J Korean Med Sci.
2015 Oct;30(10):1439-1445. 10.3346/jkms.2015.30.10.1439.
Clinico-pathological Analysis of the Lungs from Patients with Lung Transplantation in a Single Institute in Korea
- Affiliations
-
- 1Department of Pathology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. doohyun@snu.ac.kr
- 2Department of Thoracic Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 3Xenotransplantation Research Center, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 4Transplantation Research Institute, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Biomedical Sciences, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2344176
- DOI: http://doi.org/10.3346/jkms.2015.30.10.1439
Abstract
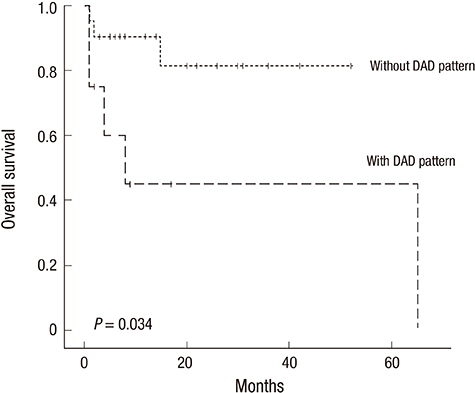
- Recently, the numbers of lung transplantation (LT) has been increased in Korea. However, post-LT outcome has not been successful in all patients, which may be partially affected by the primary lung disease. Therefore comprehensive understanding in original pathological diagnosis of patients with LT would be needed for achieving better clinical outcome. To address this issue, we performed clinico-pathological analysis of the explanted lungs from 29 patients who underwent LT over a 9-yr period in Seoul National University Hospital. Among them, 26 patients received single (1/26) or double (25/26) LT, while heart-lung transplantation was performed in 3 patients. The final clinico-pathological diagnoses were idiopathic pulmonary fibrosis/usual interstitial pneumonia (UIP) (n = 6), acute interstitial pneumonia (AIP)/diffuse alveolar damage (DAD) (n = 4), AIP/non-specific interstitial pneumonia with DAD (n = 1), collagen vascular disease-related interstitial lung disease (CVD-ILD)/DAD (n = 3), CVD-ILD/UIP (n = 1), lymphangioleiomyomatosis (n = 1), bronchiectasis (n = 4), pulmonary arterial hypertension (n = 2), tuberculosis (n = 1), bronchiolitis obliterans (BO) (n = 1), and lung cancer (n = 1). Moreover, 4 patients who had chemotherapy and hematopoietic stem cell transplantation due to hematologic malignancy showed unclassifiable interstitial pneumonia with extensive fibrosis in the lungs. Our study demonstrates that pathology of the explanted lungs from Korean patients with LT is different from that of other countries except for interstitial lung disease and bronchiectasis, which may be helpful for optimization of selecting LT candidates for Korean patients.
Keyword
MeSH Terms
-
Acinetobacter baumannii/isolation & purification
Adolescent
Adult
Aged
Bronchiectasis/*pathology
Child
Female
Humans
Idiopathic Pulmonary Fibrosis/*pathology
Lung/microbiology/*pathology
Lung Diseases, Interstitial/*pathology
*Lung Transplantation
Male
Middle Aged
Republic of Korea
Treatment Outcome
Vancomycin-Resistant Enterococci/isolation & purification
Young Adult
Figure
Reference
-
1. Yusen RD, Edwards LB, Kucheryavaya AY, Benden C, Dipchand AI, Dobbels F, Goldfarb SB, Levvey BJ, Lund LH, Meiser B, et al. International Society for Heart and Lung Transplantation. The registry of the International Society for Heart and Lung Transplantation: thirty-first adult lung and heart-lung transplant report--2014; focus theme: retransplantation. J Heart Lung Transplant. 2014; 33:1009–1024.2. Haam SJ, Lee DY, Paik HC. An overview of lung transplantation in Korea. Transplant Proc. 2008; 40:2620–2622.3. Korean Network for Organ Sharing (KONOS). KONOS 2013 statistical yearbook. accessed on 10 July 2014. Available at http://www.konos.go.kr/konosis/.4. Stewart S, McNeil K, Nashef SA, Wells FC, Higenbottam TW, Wallwork J. Audit of referral and explant diagnoses in lung transplantation: a pathologic study of lungs removed for parenchymal disease. J Heart Lung Transplant. 1995; 14:1173–1186.5. Calabrese F, Alessandrini L, Loy M, Marulli G, Balestro E, Perissinotto E, Valente M, Rea F. Comparison between referral diagnosis of patients requiring transplantation and pathologic diagnosis of native lungs. J Heart Lung Transplant. 2009; 28:1135–1140.6. Sato M, Okada Y, Oto T, Minami M, Shiraishi T, Nagayasu T, Yoshino I, Chida M, Okumura M, Date H, et al. Japanese Society of Lung and Heart-Lung Transplantation. Registry of the Japanese Society of Lung and Heart-Lung Transplantation: official Japanese lung transplantation report, 2014. Gen Thorac Cardiovasc Surg. 2014; 62:594–601.7. Orens JB, Estenne M, Arcasoy S, Conte JV, Corris P, Egan JJ, Egan T, Keshavjee S, Knoop C, Kotloff R, et al. Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. International guidelines for the selection of lung transplant candidates: 2006 update--a consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2006; 25:745–755.8. Avnon LS, Pikovsky O, Sion-Vardy N, Almog Y. Acute interstitial pneumonia-Hamman-Rich syndrome: clinical characteristics and diagnostic and therapeutic considerations. Anesth Analg. 2009; 108:232–237.9. Vourlekis JS, Brown KK, Cool CD, Young DA, Cherniack RM, King TE, Schwarz MI. Acute interstitial pneumonitis. Case series and review of the literature. Medicine (Baltimore). 2000; 79:369–378.10. Paloyan EB, Swinnen LJ, Montoya A, Lonchyna V, Sullivan HJ, Garrity E. Lung transplantation for advanced bronchioloalveolar carcinoma confined to the lungs. Transplantation. 2000; 69:2446–2448.11. Garver RI Jr, Zorn GL, Wu X, McGiffin DC, Young KR Jr, Pinkard NB. Recurrence of bronchioloalveolar carcinoma in transplanted lungs. N Engl J Med. 1999; 340:1071–1074.12. de Perrot M, Chernenko S, Waddell TK, Shargall Y, Pierre AF, Hutcheon M, Keshavjee S. Role of lung transplantation in the treatment of bronchogenic carcinomas for patients with end-stage pulmonary disease. J Clin Oncol. 2004; 22:4351–4356.13. Camus P, Fanton A, Bonniaud P, Camus C, Foucher P. Interstitial lung disease induced by drugs and radiation. Respiration. 2004; 71:301–326.14. Watkins TR, Chien JW, Crawford SW. Graft versus host-associated pulmonary disease and other idiopathic pulmonary complications after hematopoietic stem cell transplant. Semin Respir Crit Care Med. 2005; 26:482–489.15. Miyagawa-Hayashino A, Sonobe M, Kubo T, Yoshizawa A, Date H, Manabe T. Non-specific interstitial pneumonia as a manifestation of graft-versus-host disease following pediatric allogeneic hematopoietic stem cell transplantation. Pathol Int. 2010; 60:137–142.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ex Vivo Lung Perfusion in Lung Transplantation
- Lung Cancer in the Explanted Lung of the Recipient in Lung Transplantation
- Patient management for thoracic organ donor candidates: the lung transplantation team’s view
- Donor Selection, Management, and Procurement for Lung Transplantation
- Histopathological changes in the lungs of rats instilled with Korean chrysotile