J Korean Soc Radiol.
2011 Mar;64(3):231-238. 10.3348/jksr.2011.64.3.231.
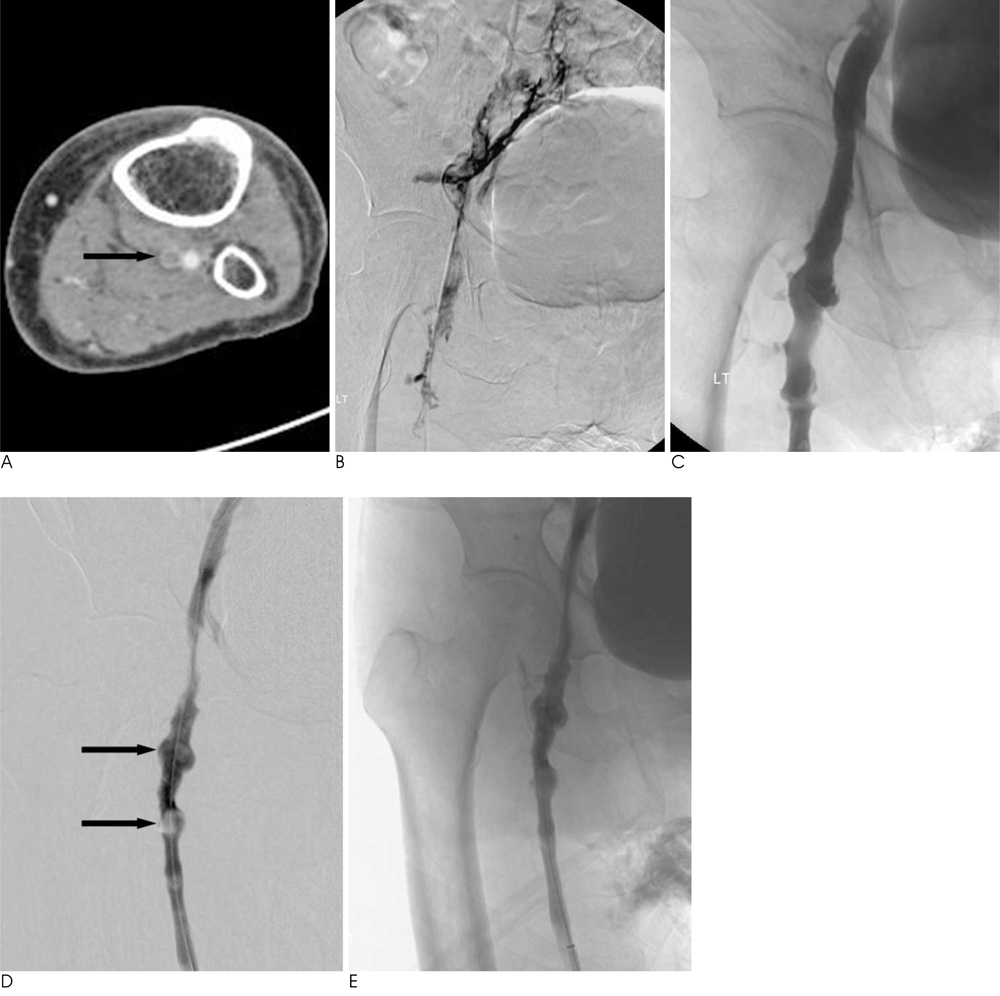
Aspiration Thrombectomy Using a Guiding Catheter in Acute Lower Extremity Deep Vein Thrombosis: Usefulness of the Calf-Squeeze Technique
- Affiliations
-
- 1Department of Radiology, Chonbuk National University Medical School, Chonbuk 561-712, Korea. kwak8140@jbnu.ac.kr
- 2Department of Surgery, Chonbuk National University Medical School, Chonbuk 561-712, Korea.
- KMID: 2097943
- DOI: http://doi.org/10.3348/jksr.2011.64.3.231
Abstract
- PURPOSE
The effectiveness of the calf-squeeze technique during aspiration thrombectomy using guiding catheter in the treatment of an acute lower extremity deep vein thrombosis (DVT) was evaluated by the use of imaging and the clinical follow-up of patients.
MATERIALS AND METHODS
A prospective analysis of ten patients (seven women, three men; median age, 56.9 years) with common iliac vein (CIV) obstruction and ipsilateral DVT was performed for this study. All patients presented with leg edema or pain and were treated with catheter-directed thrombolysis via an ipsilateral popliteal vein approach after insertion of a temporary inferior vena cava (IVC) filter. Subsequently, the patients were treated with by aspiration thrombectomy using a guiding catheter to remove the residual thrombus. The calf-squeeze technique during aspiration thrombectomy can be used to induce the proximal migration of thrombi in the popliteal, tibial, and muscular veins were used to increase venous flow.
RESULTS
The calf-squeeze technique was employed at mean of 1.3 times (range, 1-3 times). All patients showed proximal migration of a popliteal and muscular vein thrombus during the execution of the calf-squeeze technique. Successful recanalization was achieved in all patients (100%) without any complications. On duplex ultrasonography, which was performed immediately after the aspiration thrombectomy, four patients had a residual thrombus in the soleal muscular veins. However, none of the patients had a thrombus in the popliteal and tibial veins; and, during follow-up, no DVT recurred in any patient.
CONCLUSION
The use of the calf-squeeze technique during aspiration thrombectomy after catheter-directed thrombolysis can induce the proximal migration of thrombi in the popliotibial and muscular veins and is an effective method that can remove a thrombus in calf veins.
MeSH Terms
Figure
Reference
-
1. Markel A, Manzo RA, Bergelin RO, Strandness DE Jr. Valvular reflux after deep vein thrombosis: incidence and time of occurrence. J Vasc Surg. 1992; 15:377–382.2. Akesson H, Brudin L, Dahlstom JA, Eklof B, Ohlin P, Plate G. Venous function assessed during a 5 year period after acute ilio-femoral venous thrombosis treated with anticoagulation. Eur J Vasc Surg. 1990; 4:43–48.3. Comerota AJ, Aldridge SC, Cohen G, Ball DS, Pliskin M, White JV. A strategy of aggressive regional therapy for acute iliofemoral venous thrombosis with contemporary venous thrombectomy or catheter-directed thrombolysis. J Vasc Surg. 1994; 20:244–254.4. Semba CP, Dake MD. Iliofemoral deep venous thrombosis: aggressive therapy with catheter-directed thrombolysis. Radiology. 1994; 191:487–494.5. O'Sullivan GJ, Semba CP, Bittner CA, Kee ST, Razavi MK, Sze DY, et al. Endovascular management of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol. 2000; 11:823–836.6. Kwak HS, Han YM, Lee YS, Jin GY, Chung GH. Stents in common iliac vein obstruction with acute ipsilateral deep venous thrombosis: early and late results. J Vasc Interv Radiol. 2005; 16:815–822.7. Patel NH, Stookey KR, Ketcham DB, Cragg AH. Endovascular management of acute extensive iliofemoral deep venous thrombosis caused by May-Thurner syndrome. J Vasc Interv Radiol. 2000; 11:1297–1302.8. Vedantham S, Vesely TM, Sicard GA, Brown D, Rubin B, Sanchez LA, et al. Pharmacomechanical thrombolysis and early stent placement for iliofemoral deep vein thrombosis. J Vasc Interv Radiol. 2004; 15:565–574.9. Kim HS, Patra A, Paxton BE, Khan J, Streiff M. Adjunctive percutaneous mechanical thrombectomy for lower-extremity deep vein thrombosis: clinical and economic outcomes. J Vasc Interv Radiol. 2006; 17:1099–1104.10. Kasirajan K, Gray B, Ouriel K. Percutaneous angioJet thrombectomy in the management of extensive deep venous thrombosis. J Vasc Interv Radiol. 2001; 12:179–185.11. Vedantham S, Vesely TM, Parti N, Darcy M, Hovseian DM, Picus D. Lower extremity venous thrombolysis with adjunctive mechanical thrombectomy. J Vasc Interv Radiol. 2002; 13:1001–1008.12. Jaffe JW, Newcomb JA, York T, Matulewicz TJ. Venous valvular assessment after retrograde catheterization. J Vasc Interv Radiol. 1996; 7:595–597.13. Armon MP, Whitaker SC, Tennant WG. Catheter-directed thrombolysis of iliofemoral deep vein thrombosis. A new approach via the posterior tibial vein. Eur J Vasc Endovasc Surg. 1997; 13:413–416.14. Enden T, Sandvik L, Klow N, Hafsahl G, Holme PA, Holmen LO, et al. Catheter-directed venous thrombolysis in acute iliofemoral vein thrombosis-the CaVenT study: rationale and design of a multicenter, randomized, controlled, clinical trial. Am Heart J. 2007; 154:808–814.15. Lin PH, Zhou W, Dardik A, Mussa F, Kougias P, Hedayati N, et al. Catheter-direct thrombolysis versus pharmacomechanical thrombectomy for treatment of symptomatic lower extremity deep venous thrombosis. Am J Surg. 2006; 19:782–788.16. O'Sullivan GJ, Lohan DG, Gough N, Cronin CG, Kee ST. Pharmacomechanical thrombectomy of acute deep vein thrombosis with the Trellis-8 isolated thrombolysis catheter. J Vasc Interv Radiol. 2007; 18:715–724.17. Kölbel T, Lindh M, Holst J, Uher P, Eriksson KF, Sonesson B, et al. Extensive acute deep vein thrombosis of the iliocaval segment: midterm results of thrombolysis and stent placement. J Vasc Interv Radiol. 2007; 18:243–250.18. Elsharawy M, Elzayat E. Early results of thrombolysis vs anticoagulation in iliofemoral venous thrombosis. A randomised clinical trial. Eur J Vasc Endovasc Surg. 2002; 24:209–214.19. Watson LI, Armon MP. Thrombolysis for acute deep vein thrombosis. Cochrane Library. 2005; 1:1–66.20. Wells PS, Forster AJ. Thrombolysis in deep vein thrombosis: is there still an indication? Thromb Haemost. 2001; 86:499–508.21. Mewissen MW, Seabrook GR, Meissner MH, Cynamn J, Labroonlos N, Haughton SH, et al. Catheter-directed thrombolysis for lower extremity deep venous thrombosis: report of a national multicenter registry. Radiology. 1999; 211:39–49.22. McLennan G, Trerotola SO, Davidson E, Rhodes CA, Lazzaro C, Dreesen J, et al. The effects of a mechanical thrombolytic device on normal canine vein valves. J Vasc Interv Radiol. 2001; 12:89–94.23. Roy S, Laerum F. Transcatheter aspiration: the key to successful percutaneous treatment of deep venous thrombosis? Acad Radiol. 1999; 6:730–735.24. Sharafuddin MJ, Gu X, Han YM, Urness M, Gunther R, Amplatz K. Injury potential to venous valves from the Amplatz thrombectomy device. J Vasc Interv Radiol. 1999; 10:64–69.25. Polak JF. Peripheral vascular sonography: a practical guide. 2nd ed. Philadelphia: Lippincott Williams and Wilkins;2004. p. 168–220.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Incidence of Deep Vein Thrombosis in the Lower Extremity
- Catheter-Directed Thrombolysis with Conventional Aspiration Thrombectomy for Lower Extremity Deep Vein Thrombosis
- Surgical Technique for the Removal of Deep Vein Thrombi of the Lower Extremities
- Upper Extremity Deep Vein Thrombosis after Clavicle Fracture and Immobilization
- Clinical Experiences of Venous Stent for Deep Vein Thrombosis in the Lower Extremity