Korean J Ophthalmol.
2014 Aug;28(4):292-297.
Biometric Risk Factors for Corneal Neovascularization Associated with Hydrogel Soft Contact Lens Wear in Korean Myopic Patients
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. kmk9@snu.ac.kr
- 2Laboratory of Ocular Regenerative Medicine and Immunology, Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea.
Abstract
- PURPOSE
To investigate the biometric risk factors for corneal surface complications associated with hydrogel soft contact lens (SCL) fitting in myopic patients in Korea.
METHODS
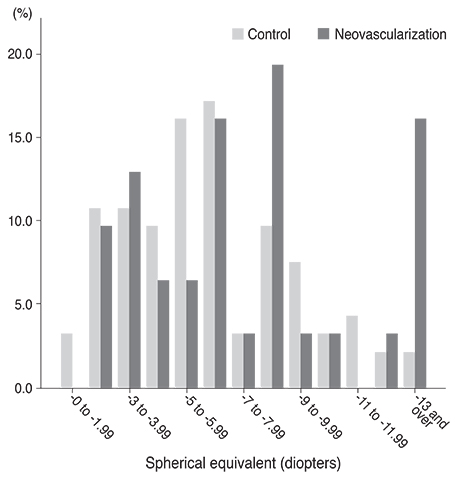
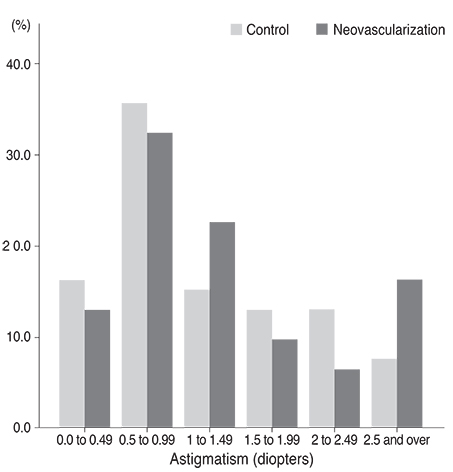
This is a retrospective case-control study. The records of 124 subjects (124 eyes) who wore SCLs on a daily basis were reviewed. Thirty-one patients (31 eyes) who were diagnosed with corneal neovascularization (NV) while wearing SCLs were included in the complication group. Ninety-three age- and sex-matched patients (93 eyes) who wore SCLs, who did not have corneal NV and who visited our clinic for correction of refractive errors were included in the control group. The degree of spherical equivalent, astigmatism and corneal base curve radius (BCR) were compared in both groups.
RESULTS
Patients with NV exhibited poorer best corrected visual acuity and more myopia than controls (p = 0.008 and 0.006, respectively). In univariate analysis, highly myopic patients (-9 diopters [D] or higher) were more likely to experience NV (odds ratio [OR], 2.232; 95% confidence interval [CI], 1.602 to 3.105). High astigmatism (> or =2 D) increased the risk of complications (OR, 2.717; 95% CI, 1.141 to 6.451). Steep cornea, in which BCR was <7.5 mm, also raised the risk of complications (OR, 4.000; 95% CI, 1.661 to 9.804). Flat cornea was not a risk factor for the development of NV.
CONCLUSIONS
High myopia, high astigmatism, and steep cornea seemed to be risk factors in the development of corneal NV in SCL wearers.
MeSH Terms
Figure
Reference
-
1. Robertson DM, Petroll WM, Jester JV, Cavanagh HD. The role of contact lens type, oxygen transmission, and care-related solutions in mediating epithelial homeostasis and pseudomonas binding to corneal cells: an overview. Eye Contact Lens. 2007; 33:394–398.2. Chalmers RL, Keay L, Long B, et al. Risk factors for contact lens complications in US clinical practices. Optom Vis Sci. 2010; 87:725–735.3. Jones LW, Jones DA. Non-inflammatory corneal complications of contact lens wear. Cont Lens Anterior Eye. 2001; 24:73–79.4. Markoulli M, Papas E, Cole N, Holden B. Corneal erosions in contact lens wear. Cont Lens Anterior Eye. 2012; 35:2–8.5. Teo L, Lim L, Tan DT, et al. A survey of contact lens complications in Singapore. Eye Contact Lens. 2011; 37:16–19.6. Chalmers RL, Wagner H, Mitchell GL, et al. Age and other risk factors for corneal infiltrative and inflammatory events in young soft contact lens wearers from the Contact Lens Assessment in Youth (CLAY) study. Invest Ophthalmol Vis Sci. 2011; 52:6690–6696.7. Dart JK, Radford CF, Minassian D, et al. Risk factors for microbial keratitis with contemporary contact lenses: a case-control study. Ophthalmology. 2008; 115:1647–1654.8. Nichols JJ, Sinnott LT. Tear film, contact lens, and patient factors associated with corneal staining. Invest Ophthalmol Vis Sci. 2011; 52:1127–1137.9. Ozkan J, Mandathara P, Krishna P, et al. Risk factors for corneal inflammatory and mechanical events with extended wear silicone hydrogel contact lenses. Optom Vis Sci. 2010; 87:847–853.10. Ramamoorthy P, Sinnott LT, Nichols JJ. Treatment, material, care, and patient-related factors in contact lens-related dry eye. Optom Vis Sci. 2008; 85:764–772.11. Richdale K, Sinnott LT, Skadahl E, Nichols JJ. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. 2007; 26:168–174.12. Stapleton F, Edwards K, Keay L, et al. Risk factors for moderate and severe microbial keratitis in daily wear contact lens users. Ophthalmology. 2012; 119:1516–1521.13. Martin R. Corneal conjunctivalisation in long-standing contact lens wearers. Clin Exp Optom. 2007; 90:26–30.14. Jeng BH, Halfpenny CP, Meisler DM, Stock EL. Management of focal limbal stem cell deficiency associated with soft contact lens wear. Cornea. 2011; 30:18–23.15. Morgan PB, Brennan NA, Maldonado-Codina C, et al. Central and peripheral oxygen transmissibility thresholds to avoid corneal swelling during open eye soft contact lens wear. J Biomed Mater Res B Appl Biomater. 2010; 92:361–365.16. Papas E. On the relationship between soft contact lens oxygen transmissibility and induced limbal hyperaemia. Exp Eye Res. 1998; 67:125–131.17. Wagner H, Chalmers RL, Mitchell GL, et al. Risk factors for interruption to soft contact lens wear in children and young adults. Optom Vis Sci. 2011; 88:973–980.18. Sutton-Tyrrell K. Assessing bias in case-control studies. Proper selection of cases and controls. Stroke. 1991; 22:938–942.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corneal Neovascularization and Corneal Hypesthesia as Contact Lens Complications
- Complications of Contact Lens Wear After Radial Keratotomy in an Animal Model
- Characteristics of Silicone Hydrogel Contact Lenses Commercially Available in Korea
- The Effect of Corneal Edema on Corneal Topography
- The Effects of Cheap Tinted Contact Lenses on Corneal Swelling and Ocular Surface Inflammation