J Korean Orthop Assoc.
2014 Jun;49(3):239-243.
Arthroscopic Treatment of Delayed Patella Infera
- Affiliations
-
- 1Department of Orthopedic Surgery, VHS Medical Center, Seoul, Korea. jaekorea@gmail.com
- 2Department of Orthopaedic Surgery, Konkuk University School of Medicine, Seoul, Korea.
Abstract
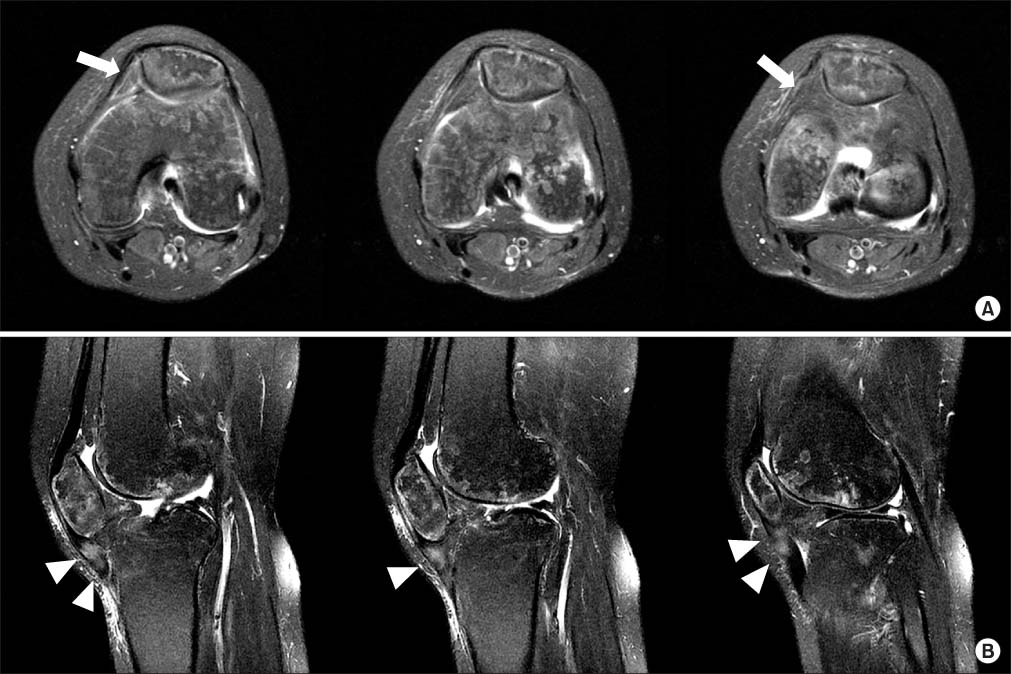
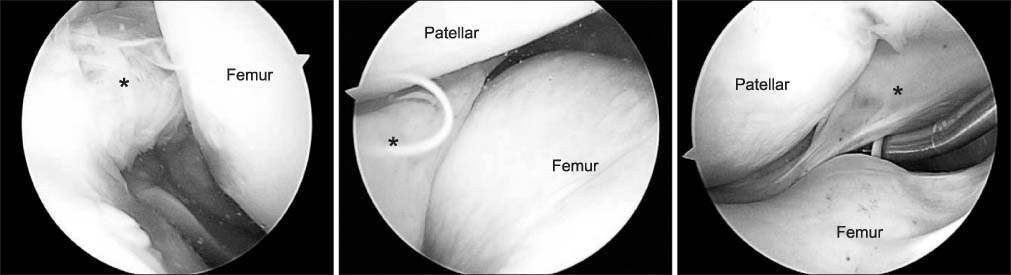
- Patella infera (baja) is a rare condition that can result from several etiologies including trauma around the knee. Risk factors include scar tissue formation in the retropatella fat pad, extensor mechanism dysfunction, immobilization in extension position of the knee joint, etc. Unawareness and delayed recognition are known to be associated with long-term disability. In this condition, arthroscopic treatment is generally recommended only for early cases. In this report, we present a case with reasonable outcome of delayed patella infera treated by arthroscopic treatment. Prudent arthroscopic debridement of the responsible scar tissue and accelerated rehabilitation therapy is necessary for achievement of a successful outcome.
MeSH Terms
Figure
Reference
-
1. Conner AN. The treatment of flexion contractures of the knee in poliomyelitis. J Bone Joint Surg Br. 1970; 52:138–144.
Article2. Mingo-Robinet J, Castañeda-Cabrero C, Alvarez V, León Alonso-Cortés JM, Monge-Casares E. Tourniquet-related iatrogenic femoral nerve palsy after knee surgery: case report and review of the literature. Case Rep Orthop. 2013; 2013:368290.
Article3. Mariani PP, Del Signore S, Perugia L. Early development of patella infera after knee fractures. Knee Surg Sports Traumatol Arthrosc. 1994; 2:166–169.
Article4. Hantes ME, Zachos VC, Bargiotas KA, Basdekis GK, Karantanas AH, Malizos KN. Patellar tendon length after anterior cruciate ligament reconstruction: a comparative magnetic resonance imaging study between patellar and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2007; 15:712–719.
Article5. Noyes FR, Wojtys EM, Marshall MT. The early diagnosis and treatment of developmental patella infera syndrome. Clin Orthop Relat Res. 1991; 265:241–252.
Article6. Okamoto R, Koshino T, Morii T. Shortening of patellar ligament and patella baja with improvement of quadriceps muscle strength after high tibial osteotomy. Bull Hosp Jt Dis. 1993; 53:21–24.7. Scuderi GR, Windsor RE, Insall JN. Observations on patellar height after proximal tibial osteotomy. J Bone Joint Surg Am. 1989; 71:245–248.
Article8. Paulos LE, Wnorowski DC, Greenwald AE. Infrapatellar contracture syndrome. Diagnosis, treatment, and long-term followup. Am J Sports Med. 1994; 22:440–449.9. Richmond JC, al Assal M. Arthroscopic management of arthrofibrosis of the knee, including infrapatellar contraction syndrome. Arthroscopy. 1991; 7:144–147.
Article10. Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990; 18:292–299.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Patella Infera in Residual Poliomyelitis
- A Clinical Study of Patella Alta and Infera
- Arthroscopic-Assisted Reduction and Internal Fixation of Patella Fractures
- Arthroscopic Reduction and Percutaneous Cannulated Screw Fixation for Longitudinal Fractures of Patella
- Osteomyelitis of the Patella in a Child: A Case Report