J Korean Surg Soc.
2012 May;82(5):306-311.
Risk factors for delayed recanalization of calf vein thrombosis
- Affiliations
-
- 1Division of Vascular Surgery, Department of Surgery, Cardiac and Vascular Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ywkim@skku.edu
- 2Department of Surgery, Seoul Medical Center, Seoul, Korea.
- 3Division of Cardiology, Department of Medicine, Cardiac and Vascular Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
Abstract
- PURPOSE
To determine the risk factors of delayed recanalization of isolated calf vein thrombosis (CVT).
METHODS
One hundred fifty limbs of 110 patients with CVT between September 2007 and April 2010 were enrolled. We used ultrasonography for the diagnosis and follow-up examinations of CVT. We calculated recanalization rates at 1 and 3 months after initial diagnosis and analyzed the risk factors associated with delayed recanalization of CVT.
RESULTS
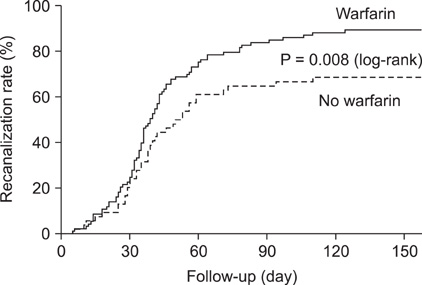
CVTs were located in the muscular calf vein in 110 (73.3%), in the deep calf vein in 18 (12%), and in both in 22 cases (14.7%). Among all CVTs, 94 limbs (63%) were symptomatic. Major risk factors for CVT were orthopedic surgery (87.3%), malignancy (21.3%), and immobilization (15.3%). Sixty-seven patients (60.9%) were treated with oral anticoagulation therapy, while 43 patients by low molecular weight heparin (n = 19) or by conservative methods including elastic compression stockings and ambulation (n = 21). The cumulative recanalization rate at 1 and 3 months was 23% and 82% and it was significantly higher in patients who underwent oral anticoagulation therapy compared with patients without oral anticoagulation therapy (84% vs. 65%, P = 0.008 by log-rank test). Malignancy (odds ratio [OR], 2.789; P = 0.043) and immobilization (OR, 4.191; P = 0.029) were independent risk factors for delayed recanalization of CVT and oral anticoagulation (OR, 0.300; P = 0.020) was an independent factor in promoting recanalization in multivariate analysis.
CONCLUSION
For patients with isolated CVT, no oral anticoagulation resulted in higher rates of delayed recanalization compared to oral anticoagulation treatment. Immobilization and having malignancy were independent risk factors for delayed recanalization.
Keyword
MeSH Terms
Figure
Reference
-
1. Labropoulos N, Webb KM, Kang SS, Mansour MA, Filliung DR, Size GP, et al. Patterns and distribution of isolated calf deep vein thrombosis. J Vasc Surg. 1999. 30:787–791.2. Simons GR, Skibo LK, Polak JF, Creager MA, Klapec-Fay JM, Goldhaber SZ. Utility of leg ultrasonography in suspected symptomatic isolated calf deep venous thrombosis. Am J Med. 1995. 99:43–47.3. Gottlieb RH, Widjaja J. Clinical outcomes of untreated symptomatic patients with negative findings on sonography of the thigh for deep vein thrombosis: our experience and a review of the literature. AJR Am J Roentgenol. 1999. 172:1601–1604.4. Gottlieb RH, Widjaja J, Tian L, Rubens DJ, Voci SL. Calf sonography for detecting deep venous thrombosis in symptomatic patients: experience and review of the literature. J Clin Ultrasound. 1999. 27:415–420.5. Oishi CS, Grady-Benson JC, Otis SM, Colwell CW Jr, Walker RH. The clinical course of distal deep venous thrombosis after total hip and total knee arthroplasty, as determined with duplex ultrasonography. J Bone Joint Surg Am. 1994. 76:1658–1663.6. Reis SE, Polak JF, Hirsch DR, Cohn LH, Creager MA, Donovan BC, et al. Frequency of deep venous thrombosis in asymptomatic patients with coronary artery bypass grafts. Am Heart J. 1991. 122:478–482.7. Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ, et al. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008. 133:6 Suppl. 454S–545S.8. Nordstrom M, Lindblad B, Bergqvist D, Kjellstrom T. A prospective study of the incidence of deep-vein thrombosis within a defined urban population. J Intern Med. 1992. 232:155–160.9. White RH. The epidemiology of venous thromboembolism. Circulation. 2003. 107:23 Suppl 1. I4–I8.10. Lohr JM, Kerr TM, Lutter KS, Cranley RD, Spirtoff K, Cranley JJ. Lower extremity calf thrombosis: to treat or not to treat? J Vasc Surg. 1991. 14:618–623.11. Righini M, Paris S, Le Gal G, Laroche JP, Perrier A, Bounameaux H. Clinical relevance of distal deep vein thrombosis. Review of literature data. Thromb Haemost. 2006. 95:56–64.12. Schwarz T, Schmidt B, Beyer J, Schellong SM. Therapy of isolated calf muscle vein thrombosis with low-molecular-weight heparin. Blood Coagul Fibrinolysis. 2001. 12:597–599.13. Macdonald PS, Kahn SR, Miller N, Obrand D. Short-term natural history of isolated gastrocnemius and soleal vein thrombosis. J Vasc Surg. 2003. 37:523–527.14. Gillet JL, Perrin MR, Allaert FA. Short-term and mid-term outcome of isolated symptomatic muscular calf vein thrombosis. J Vasc Surg. 2007. 46:513–519.15. Giannoukas AD, Labropoulos N, Burke P, Katsamouris A, Nicolaides AN. Calf deep venous thrombosis: a review of the literature. Eur J Vasc Endovasc Surg. 1995. 10:398–404.16. Lohr JM, Fellner AN. Isolated calf vein thrombosis should be treated with anticoagulation. Dis Mon. 2010. 56:590–600.17. Meissner MH, Caps MT, Bergelin RO, Manzo RA, Strandness DE Jr. Propagation, rethrombosis and new thrombus formation after acute deep venous thrombosis. J Vasc Surg. 1995. 22:558–567.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictor of Recanalization in Lower Extremity Deep Vein Thrombosis
- The Incidence of Deep Vein Thrombosis in the Lower Extremity
- Deep Vein Thrombosis after Total Hip Replacement: Incidence and correlation between DVT and its risk factors
- Deep Vein Thrombosis after Total Knee Replacement: Incidence and correlation with clinical risk factors
- Aspiration Thrombectomy Using a Guiding Catheter in Acute Lower Extremity Deep Vein Thrombosis: Usefulness of the Calf-Squeeze Technique