J Korean Ophthalmol Soc.
2008 Sep;49(9):1483-1490.
Clinical Features in Korean Patients with Sarcoid Uveitis
- Affiliations
-
- 1Department of Ophthalmology, Seoul Metropolitan Boramae Hospital, Seoul, Korea.
- 2Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. hgonyu@snu.ac.kr
- 3Medical Research Center, Seoul National University, Seoul, Korea.
Abstract
-
PURPOSE: To investigate the clinical features of Korean patients with sarcoid uveitis.
METHODS
The medical records of patients with endogenous uveitis who were recruited from the uveitis clinic at Seoul National University Hospital were reviewed. Sex, age at presentation, ocular symptoms and signs, treatment, complications, and the rate of recurrence were analyzed.
RESULTS
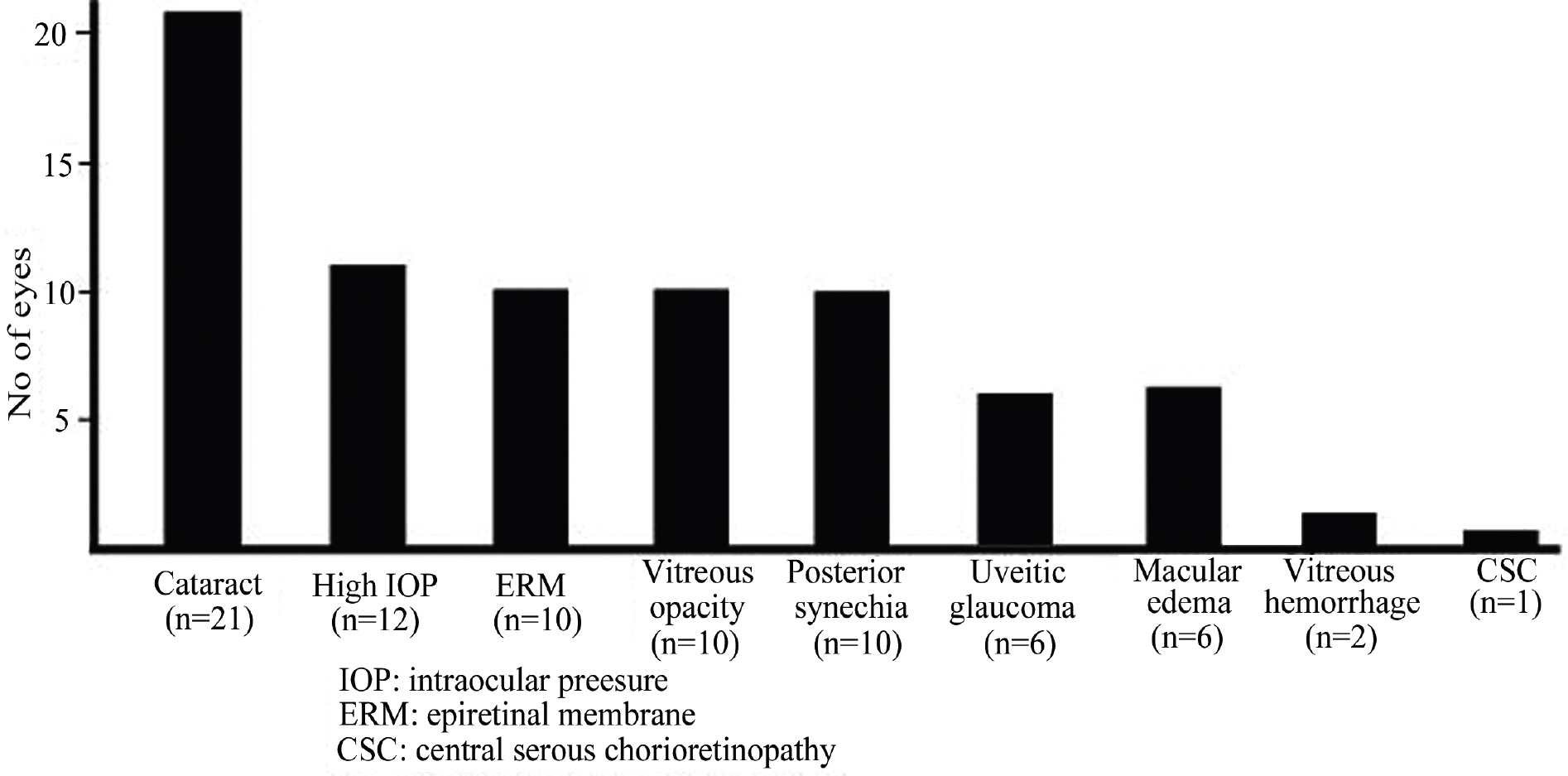
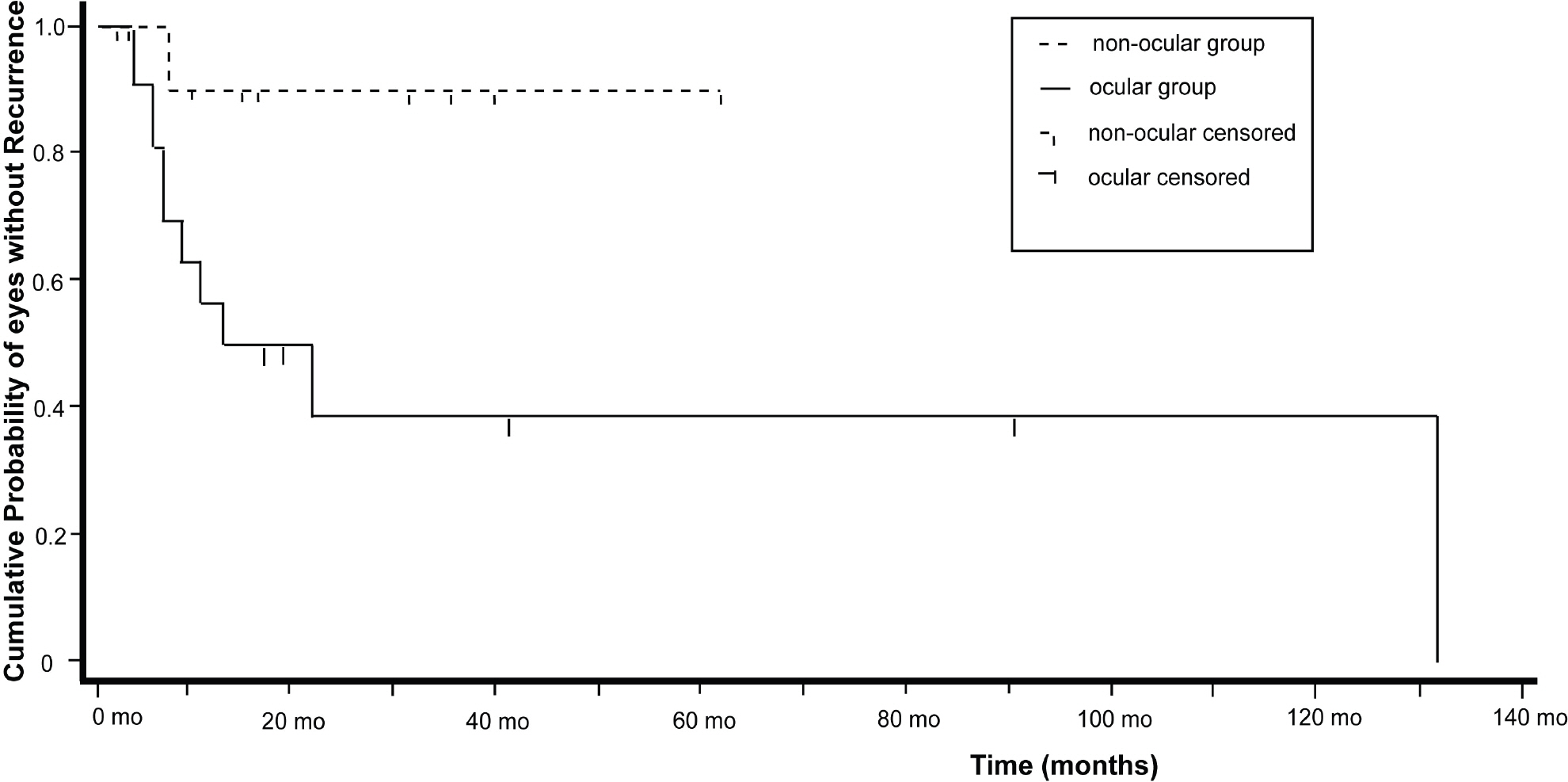
Of 440 patients with endogenous uveitis, 31 (7.1%) with sarcoidosis were included. The mean age at onset was 54.5 years. Sarcoidosis patients with uveitis tended to be older than those without uveitis (44.1 years). Uveitis was the primary manifestation of sarcoidosis in 16 of 31 patients (51.6%). Anterior uveitis was the most common in terms of the anatomic location of inflammation (54.8%), and posterior involvement (38.7%) was not rare. Systemic corticosteroid therapy was administered to 28 patients (90.3%). Five patients (16.1%) received corticosteroids combined with immunosuppressive agents.
CONCLUSIONS
Sarcoid uveitis is not a rare etiology of endogenous uveitis. Topical or systemic corticosteroids could control inflammation in most cases, but immunosuppressive agents are needed in a small percentage of patients. Steroids combined with immunosuppressive agents can prevent severe visual losses in such patients.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Statement on sarcoidosis Joint statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the Association of Sarcoidosis Granulomatous and other Disorders (WASOG) adopted by the ERS Executive Committee, February, 1999. Am J Respir Crit Care Med. 1999; 160:736–55.2. Costabel U. Sarcoidosis: clinical update. Eur Respir J. 2001; 32:56–68.3. Baumer I, Zissel G, Schlaak M, Muller-Quernheim J. Th1/Th2 cell distribution in pulmonary sarcoidosis. Am J Respir Cell Mol Biol. 1997; 16:171–7.
Article4. Song Z, Marzilli L, Greenlee BM. . Mycobacterial catalase-peroxidase is a tissue antigen and target of the adaptive immune response in systemic sarcoidosis. J Exp Med. 2005; 201:755–67.
Article5. Yasuhara T, Tada R, Nakano Y. . The presence of Propionibacterium spp. in the vitreous fluid of uveitis patients with sarcoidosis. Acta Ophthalmol Scand. 2005; 83:364–9.
Article6. Siltzbach LE, James DG, Neville E. . Course and prognosis of sarcoidosis around the world. Am J Med. 1974; 57:847–52.
Article7. James DG, Neville E, Langley DA. Ocular sarcoidosis. Trans Ophthalmol Soc U K. 1976; 96:133–9.
Article8. Jabs DA, Johns CJ. Ocular involvement in chronic sarcoidosis. Am J Ophthalmol. 1986; 102:297–301.
Article9. Bradley D, Baughman RP, Raymond L, Kaufman AH. Ocular manifestations of sarcoidosis. Semin Respir Crit Care Med. 2002; 23:543–8.
Article10. Chung YM, Lin YC, Liu YT. . Uveitis with Biopsy-proven sarcoidosis in Chinese-a study of 60 patients in a vveitis clinic over a period of 20 years. J Chin Med Assoc. 2007; 70:492–6.11. Wakabayashi T, Morimura Y, Miyamoto Y, Okada AA. Changing patterns of intraocular inflammatory disease in Japan. Ocul Immunol Inflamm. 2003; 11:277–86.
Article12. Rodriguez A, Calogne M, Pedroza-Seres M. . Referral patterns of uveitis in a tertiary eye care center. Arch Ophthalmol. 1996; 114:593–9.
Article13. Rothova A, Suttorp-van Schulten MS, Frits Treffers W, Kijlstra A. Causes and frequency of blindness in patients with intraocular inflammatory disease. Br J Ophthalmol. 1996; 80:332–6.
Article14. Cho NC, Ahn HS. A case of palpebral sarcoidosis associated with granulomatous uveitis. J Korean Ophthalmol Soc. 1990; 31:810–23.15. Lee TH, Kim YJ, Sin DH. Case report: Ocular sarcoidosis. J Korean Ophthalmol Soc. 1993; 34:687–91.16. Kim KS, Choi BC, Kim HJ. . A case of sarcoidosis associated with uveitis and vitreous hemorrhage. J Korean Ophthalmol Soc. 1988; 29:433–42.17. Sohn MS, Kim JD, Cha OJ. . A case of sarcoidosis associated with granulomatous uveitis. J Korean Ophthalmol Soc. 1967; 8:11–6.18. Lee DY, Kim DH, Yu SY, Gwag HU. A case of sarcoidosis misdiagnosed as tuberculosis in the early phase. J Korean Ophthalmol Soc. 2004; 45:438–43.19. Ko DA, Kim BJ. Sarcoidosis, presented as recurrent eyelid masses. J Korean Ophthalmol Soc. 2004; 45:1590–5.20. Standardization of Uveitis Nomenclature (SUN) Working Group Standardization of uveitis nomenclature for reporting clinical data: results of the first international workshop. Am J Ophthalmol. 2005; 140:509–16.21. BenEzra D, Forrester JV, Nussenblatt RB. . Uveitis Scoring System. Berlin: Springer-Verlag;1991. p. 1–13.
Article22. O’Connor GR. Ocular sarcoidosis. Trans New Orleans Acad Ophthalmol. 1983; 31:211–22.23. Margolis R, Lowder CY. Sarcoidosis. Curr Opin Ophthalmol. 2007; 18:470–5.
Article24. Goto H, Mochizuki M, Yamaki K. . Epidemiological survey of intraocular inflammation in Japan. Jpn J Ophthalmol. 2007; 51:41–4.
Article25. Diab S, Karnik A, Ouda B. . Sarcoidosis in Arabs: The clinical profile of 20 patients and a review of the literature. Sarcoidosis. 1991; 8:56–62.26. Hegab SM, Al-Mutawa SA, Sheriff SM. Ocular sarcoidosis in Kuwait with a review of literature. Int Ophthalmol. 1998; 21:255–60.27. Jones NP. Sarcoidosis and uveitis. Ophthalmol Clin North Am. 2002; 15:319–26.
Article28. Bonfioli AA, Orefice F. Sarcoidosis. Semin Ophthalmol. 2005; 20:177–82.
Article29. Baughman RP, Winget DB, Lower EE. Methotrexate is steroid sparing in acute sarcoidosis. Sarcoidosis. 2000; 17:60–6.30. White ES, Lynch JP. 3rd. Current and emerging strategies for the management of sarcoidosis. Expert Opin Pharmacother. 2007; 8:1293–311.
Article31. Kawaguchi T, Hanada A, Horie S. . Evaluation of characteristic ocular signs and systemic investigations in ocular sarcoidosis patients. Jpn J Ophthalmol. 2007; 51:121–6.
Article32. Power WJ, Neves RA, Rodriguez A. . The value of combined serum angiotensin-converting enzyme and gallium scan in diagnosing ocular sarcoidosis. Ophthalmology. 1995; 102:2007–11.
Article33. King TE. Overview of sarcoidosis. UpToDate Online 13.1. Available at: http://www.uptodate.com/.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Necrotizing Sarcoid Granulomatosis
- Sarcoid-Like Reaction after Complete Remission of Malignancy: CT and 18F-FDG PET/CT Features for the Differential Diagnosis from Lymph Node Metastasis
- Clineal Analysis of Peripheral Uveitis
- Clinical Features and Risk Factors for Uveitis in Patients with Ankylosing Spondylitis: A Survey-Based Study
- Clinical analysis of uveitis