Yonsei Med J.
2015 Nov;56(6):1545-1551. 10.3349/ymj.2015.56.6.1545.
Circulating Anti-Elastin Antibody Levels and Arterial Disease Characteristics: Associations with Arterial Stiffness and Atherosclerosis
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. shl1106@yuhs.ac
- 2Graduate School of Medical Science and Engineering, Korea Advanced Institute of Science and Technology, Daejeon, Korea. seung-hyo.lee@kaist.ac.kr
- 3Cardiovascular Research Institute, Yonsei University Health System, Seoul, Korea.
- KMID: 2345881
- DOI: http://doi.org/10.3349/ymj.2015.56.6.1545
Abstract
- PURPOSE
Elastin is a major arterial structural protein, and elastin-derived peptides are related to arterial change. We previously reported on a novel assay developed using aortic elastin peptides; however, its clinical implications remain unclear. In this study, we assessed whether anti-elastin antibody titers reflect the risk of coronary artery disease (CAD) or its characteristics.
MATERIALS AND METHODS
We included 174 CAD patients and 171 age- and sex-matched controls. Anti-elastin antibody titers were quantified by enzyme-linked immunosorbent assay. Parameters of arterial stiffness, including the augmentation index (AI) and heart-to-femoral pulse wave velocity (hfPWV), were measured non-invasively. The clinical and angiographic characteristics of CAD patients were also evaluated. Associations between anti-elastin levels and vascular characteristics were examined by linear regression analysis.
RESULTS
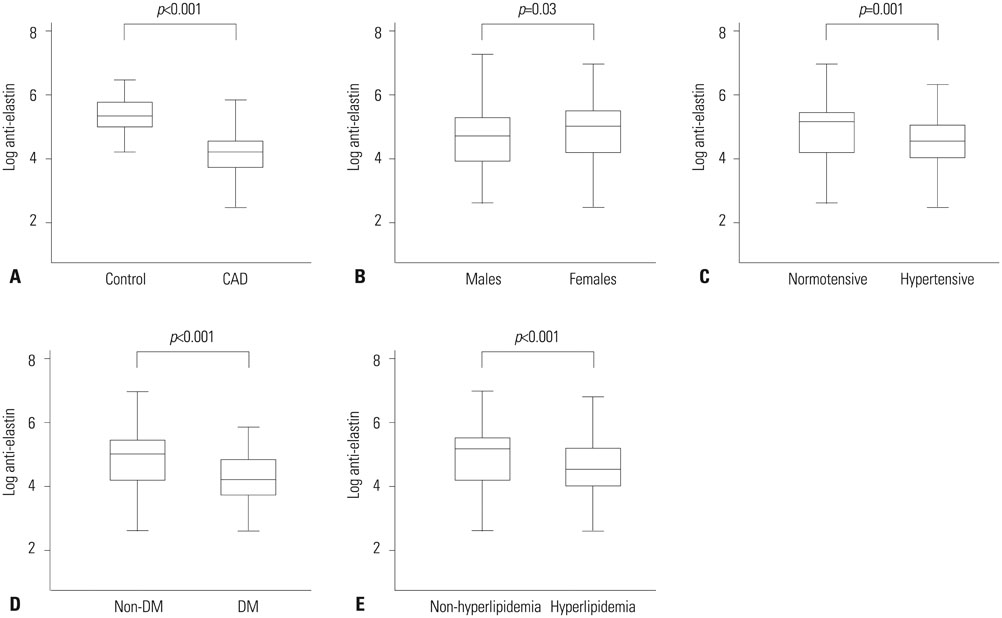
The median blood level of anti-elastin was significantly lower in the CAD group than in the controls [197 arbitrary unit (a.u.) vs. 63 a.u., p<0.001]. Levels of anti-elastin were significantly lower in men and in subjects with hypertension, diabetes mellitus, hyperlipidemia, or high hfPWV. Nevertheless, anti-elastin levels were not dependent on atherothrombotic events or the angiographic severity of CAD. In a multivariate analysis, male sex (beta=-0.38, p<0.001), diabetes mellitus (beta=-0.62, p<0.001), hyperlipidemia (beta=-0.29, p<0.001), and AI (beta=-0.006, p=0.02) were ultimately identified as determinants of anti-elastin levels.
CONCLUSION
Lower levels of anti-elastin are related to CAD. The association between antibody titers and CAD is linked to arterial stiffness rather than the advancement of atherosclerosis.
MeSH Terms
-
Aged
Angiography
Antibodies/*blood
Atherosclerosis/*blood/immunology
Coronary Artery Disease/blood/*immunology
Elastin/*blood/immunology
Enzyme-Linked Immunosorbent Assay
Female
Humans
Hyperlipidemias
Hypertension/complications
Male
Middle Aged
Pulse Wave Analysis
Vascular Stiffness/*immunology/physiology
Antibodies
Elastin
Figure
Reference
-
1. Zieman SJ, Melenovsky V, Kass DA. Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol. 2005; 25:932–943.
Article2. Smith ER, Tomlinson LA, Ford ML, McMahon LP, Rajkumar C, Holt SG. Elastin degradation is associated with progressive aortic stiffening and all-cause mortality in predialysis chronic kidney disease. Hypertension. 2012; 59:973–978.
Article3. Maurice P, Blaise S, Gayral S, Debelle L, Laffargue M, Hornebeck W, et al. Elastin fragmentation and atherosclerosis progression: the elastokine concept. Trends Cardiovasc Med. 2013; 23:211–221.
Article4. Maclay JD, McAllister DA, Rabinovich R, Haq I, Maxwell S, Hartland S, et al. Systemic elastin degradation in chronic obstructive pulmonary disease. Thorax. 2012; 67:606–612.
Article5. Fülöp T Jr, Wei SM, Robert L, Jacob MP. Determination of elastin peptides in normal and arteriosclerotic human sera by ELISA. Clin Physiol Biochem. 1990; 8:273–282.6. Baydanoff S, Nicoloff G, Alexiev C. Age-related changes in anti-elastin antibodies in serum from normal and atherosclerotic subjects. Atherosclerosis. 1987; 63:267–271.
Article7. Hong YJ, Kim J, Oh BR, Lee YJ, Lee EY, Lee EB, et al. Serum elastin-derived peptides and anti-elastin antibody in patients with systemic sclerosis. J Korean Med Sci. 2012; 27:484–488.
Article8. Baydanoff S, Nicoloff G, Alexiev C. Age-related changes in the level of circulating elastin-derived peptides in serum from normal and atherosclerotic subjects. Atherosclerosis. 1987; 66:163–168.
Article9. Skjøt-Arkil H, Clausen RE, Rasmussen LM, Wang W, Wang Y, Zheng Q, et al. Acute Myocardial Infarction and Pulmonary Diseases Result in Two Different Degradation Profiles of Elastin as Quantified by Two Novel ELISAs. PLoS One. 2013; 8:e60936.
Article10. Tzvetanov P, Hegde V, Al-Hashel JY, Atanasova M, Sohal AP, Rousseff RT. Abnormal levels of serum anti-elastin antibodies in patients with symptomatic carotid stenosis. Clin Neurol Neurosurg. 2014; 116:9–12.
Article11. Wilkinson IB, Fuchs SA, Jansen IM, Spratt JC, Murray GD, Cockcroft JR, et al. Reproducibility of pulse wave velocity and augmentation index measured by pulse wave analysis. J Hypertens. 1998; 16(12 Pt 2):2079–2084.
Article12. Lee SH, Choi S, Jung JH, Lee N. Effects of atrial fibrillation on arterial stiffness in patients with hypertension. Angiology. 2008; 59:459–463.
Article13. Lee SH, Goswami S, Grudo A, Song LZ, Bandi V, Goodnight-White S, et al. Antielastin autoimmunity in tobacco smoking-induced emphysema. Nat Med. 2007; 13:567–569.
Article14. Sukhova GK, Shi GP, Simon DI, Chapman HA, Libby P. Expression of the elastolytic cathepsins S and K in human atheroma and regulation of their production in smooth muscle cells. J Clin Invest. 1998; 102:576–583.
Article15. Cheng XW, Huang Z, Kuzuya M, Okumura K, Murohara T. Cysteine protease cathepsins in atherosclerosis-based vascular disease and its complications. Hypertension. 2011; 58:978–986.
Article16. Senior RM, Griffin GL, Mecham RP, Wrenn DS, Prasad KU, Urry DW. Val-Gly-Val-Ala-Pro-Gly, a repeating peptide in elastin, is chemotactic for fibroblasts and monocytes. J Cell Biol. 1984; 99:870–874.
Article17. Ruseva B, Atanasova M, Georgieva M, Shumkov N, Laleva P. Effects of selenium on the vessel walls and anti-elastin antibodies in spontaneously hypertensive rats. Exp Biol Med (Maywood). 2012; 237:160–166.
Article18. Atanasova M, Konova E, Georgieva M, Dimitrova A, Coquand-Gandit M, Faury G, et al. Age-related changes of anti-elastin antibodies in senescence-accelerated mice. Gerontology. 2010; 56:310–318.
Article19. Laugesen E, Høyem P, Christiansen JS, Knudsen ST, Hansen KW, Argraves WS, et al. Plasma levels of the arterial wall protein fibulin-1 are associated with carotid-femoral pulse wave velocity: a cross-sectional study. Cardiovasc Diabetol. 2013; 12:107.
Article20. Podet EJ, Shaffer DR, Gianturco SH, Bradley WA, Yang CY, Guyton JR. Interaction of low density lipoproteins with human aortic elastin. Arterioscler Thromb. 1991; 11:116–122.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum to "Circulating Anti-Elastin Antibody Levels and Arterial Disease Characteristics: Associations with Arterial Stiffness and Atherosclerosis" by Lee SH, et al. (Yonsei Med J 2015;56:1545-51.)
- Measurements of Arterial Stiffness: Methodological Aspects
- Arterial stiffness and hypertension
- Association Between Arterial Stiffness and Carotid Atherosclerosis in the Elderly
- Arterial Ageing