional status and quality of life as were observed to be significantly diminished in all patients with chronic pain. An up-regulation in the mRNA expression of signal transduction and a positive correlation was noted between the mRNA expression of signal transduction genes and VAS score in all patients with CPPP at the end of postoperative day 90.
CONCLUSIONS
The reported incidence of CPPP in patients with carcinoma ovary was 38.1%. An up-regulation and positive correlation between mRNA expression of signal transduction genes and VAS score depicts its potential role in the pathogenesis of CPPP.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Chronic postsurgical pain: current evidence for prevention and management
Parineeta Thapa, Pramote Euasobhon
Korean J Pain. 2018;31(3):155-173. doi: 10.3344/kjp.2018.31.3.155.
Reference
-
1. Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006; 367:1618–1625. PMID: 16698416.
Article2. Kehlet H, Edward RR, Buvanendran A. Persistent postoperative pain: pathogenic mechanism and preventive strategies. Seattle (WA): International Association for the Study of Pain/IASP Press;2012. p. 133–146.3. Mikkelsen T, Werner MU, Lassen B, Kehlet H. Pain and sensory dysfunction 6 to 12 months after inguinal herniotomy. Anesth Analg. 2004; 99:146–151. PMID: 15281521.
Article4. Brandsborg B, Nikolajsen L, Kehlet H, Jensen TS. Chronic pain after hysterectomy. Acta Anaesthesiol Scand. 2008; 52:327–331. PMID: 18269384.
Article5. Brandsborg B. Pain following hysterectomy: epidemiological and clinical aspects. Dan Med J. 2012; 59:B4374. PMID: 22239844.6. Brandsborg B, Dueholm M, Nikolajsen L, Kehlet H, Jensen TS. A prospective study of risk factors for pain persisting 4 months after hysterectomy. Clin J Pain. 2009; 25:263–268. PMID: 19590472.
Article7. Scholz J, Broom DC, Youn DH, Mills CD, Kohno T, Suter MR, et al. Blocking caspase activity prevents transsynaptic neuronal apoptosis and the loss of inhibition in lamina II of the dorsal horn after peripheral nerve injury. J Neurosci. 2005; 25:7317–7323. PMID: 16093381.
Article8. Apkarian AV, Sosa Y, Sonty S, Levy RM, Harden RN, Parrish TB, et al. Chronic back pain is associated with decreased prefrontal and thalamic gray matter density. J Neurosci. 2004; 24:10410–10415. PMID: 15548656.
Article9. Zhang X, Xiao HS. Gene array analysis to determine the components of neuropathic pain signaling. Curr Opin Mol Ther. 2005; 7:532–537. PMID: 16370375.10. Li G, Lu X, Zhang S, Zhou Q, Zhang L. mTOR and Erk1/2 signaling in the cerebrospinal fluid-contacting nucleus is involved in neuropathic pain. Neurochem Res. 2015; 40:1053–1062. PMID: 25846007.
Article11. Melemedjian OK, Khoutorsky A. Translational control of chronic pain. Prog Mol Biol Transl Sci. 2015; 131:185–213. PMID: 25744674.
Article12. Fu Y, Han J, Ishola T, Scerbo M, Adwanikar H, Ramsey C, et al. PKA and ERK, but not PKC, in the amygdala contribute to pain-related synaptic plasticity and behavior. Mol Pain. 2008; 4:26. PMID: 18631385.
Article13. Bird GC, Lash LL, Han JS, Zou X, Willis WD, Neugebauer V. Protein kinase A-dependent enhanced NMDA receptor function in pain-related synaptic plasticity in rat amygdala neurones. J Physiol. 2005; 564:907–921. PMID: 15760935.
Article14. Gao YJ, Ji RR. Activation of JNK pathway in persistent pain. Neurosci Lett. 2008; 437:180–183. PMID: 18455869.
Article15. Brandsborg B, Nikolajsen L, Hansen CT, Kehlet H, Jensen TS. Risk factors for chronic pain after hysterectomy: a nationwide questionnaire and database study. Anesthesiology. 2007; 106:1003–1012. PMID: 17457133.17. Poobalan AS, Bruce J, Smith WC, King PM, Krukowski ZH, Chambers WA. A review of chronic pain after inguinal herniorrhaphy. Clin J Pain. 2003; 19:48–54. PMID: 12514456.
Article18. Wallace MS, Wallace AM, Lee J, Dobke MK. Pain after breast surgery: a survey of 282 women. Pain. 1996; 66:195–205. PMID: 8880841.
Article19. Gupta A, Gandhi K, Viscusi ER. Persistent postsurgical pain after abdominal surgery. Tech Reg Anesth Pain Manag. 2011; 15:140–146.
Article20. Obata H, Saito S, Fujita N, Fuse Y, Ishizaki K, Goto F. Epidural block with mepivacaine before surgery reduces long-term post-thoracotomy pain. Can J Anaesth. 1999; 46:1127–1132. PMID: 10608205.
Article21. Gottschalk A, Smith DS, Jobes DR, Kennedy SK, Lally SE, Noble VE, et al. Preemptive epidural analgesia and recovery from radical prostatectomy: a randomized controlled trial. JAMA. 1998; 279:1076–1082. PMID: 9546566.
Article22. Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth. 2008; 101:77–86. PMID: 18434337.
Article23. Kehlet H, Rathmell JP. Persistent postsurgical pain: the path forward through better design of clinical studies. Anesthesiology. 2010; 112:514–515. PMID: 20124977.24. Pan PH, Coghill R, Houle TT, Seid MH, Lindel WM, Parker RL, et al. Multifactorial preoperative predictors for postcesarean section pain and analgesic requirement. Anesthesiology. 2006; 104:417–425. PMID: 16508387.
Article25. Strulov L, Zimmer EZ, Granot M, Tamir A, Jakobi P, Lowenstein L. Pain catastrophizing, response to experimental heat stimuli, and post-cesarean section pain. J Pain. 2007; 8:273–279. PMID: 17113350.
Article26. Nielsen PR, Nørgaard L, Rasmussen LS, Kehlet H. Prediction of post-operative pain by an electrical pain stimulus. Acta Anaesthesiol Scand. 2007; 51:582–586. PMID: 17430320.
Article27. de Andrade DC, Ferreira KA, Nishimura CM, Yeng LT, Batista AF, de Sá K, et al. Psychometric validation of the Portuguese version of the Neuropathic Pain Symptoms Inventory. Health Qual Life Outcomes. 2011; 9:107. PMID: 22128801.
Article28. Freynhagen R, Baron R, Gockel U, Tölle TR. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006; 22:1911–1920. PMID: 17022849.
Article29. Bruce J, Poobalan AS, Smith WC, Chambers WA. Quantitative assessment of chronic postsurgical pain using the McGill Pain Questionnaire. Clin J Pain. 2004; 20:70–75. PMID: 14770045.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bone/Vascular Calcification: Signal Transduction Pathway and Calcification Related Genes
- A Case of Small Cell Carcinoma arising in a Benign Mature Cystic Teratoma of the Ovary with Metastasis to the Supraclavicular Lymph Nodes
- Signal Transduction
- Control of Signal Transduction Pathway
- Cellular Signal Transduction