J Gastric Cancer.
2016 Jun;16(2):72-77. 10.5230/jgc.2016.16.2.72.
Should an Aberrant Left Hepatic Artery Arising from the Left Gastric Artery Be Preserved during Laparoscopic Gastrectomy for Early Gastric Cancer Treatment?
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. tssohn@skku.edu
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2328072
- DOI: http://doi.org/10.5230/jgc.2016.16.2.72
Abstract
- PURPOSE
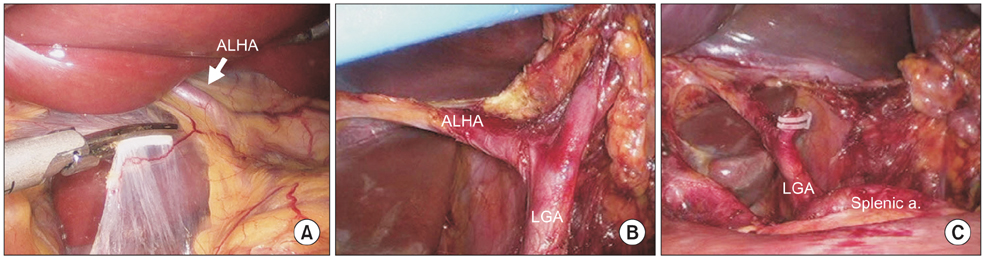
During laparoscopic gastrectomy, an aberrant left hepatic artery (ALHA) arising from the left gastric artery (LGA) is occasionally encountered. The aim of this study was to define when an ALHA should be preserved during laparoscopic gastrectomy.
MATERIALS AND METHODS
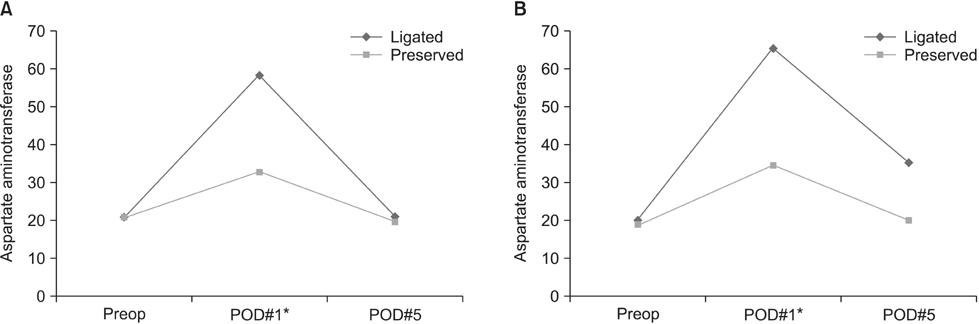
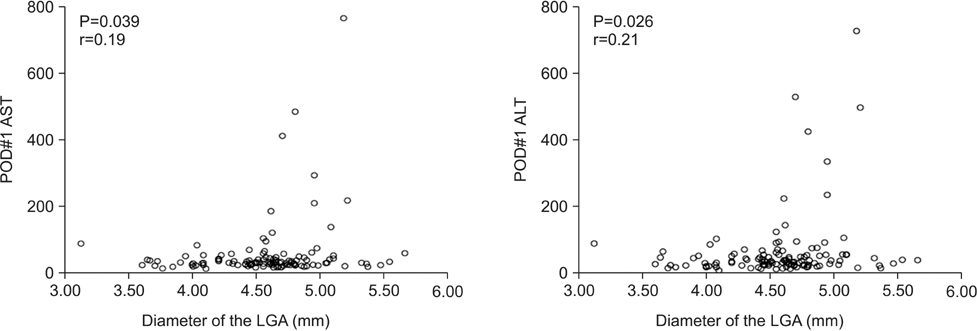
From August 2009 to December 2014, 1,340 patients with early gastric cancer underwent laparoscopic distal gastrectomy. One hundred fifty patients presented with an ALHA; of the ALHA was ligated in 116 patients and preserved in 34 patients. Patient characteristics, postoperative outcomes and perioperative liver function tests were reviewed retrospectively. Correlations between the diameter of the LGA measured on preoperative abdominal computed tomography and postoperative liver enzyme levels were analyzed.
RESULTS
Pearson's correlation analysis showed a positive correlation between the diameter of the LGA and serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels on postoperative day 1 in the ALHA-ligated group (P=0.039, P=0.026, respectively). Linear regression analysis estimated the diameter of the LGA to be 5.1 mm and 4.9 mm when AST and ALT levels were twice the normal limit on postoperative day 1.
CONCLUSIONS
We suggest preserving the ALHA arising from a large LGA, having diameter greater than 5 mm, during laparoscopic gastrectomy to prevent immediate postoperative hepatic dysfunction.
MeSH Terms
Figure
Reference
-
1. Michels NA. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg. 1966; 112:337–347.2. Hiatt JR, Gabbay J, Busuttil RW. Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg. 1994; 220:50–52.3. López-Andújar R, Moya A, Montalvá E, Berenguer M, De Juan M, San Juan F, et al. Lessons learned from anatomic variants of the hepatic artery in 1,081 transplanted livers. Liver Transpl. 2007; 13:1401–1404.4. Oki E, Sakaguchi Y, Hiroshige S, Kusumoto T, Kakeji Y, Maehara Y. Preservation of an aberrant hepatic artery arising from the left gastric artery during laparoscopic gastrectomy for gastric cancer. J Am Coll Surg. 2011; 212:e25–e27.5. Kim YW, Yoon HM, Eom BW, Park JY. History of minimally invasive surgery for gastric cancer in Korea. J Gastric Cancer. 2012; 12:13–17.6. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112.7. Shinohara T, Ohyama S, Muto T, Yanaga K, Yamaguchi T. The significance of the aberrant left hepatic artery arising from the left gastric artery at curative gastrectomy for gastric cancer. Eur J Surg Oncol. 2007; 33:967–971.8. Huang CM, Chen QY, Lin JX, Zheng CH, Li P, Xie JW, et al. Short-term clinical implications of the accessory left hepatic artery in patients undergoing radical gastrectomy for gastric cancer. PLoS One. 2013; 8:e64300.9. Lurie AS. The significance of the variant left accessory hepatic artery in surgery for proximal gastric cancer. Arch Surg. 1987; 122:725–728.10. Hemming AW, Finley RJ, Evans KG, Nelems B, Fradet G. Esophagogastrectomy and the variant left hepatic artery. Ann Thorac Surg. 1992; 54:166–168.11. Matsuki M, Kani H, Tatsugami F, Yoshikawa S, Narabayashi I, Lee SW, et al. Preoperative assessment of vascular anatomy around the stomach by 3D imaging using MDCT before laparoscopy-assisted gastrectomy. AJR Am J Roentgenol. 2004; 183:145–151.12. Lee SW, Shinohara H, Matsuki M, Okuda J, Nomura E, Mabuchi H, et al. Preoperative simulation of vascular anatomy by three-dimensional computed tomography imaging in laparoscopic gastric cancer surgery. J Am Coll Surg. 2003; 197:927–936.13. Yamashita K, Sakuramoto S, Mieno H, Shibata T, Nemoto M, Katada N, et al. Preoperative dual-phase 3D CT angiography assessment of the right hepatic artery before gastrectomy. Surg Today. 2014; 44:1912–1919.14. Koops A, Wojciechowski B, Broering DC, Adam G, Krupski-Berdien G. Anatomic variations of the hepatic arteries in 604 selective celiac and superior mesenteric angiographies. Surg Radiol Anat. 2004; 26:239–244.15. Miyaki T, Sakagami S, Ito H. Intrahepatic territory of the accessory hepatic artery in the human. Acta Anat (Basel). 1989; 136:34–37.16. Okano S, Sawai K, Taniguchi H, Takahashi T. Aberrant left hepatic artery arising from the left gastric artery and liver function after radical gastrectomy for gastric cancer. World J Surg. 1993; 17:70–73. discussion 74.17. Koehler RE, Korobkin M, Lewis F. Arteriographic demonstration of collateral arterial supply to the liver after hepatic artery ligation. Radiology. 1975; 117:49–54.18. Mays ET, Wheeler CS. Demonstration of collateral arterial flow after interruption of hepatic arteries in man. N Engl J Med. 1974; 290:993–996.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Common Hepatic Artery Originating from Left Gastric Artery: A Rare Variant Encountered in Gastric Cancer Surgery
- Implication of the Accessory Left Hepatic Artery in Curative Surgery for Gastric Cancer
- Analysis of branching patterns of middle hepatic artery using A-P and oblique view hepatic angiography
- Normal Variation of Hepatic Artery
- Setting the Stomach Transection Line Based on Anatomical Landmarks in Laparoscopic Distal Gastrectomy