Cancer Res Treat.
2016 Jul;48(3):1020-1029. 10.4143/crt.2015.264.
Effect of Helicobacter pylori Eradication on Long-Term Survival after Distal Gastrectomy for Gastric Cancer
- Affiliations
-
- 1Center for Gastric Cancer, National Cancer Center, Korea. cij1224@hanmail.net
- KMID: 2344075
- DOI: http://doi.org/10.4143/crt.2015.264
Abstract
- PURPOSE
Negative Helicobacter pylori status has been identified as a poor prognostic factor for survival in gastric cancer (GC) patients who underwent surgery. The aim of this study was to examine the effect of H. pylori eradication on long-term outcomes after distal gastrectomy for GC.
MATERIALS AND METHODS
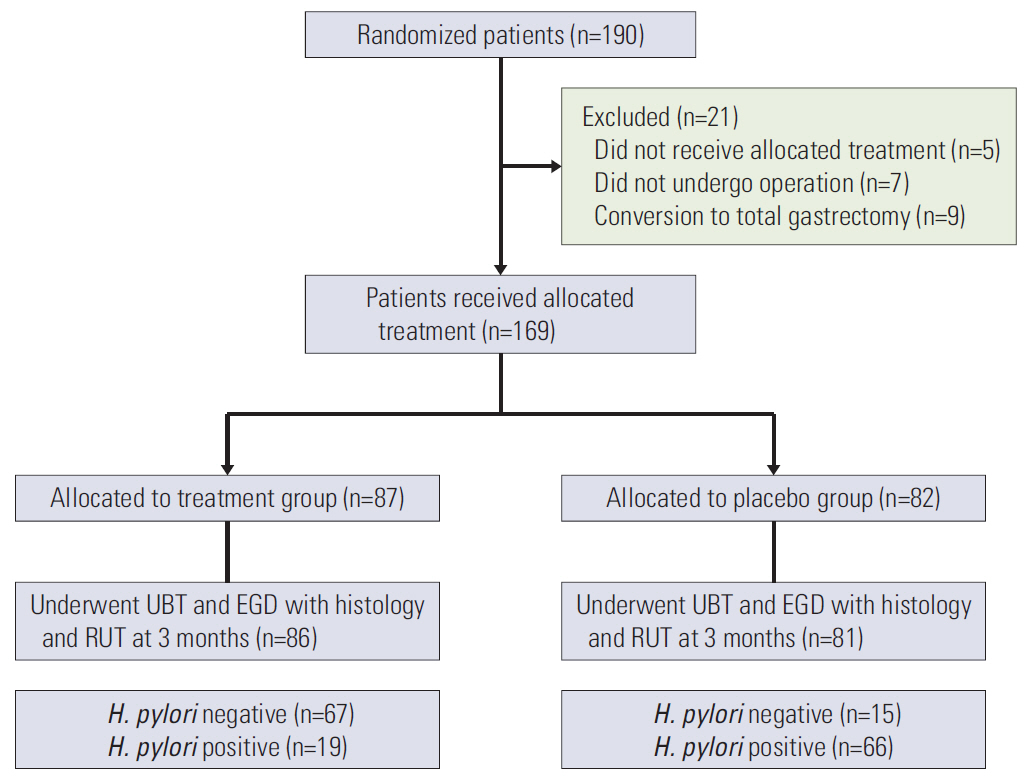
We analyzed the survival of 169 distal GC patients enrolled in a prospective randomized trial evaluating histologic changes of gastric mucosa after H. pylori eradication in the remnant stomach. The outcomes measured were overall survival (OS) and GC recurrence rates.
RESULTS
The median follow-up duration was 9.4 years. In the modified intention-to-treat analysis including patients who underwent H. pylori treatment (n=87) or placebo (n=82), 5-year OS rates were 98.9% in the treatment group and 91.5% in the placebo group, and Kaplan-Meier analysis showed no significant difference in OS (p=0.957) between groups. In multivariate analysis, no difference in overall mortality was observed between groups (adjusted hazard ratio [aHR] for H. pylori treatment, 0.75; p=0.495) or H. pylori-eradicated status (aHR for positive H. pylori status, 1.16; p=0.715), while old age, male sex, and advanced stage ≥ IIIa were independent risk factors. Six patients in the treatment group (6.9%) and seven patients in the placebo group (8.5%) had GC recurrences, and GC recurrence rates were not different according to H. pylori treatment (5-year GC recurrence rates, 4.6% in the treatment group vs. 8.5% in the placebo group; p=0.652).
CONCLUSION
H. pylori eradication for GC patients who underwent distal gastrectomy did not compromise long-term survival after surgery.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Choi IJ. Current evidence of effects of Helicobacter pylori eradication on prevention of gastric cancer. Korean J Intern Med. 2013; 28:525–37.2. Meimarakis G, Winter H, Assmann I, Kopp R, Lehn N, Kist M, et al. Helicobacter pylori as a prognostic indicator after curative resection of gastric carcinoma: a prospective study. Lancet Oncol. 2006; 7:211–22.
Article3. Marrelli D, Pedrazzani C, Berardi A, Corso G, Neri A, Garosi L, et al. Negative Helicobacter pylori status is associated with poor prognosis in patients with gastric cancer. Cancer. 2009; 115:2071–80.4. Kang SY, Han JH, Ahn MS, Lee HW, Jeong SH, Park JS, et al. Helicobacter pylori infection as an independent prognostic factor for locally advanced gastric cancer patients treated with adjuvant chemotherapy after curative resection. Int J Cancer. 2012; 130:948–58.
Article5. Yoon H, Kim N, Lee HS, Shin CM, Park YS, Lee DH, et al. Helicobacter pylori-negative gastric cancer in South Korea: incidence and clinicopathologic characteristics. Helicobacter. 2011; 16:382–8.
Article6. Qiu HB, Zhang LY, Keshari RP, Wang GQ, Zhou ZW, Xu DZ, et al. Relationship between H. pylori infection and clinicopathological features and prognosis of gastric cancer. BMC Cancer. 2010; 10:374.
Article7. Kwak HW, Choi IJ, Cho SJ, Lee JY, Kim CG, Kook MC, et al. Characteristics of gastric cancer according to Helicobacter pylori infection status. J Gastroenterol Hepatol. 2014; 29:1671–7.
Article8. Fukase K, Kato M, Kikuchi S, Inoue K, Uemura N, Okamoto S, et al. Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an open-label, randomised controlled trial. Lancet. 2008; 372:392–7.
Article9. Kim YI, Choi IJ, Kook MC, Cho SJ, Lee JY, Kim CG, et al. The association between Helicobacter pylori status and incidence of metachronous gastric cancer after endoscopic resection of early gastric cancer. Helicobacter. 2014; 19:194–201.10. Cho SJ, Choi IJ, Kook MC, Yoon H, Park S, Kim CG, et al. Randomised clinical trial: the effects of Helicobacter pylori eradication on glandular atrophy and intestinal metaplasia after subtotal gastrectomy for gastric cancer. Aliment Pharmacol Ther. 2013; 38:477–89.11. Hwang JJ, Lee DH, Kang KK, Lee AR, Yoon H, Shin CM, et al. Eradication rate and histological changes after Helicobacter pylori eradication treatment in gastric cancer patients following subtotal gastrectomy. World J Gastroenterol. 2015; 21:3936–43.12. Sobin LH, Wittekind C. TNM classification of malignant tumours. 6th ed. New York: Wiley-Liss;2002.13. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–23.14. Matsuo T, Ito M, Takata S, Tanaka S, Yoshihara M, Chayama K. Low prevalence of Helicobacter pylori-negative gastric cancer among Japanese. Helicobacter. 2011; 16:415–9.
Article15. Cancer Genome Atlas Research Network. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014; 513:202–9.16. Hanada K, Graham DY. Helicobacter pylori and the molecular pathogenesis of intestinal-type gastric carcinoma. Expert Rev Anticancer Ther. 2014; 14:947–54.17. Hobsley M, Tovey FI, Holton J. Helicobacter pylori and gastric cancer: neither friend nor foe. Gastroenterology. 2007; 132:2076.
Article18. Lin YS, Chen MJ, Shih SC, Bair MJ, Fang CJ, Wang HY. Management of Helicobacter pylori infection after gastric surgery. World J Gastroenterol. 2014; 20:5274–82.19. Lee Y, Tokunaga A, Tajiri T, Masuda G, Okuda T, Fujita I, et al. Inflammation of the gastric remnant after gastrectomy: mucosal erythema is associated with bile reflux and inflammatory cellular infiltration is associated with Helicobacter pylori infection. J Gastroenterol. 2004; 39:520–6.
Article20. Lynch DA, Mapstone NP, Clarke AM, Jackson P, Dixon MF, Quirke P, et al. Cell proliferation in the gastric corpus in Helicobacter pylori associated gastritis and after gastric resection. Gut. 1995; 36:351–3.
Article21. Sakakibara M, Ando T, Ishiguro K, Maeda O, Watanabe O, Hirayama Y, et al. Usefulness of Helicobacter pylori eradication for precancerous lesions of the gastric remnant. J Gastroenterol Hepatol. 2014; 29 Suppl 4:60–4.
Article22. Jung DH, Kim JH, Chung HS, Park JC, Shin SK, Lee SK, et al. Helicobacter pylori eradication on the prevention of metachronous lesions after endoscopic resection of gastric neoplasm: a meta-analysis. PLoS One. 2015; 10:e0124725.
Article23. Eom BW, Lee JH, Choi IJ, Kook MC, Nam BH, Ryu KW, et al. Pretreatment risk factors for multiple gastric cancer and missed lesions. J Surg Oncol. 2012; 105:813–7.
Article24. Nasu J, Doi T, Endo H, Nishina T, Hirasaki S, Hyodo I. Characteristics of metachronous multiple early gastric cancers after endoscopic mucosal resection. Endoscopy. 2005; 37:990–3.
Article25. Bair MJ, Wu MS, Chang WH, Shih SC, Wang TE, Chen CJ, et al. Spontaneous clearance of Helicobacter pylori colonization in patients with partial gastrectomy: correlates with operative procedures and duration after operation. J Formos Med Assoc. 2009; 108:13–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Helicobacter pylori Eradication in Patients Undergoing Gastrectomy: Diagnosis and Therapy
- Approach to Patients after Successful Eradication of Helicobacter pylori
- Effectiveness of Helicobacter pylori Eradication before Endoscopic Resection
- Helicobacter pylori Eradication and Gastric Cancer Prevention
- Is Helicobacter Pylori Eradication Beneficial in Terms of Preventing Gastric Cancer and Increasing Survival?