J Korean Med Sci.
2015 Oct;30(Suppl 1):S88-S94. 10.3346/jkms.2015.30.S1.S88.
Retinopathy of Prematurity among Very-Low-Birth-Weight Infants in Korea: Incidence, Treatment, and Risk Factors
- Affiliations
-
- 1Department of Pediatrics, Inje University College of Medicine, Ilsan Paik Hospital, Goyang, Korea.
- 2Department of Pediatrics, Korea University College of Medicine, Seoul, Korea.
- 3Department of Pediatrics, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea. arkim@amc.seoul
- KMID: 2351141
- DOI: http://doi.org/10.3346/jkms.2015.30.S1.S88
Abstract
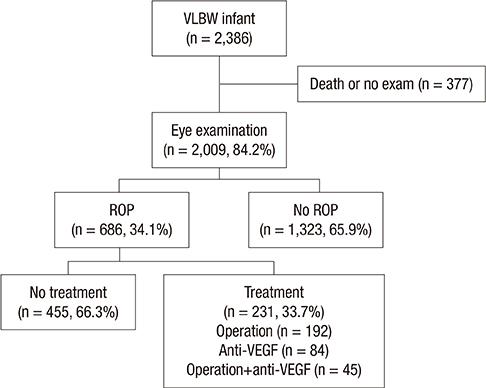
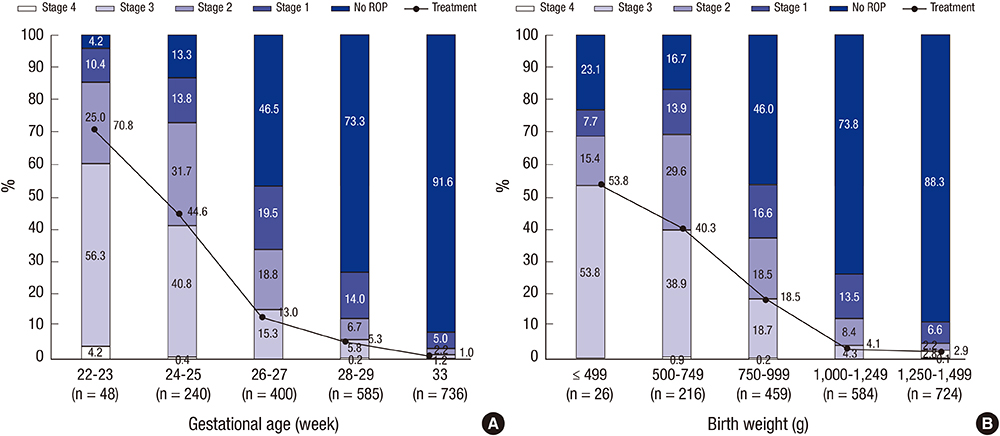
- This study was conducted to describe the incidence, risk factors, and current treatment status of retinopathy of prematurity (ROP) in very-low-birth-weight (VLBW) infants registered in the Korean Neonatal Network database. Medical records of 2,009 VLBW infants born between January 2013 and June 2014 who underwent examination by an ophthalmologist were reviewed. The total incidence of ROP was 34.1%. Of the patients, 11.6% showed ROP stage > or = 3 and 11.5% received treatment of VLBW. Among all infants who received treatment of ROP, 63.6% underwent operation only; 16.9%, anti-vascular endothelial growth factor (anti-VEGF) treatment only; and 19.5%, both operation and anti-VEGF treatment. The mean gestational age (GA) and birth weight (BW) were significantly lower and the prevalence rates of respiratory distress syndrome, patent ductus arteriosus (PDA), invasive ventilator duration, and sepsis were significantly higher in the VLBW infants with ROP than in those without ROP. In the multivariable logistic regression analysis, PDA (odd ratio [OR], 2.1; 95% confidence interval [CI], 1.11-3.79) and invasive ventilator duration (OR, 1.0; 95% CI, 1.00-1.02) were significant risk factors of ROP and ROP stage > or = 3. In conclusion, the high incidence of ROP is associated with low GA and BW, and attempt to reduce the aforementioned risk factors could reduce the incidence of ROP stage > or = 3 in VLBW infants.
MeSH Terms
-
Antibodies/therapeutic use
Birth Weight
Female
Gestational Age
Humans
Incidence
Infant
Infant Mortality
Infant, Newborn
Infant, Premature
*Infant, Very Low Birth Weight
Logistic Models
Male
Odds Ratio
Prevalence
Republic of Korea/epidemiology
Retinopathy of Prematurity/drug therapy/*epidemiology/mortality
Retrospective Studies
Risk Factors
Vascular Endothelial Growth Factor A/immunology
Antibodies
Vascular Endothelial Growth Factor A
Figure
Cited by 3 articles
-
Anti-vascular Endothelial Growth Factor Treatment of Retinopathy of Prematurity: Efficacy, Safety, and Anatomical Outcomes
Hyun Goo Kang, Eun Young Choi, Suk Ho Byeon, Sung Soo Kim, Hyoung Jun Koh, Sung Chul Lee, Min Kim
Korean J Ophthalmol. 2018;32(6):451-458. doi: 10.3341/kjo.2018.0011.Refractive Outcomes of 4-Year-old Children after Intravitreal Anti-vascular Endothelial Growth Factor versus Laser Photocoagulation for Retinopathy of Prematurity
Hyun Goo Kang, Tae Young Kim, Jinu Han, Sueng-Han Han
Korean J Ophthalmol. 2019;33(3):272-278. doi: 10.3341/kjo.2019.0011.Changes in neonatal outcomes in Korea
So Young Kim
J Korean Med Assoc. 2016;59(7):498-505. doi: 10.5124/jkma.2016.59.7.498.
Reference
-
1. Malcolm W. Retinopathy of prematurity and ophthalmologic issue. In : Malcolm WF, editor. Beyond the NICU: comprehensive care of the high-risk infant. New York: McGraw Hill Professional;2015. p. 347–365.2. Casteels I, Cassiman C, Van Calster J, Allegaert K. Educational paper: retinopathy of prematurity. Eur J Pediatr. 2012; 171:887–893.3. Fierson WM. American Academy of Pediatrics Section on Ophthalmology. American Academy of Ophthalmology. American Association for Pediatric Ophthalmology and Strabismus. American Association of Certified Orthoptists. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2013; 131:189–195.4. Goggin M, O'Keefe M. Childhood blindness in the Republic of Ireland: a national survey. Br J Ophthalmol. 1991; 75:425–429.5. Darlow BA. Retinopathy of prematurity: new developments bring concern and hope. J Paediatr Child Health. 2015; 51:765–770.6. Isaza G, Arora S, Bal M, Chaudhary V. Incidence of retinopathy of prematurity and risk factors among premature infants at a neonatal intensive care unit in Canada. J Pediatr Ophthalmol Strabismus. 2013; 50:27–32.7. Nair PM, Ganesh A, Mitra S, Ganguly SS. Retinopathy of prematurity in VLBW and extreme LBW babies. Indian J Pediatr. 2003; 70:303–306.8. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010; 126:443–456.9. Isayama T, Lee SK, Mori R, Kusuda S, Fujimura M, Ye XY, Shah PS. Canadian Neonatal Network. Comparison of mortality and morbidity of very low birth weight infants between Canada and Japan. Pediatrics. 2012; 130:e957–e965.10. Korean Neonatal Network database. Very low birth weight infants in 2013. accessed on 1 July 2014. Available at http://www.knn.or.kr/index.jsp.11. An international classification of retinopathy of prematurity: Prepared by an international committee. Br J Ophthalmol. 1984; 68:690–697.12. The International Committee for the Classification of the Late Stages of Retinopathy of Prematurity. An international classification of retinopathy of prematurity. II. The classification of retinal detachment. Arch Ophthalmol. 1987; 105:906–912.13. Statistics Canada. Births 2008 (Catalogue no. 84F0210X). accessed on 3 March 2015. Available at http://www.statcan.gc.ca/pub/84f0210x/84f0210x2008000-eng.14. Ministry of Health Labour and Welfare in Japan. Vital Statistics in 2008. accessed on 5 January 2015. Available at http://www.mhlw.go.jp/toukei/saikin/hw/jinkou/kakutei08/index.html.15. Yang CY, Lien R, Yang PH, Chu SM, Hsu JF, Fu RH, Chiang MC. Analysis of incidence and risk factors of retinopathy of prematurity among very-low-birth-weight infants in North Taiwan. Pediatr Neonatol. 2011; 52:321–326.16. Bas AY, Koc E, Dilmen U. ROP Neonatal Study Group. Incidence and severity of retinopathy of prematurity in Turkey. Br J Ophthalmol. 2015; 99:1311–1314.17. Menke MN, Framme C, Nelle M, Berger MR, Sturm V, Wolf S. Intravitreal ranibizumab monotherapy to treat retinopathy of prematurity zone II, stage 3 with plus disease. BMC Ophthalmol. 2015; 15:20.18. Mintz-Hittner HA, Kennedy KA, Chuang AZ. BEAT-ROP Cooperative Group. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011; 364:603–615.19. Darlow BA, Hutchinson JL, Simpson JM, Henderson-Smart DJ, Donoghue DA, Evans NJ. Variation in rates of severe retinopathy of prematurity among neonatal intensive care units in the Australian and New Zealand Neonatal Network. Br J Ophthalmol. 2005; 89:1592–1596.20. Bain LC, Dudley RA, Gould JB, Lee HC. Factors associated with failure to screen newborns for retinopathy of prematurity. J Pediatr. 2012; 161:819–823.21. van Sorge AJ, Termote JU, Simonsz HJ, Kerkhoff FT, van Rijn LJ, Lemmens WA, Schalij-Delfos NE. Outcome and quality of screening in a nationwide survey on retinopathy of prematurity in The Netherlands. Br J Ophthalmol. 2014; 98:1056–1060.22. Bassiouny MR. Risk factors associated with retinopathy of prematurity: a study from Oman. J Trop Pediatr. 1996; 42:355–358.23. Akkoyun I, Oto S, Yilmaz G, Gurakan B, Tarcan A, Anuk D, Akgun S, Akova YA. Risk factors in the development of mild and severe retinopathy of prematurity. J AAPOS. 2006; 10:449–453.24. Chaudhari S, Patwardhan V, Vaidya U, Kadam S, Kamat A. Retinopathy of prematurity in a tertiary care center--incidence, risk factors and outcome. Indian Pediatr. 2009; 46:219–224.25. Shah VA, Yeo CL, Ling YL, Ho LY. Incidence, risk factors of retinopathy of prematurity among very low birth weight infants in Singapore. Ann Acad Med Singapore. 2005; 34:169–178.26. Molloy CS, Anderson PJ, Anderson VA, Doyle LW. The long-term outcome of extremely preterm (<28 weeks' gestational age) infants with and without severe retinopathy of prematurity. J Neuropsychol. 2015.27. VanderVeen DK, Bremer DL, Fellows RR, Hardy RJ, Neely DE, Palmer EA, Rogers DL, Tung B, Good WV. Early Treatment for Retinopathy of Prematurity Cooperative Group. Prevalence and course of strabismus through age 6 years in participants of the early treatment for retinopathy of prematurity randomized trial. J AAPOS. 2011; 15:536–540.28. Saldir M, Sarici SU, Mutlu FM, Mocan C, Altinsoy HI, Ozcan O. An analysis of neonatal risk factors associated with the development of ophthalmologic problems at infancy and early childhood: a study of premature infants born at or before 32 weeks of gestation. J Pediatr Ophthalmol Strabismus. 2010; 47:331–337.29. Hoogerwerf A, Schalij-Delfos NE, van Schooneveld MJ, Termote JU. Incidence of retinopathy of prematurity over the last decade in the Central Netherlands. Neonatology. 2010; 98:137–142.30. Allegaert K, Casteels I, Cossey V, Devlieger H. Retinopathy of prematurity: any difference in risk factors between a high and low risk population? Eur J Ophthalmol. 2003; 13:784–788.31. George I, Mekahli D, Rayyan M, Levtchenko E, Allegaert K. Postnatal trends in creatinemia and its covariates in extremely low birth weight (ELBW) neonates. Pediatr Nephrol. 2011; 26:1843–1849.32. Larsson E, Carle-Petrelius B, Cernerud G, Ots L, Wallin A, Holmström G. Incidence of ROP in two consecutive Swedish population based studies. Br J Ophthalmol. 2002; 86:1122–1126.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical analysis of retinopathy of prematurity
- Incidence and Risk Factors of Retinopathy of Prematurity in Extremely Low Birth Weight and Very Low Birth Weight Infants
- A Clinical Study of Retinopathy of Prematurity
- Clinical Study of Prematurity and Low Birth Weight Infants
- A Clinical Study of Retinopathy of Prematurity