J Menopausal Med.
2014 Apr;20(1):1-6.
Postmenopausal Hypertension and Sodium Sensitivity
- Affiliations
-
- 1Department of Urology, Soonchunhyang University, College of Medicine, Bucheon, Korea.
- 2Department of Obstetrics and Gynecology, Soonchunhyang University, College of Medicine, Bucheon, Korea.
- 3Department of Nephrology, Yale University, School of Medicine, New Haven, USA.
- 4Department of Cellular and Molecular Physiology, Yale University, School of Medicine, New Haven, USA. tong.wang@yale.edu
Abstract
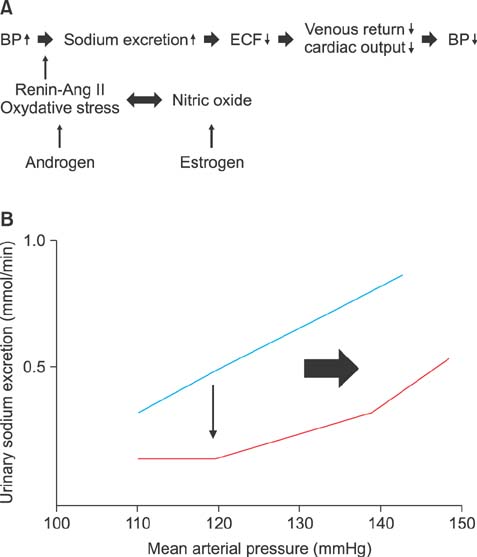
- It has been well established that women generally have lower incidence rates of hypertension than men at similar ages and these differences may vary with age. It also has been observed in many studies that after menopause, blood pressure (BP) increases in women to levels even higher than in men. The lack of estrogens may not be suggested as the only component involved in the development of postmenopausal hypertension. Thus, in this mini-review, the possible mechanisms by which sex hormones may influence the BP are discussed. This review also examines the renal regulatory mechanisms for gender differences in BP and explores the effects of salt intake on BP (salt-sensitivity) in pre and post-menopausal women. Estrogen has been shown to stimulate nitric oxide (NO) production, thus female sex hormones have a beneficial effect on BP control. Evidences that angiotensin type 2 receptor (AT2R) is up-regulated by estrogen support the favorable effects on BPs in women than men. The kidney plays an integral role in the regulation of arterial pressure through the mechanism of pressure-natriuresis, which has been shown to be modulated by the RAS. The prevalence of salt-sensitivity increases with age and low-salt diets has shown to help reduce systolic BP (SBP) and diastolic BP. While oral hormone replacement therapy has yielded only a neutral or minimal effect on the elevation of SBP, both the transdermal route replacement and a novel progestin with anti-aldosterone activity (drospirenone) has also shown to reduce SBP.
MeSH Terms
-
Arterial Pressure
Blood Pressure
Diet, Sodium-Restricted
Estrogens
Female
Gonadal Steroid Hormones
Hormone Replacement Therapy
Humans
Hypertension*
Incidence
Kidney
Male
Menopause
Nitric Oxide
Postmenopause
Prevalence
Receptor, Angiotensin, Type 2
Sodium*
Estrogens
Gonadal Steroid Hormones
Nitric Oxide
Receptor, Angiotensin, Type 2
Sodium
Figure
Reference
-
1. Kim JA, Kim SM, Choi YS, Yoon D, Lee JS, Park HS, et al. The prevalence and risk factors associated with isolated untreated systolic hypertension in Korea: the Korean National Health and Nutrition Survey 2001. J Hum Hypertens. 2007; 21:107–113.2. Reckelhoff JF. Gender differences in the regulation of blood pressure. Hypertension. 2001; 37:1199–1208.3. Hernandez Schulman I, Raij L. Salt sensitivity and hypertension after menopause: role of nitric oxide and angiotensin II. Am J Nephrol. 2006; 26:170–180.4. Romero JC, Reckelhoff JF. State-of-the-Art lecture. Role of angiotensin and oxidative stress in essential hypertension. Hypertension. 1999; 34:943–949.5. Mikkola T, Viinikka L, Ylikorkala O. Estrogen and postmenopausal estrogen/progestin therapy: effect on endothelium-dependent prostacyclin, nitric oxide and endothelin-1 production. Eur J Obstet Gynecol Reprod Biol. 1998; 79:75–82.6. Wambach G, Higgins JR. Antimineralocorticoid action of progesterone in the rat: correlation of the effect on electrolyte excretion and interaction with renal mineralocorticoid receptors. Endocrinology. 1978; 102:1686–1693.7. Hall JE, Brands MW, Henegar JR. Angiotensin II and long-term arterial pressure regulation: the overriding dominance of the kidney. J Am Soc Nephrol. 1999; 10:Suppl 12. S258–S265.8. Li XC, Hopfer U, Zhuo JL. AT1 receptor-mediated uptake of angiotensin II and NHE-3 expression in proximal tubule cells through a microtubule-dependent endocytic pathway. Am J Physiol Renal Physiol. 2009; 297:F1342–F1352.9. Ellison DH. Through a glass darkly: salt transport by the distal tubule. Kidney Int. 2011; 79:5–8.10. Guyton AC, Coleman TG, Cowley AV Jr, Scheel KW, Manning RD Jr, Norman RA Jr. Arterial pressure regulation. Overriding dominance of the kidneys in longterm regulation and in hypertension. Am J Med. 1972; 52:584–594.11. Reckelhoff JF, Zhang H, Granger JP. Testosterone exacerbates hypertension and reduces pressure-natriuresis in male spontaneously hypertensive rats. Hypertension. 1998; 31:435–439.12. McGuire BB, Watson RW, Pérez-Barriocanal F, Fitzpatrick JM, Docherty NG. Gender differences in the renin-angiotensin and nitric oxide systems: relevance in the normal and diseased kidney. Kidney Blood Press Res. 2007; 30:67–80.13. James GD, Sealey JE, Müller F, Alderman M, Madhavan S, Laragh JH. Renin relationship to sex, race and age in a normotensive population. J Hypertens Suppl. 1986; 4:S387–S389.14. Danser AH, Derkx FH, Schalekamp MA, Hense HW, Riegger GA, Schunkert H. Determinants of interindividual variation of renin and prorenin concentrations: evidence for a sexual dimorphism of (pro)renin levels in humans. J Hypertens. 1998; 16:853–862.15. Reckelhoff JF, Zhang H, Srivastava K. Gender differences in development of hypertension in spontaneously hypertensive rats: role of the renin-angiotensin system. Hypertension. 2000; 35:480–483.16. Rabi DM, Khan N, Vallee M, Hladunewich MA, Tobe SW, Pilote L. Reporting on sex-based analysis in clinical trials of angiotensin-converting enzyme inhibitor and angiotensin receptor blocker efficacy. Can J Cardiol. 2008; 24:491–496.17. Du Z, Wan L, Yan Q, Weinbaum S, Weinstein AM, Wang T. Regulation of glomerulotubular balance: II: impact of angiotensin II on flow-dependent transport. Am J Physiol Renal Physiol. 2012; 303:F1507–F1516.18. Zhuo JL, Li XC. New insights and perspectives on intrarenal renin-angiotensin system: focus on intracrine/intracellular angiotensin II. Peptides. 2011; 32:1551–1565.19. Sampson AK, Moritz KM, Jones ES, Flower RL, Widdop RE, Denton KM. Enhanced angiotensin II type 2 receptor mechanisms mediate decreases in arterial pressure attributable to chronic low-dose angiotensin II in female rats. Hypertension. 2008; 52:666–671.20. Hilliard LM, Nematbakhsh M, Kett MM, Teichman E, Sampson AK, Widdop RE, et al. Gender differences in pressure-natriuresis and renal autoregulation: role of the Angiotensin type 2 receptor. Hypertension. 2011; 57:275–282.21. Forte P, Kneale BJ, Milne E, Chowienczyk PJ, Johnston A, Benjamin N, et al. Evidence for a difference in nitric oxide biosynthesis between healthy women and men. Hypertension. 1998; 32:730–734.22. Hemmelgarn BR, Zhang J, Manns BJ, Tonelli M, Larsen E, Ghali WA, et al. Progression of kidney dysfunction in the community-dwelling elderly. Kidney Int. 2006; 69:2155–2161.23. Tharaux PL, Chatziantoniou C, Casellas D, Fouassier L, Ardaillou R, Dussaule JC. Vascular endothelin-1 gene expression and synthesis and effect on renal type I collagen synthesis and nephroangiosclerosis during nitric oxide synthase inhibition in rats. Circulation. 1999; 99:2185–2191.24. Tostes RC, Fortes ZB, Callera GE, Montezano AC, Touyz RM, Webb RC, et al. Endothelin, sex and hypertension. Clin Sci (Lond). 2008; 114:85–97.25. Yanagisawa M, Kurihara H, Kimura S, Tomobe Y, Kobayashi M, Mitsui Y, et al. A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature. 1988; 332:411–415.26. Polderman KH, Stehouwer CD, van Kamp GJ, Dekker GA, Verheugt FW, Gooren LJ. Influence of sex hormones on plasma endothelin levels. Ann Intern Med. 1993; 118:429–432.27. Rabelink TJ, Kaasjager KA, Boer P, Stroes EG, Braam B, Koomans HA. Effects of endothelin-1 on renal function in humans: implications for physiology and pathophysiology. Kidney Int. 1994; 46:376–381.28. Seo B, Oemar BS, Siebenmann R, von Segesser L, Luscher TF. Both ETA and ETB receptors mediate contraction to endothelin-1 in human blood vessels. Circulation. 1994; 89:1203–1208.29. Kittikulsuth W, Sullivan JC, Pollock DM. ET-1 actions in the kidney: evidence for sex differences. Br J Pharmacol. 2013; 168:318–326.30. Pollock JS, Pollock DM. Endothelin and NOS1/nitric oxide signaling and regulation of sodium homeostasis. Curr Opin Nephrol Hypertens. 2008; 17:70–75.31. Pechère-Bertschi A, Burnier M. Female sex hormones, salt, and blood pressure regulation. Am J Hypertens. 2004; 17:994–1001.32. Weinberger MH, Miller JZ, Luft FC, Grim CE, Fineberg NS. Definitions and characteristics of sodium sensitivity and blood pressure resistance. Hypertension. 1986; 8:II127–II134.33. Kawasaki T, Delea CS, Bartter FC, Smith H. The effect of high-sodium and low-sodium intakes on blood pressure and other related variables in human subjects with idiopathic hypertension. Am J Med. 1978; 64:193–198.34. Weinberger MH. Pathogenesis of salt sensitivity of blood pressure. Curr Hypertens Rep. 2006; 8:166–170.35. Pechère-Bertschi A, Maillard M, Stalder H, Brunner HR, Burnier M. Blood pressure and renal haemodynamic response to salt during the normal menstrual cycle. Clin Sci (Lond). 2000; 98:697–702.36. Tominaga T, Suzuki H, Ogata Y, Matsukawa S, Saruta T. The role of sex hormones and sodium intake in postmenopausal hypertension. J Hum Hypertens. 1991; 5:495–500.37. Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013; 346:f1326.38. Weinberger MH. Salt sensitivity: does it play an important role in the pathogenesis and treatment of hypertension? Curr Opin Nephrol Hypertens. 1996; 5:205–208.39. Preston RA. Comparative effects of conventional vs. novel hormone replacement therapy on blood pressure in postmenopausal women. Climacteric. 2009; 12:Suppl 1. 66–70.40. Wassertheil-Smoller S, Hendrix SL, Limacher M, Heiss G, Kooperberg C, Baird A, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women's Health Initiative: a randomized trial. JAMA. 2003; 289:2673–2684.41. Akkad AA, Halligan AW, Abrams K, al-Azzawi F. Differing responses in blood pressure over 24 hours in normotensive women receiving oral or transdermal estrogen replacement therapy. Obstet Gynecol. 1997; 89:97–103.42. White WB, Hanes V, Chauhan V, Pitt B. Effects of a new hormone therapy, drospirenone and 17-beta-estradiol, in postmenopausal women with hypertension. Hypertension. 2006; 48:246–253.