J Korean Soc Spine Surg.
2004 Dec;11(4):261-270.
Comparison of Smith-Petersen Osteotomy versus Pedicle Subtraction Osteotomy for the Correction of Fixed Sagittal Imbalance
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Inha University, Incheon, Korea. SRP@inha.com
- 2Washington University in St. Louis, Department of Orthopedic Surgery, USA.
Abstract
- STUDY DESIGN: A retrospective study.
OBJECTIVES
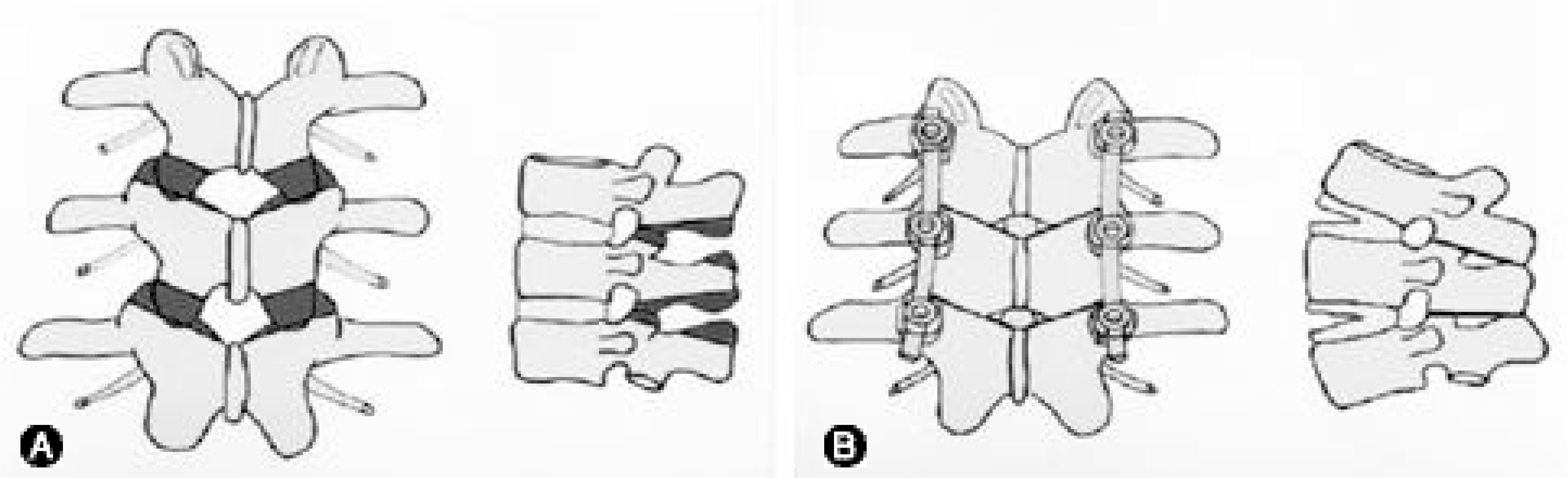
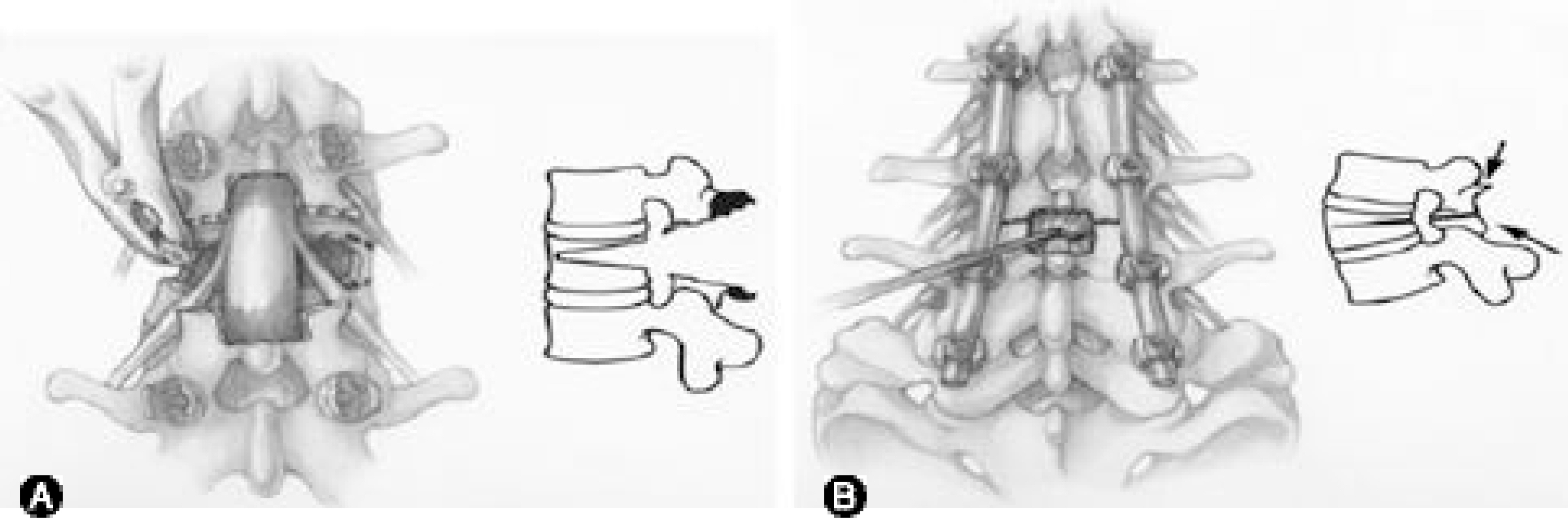
The purpose of this study was to compare the results between Smith-Petersen and pedicle subtraction osteotomies for fixed sagittal imbalance, and to determine the specific indications for each. LITERATURE REVIEW SUMMARY: Smith-Petersen (SPO) and pedicle subtraction osteotomies (PSO) are the techniques most commonly used to correct fixed sagittal imbalance of the spine, but there are no reports regarding the superiority of either technique. A Smith-Petersen osteotomy is an anterior opening wedge osteotomy, which hinges on the posterior edge of the intervertebral disc, while a pedicle subtraction osteotomy is a posterior closing wedge osteotomy, without distracting the anterior column, with the hinge on the anterior aspect of the vertebral body.
MATERIALS AND METHODS
Thirty patients (mean age 40.1 years, range 20 ~64 years), who underwent a SPO, were compared with forty-one patients (mean age 54.5 years, range 21 ~73 years) who underwent a PSO. The SPO was carried out in more than three segments (3 SPOs) in fourteen of the SPO group. The average follow-up periods were 4.6 years, ranging from 2 to 11.5 years, and 3.8 years, ranging from 2 to 7.1 years, for the SPO and PSO groups, respectively. Patients were evaluated by standing radiographs, chart review and outcome questionnaires.
RESULTS
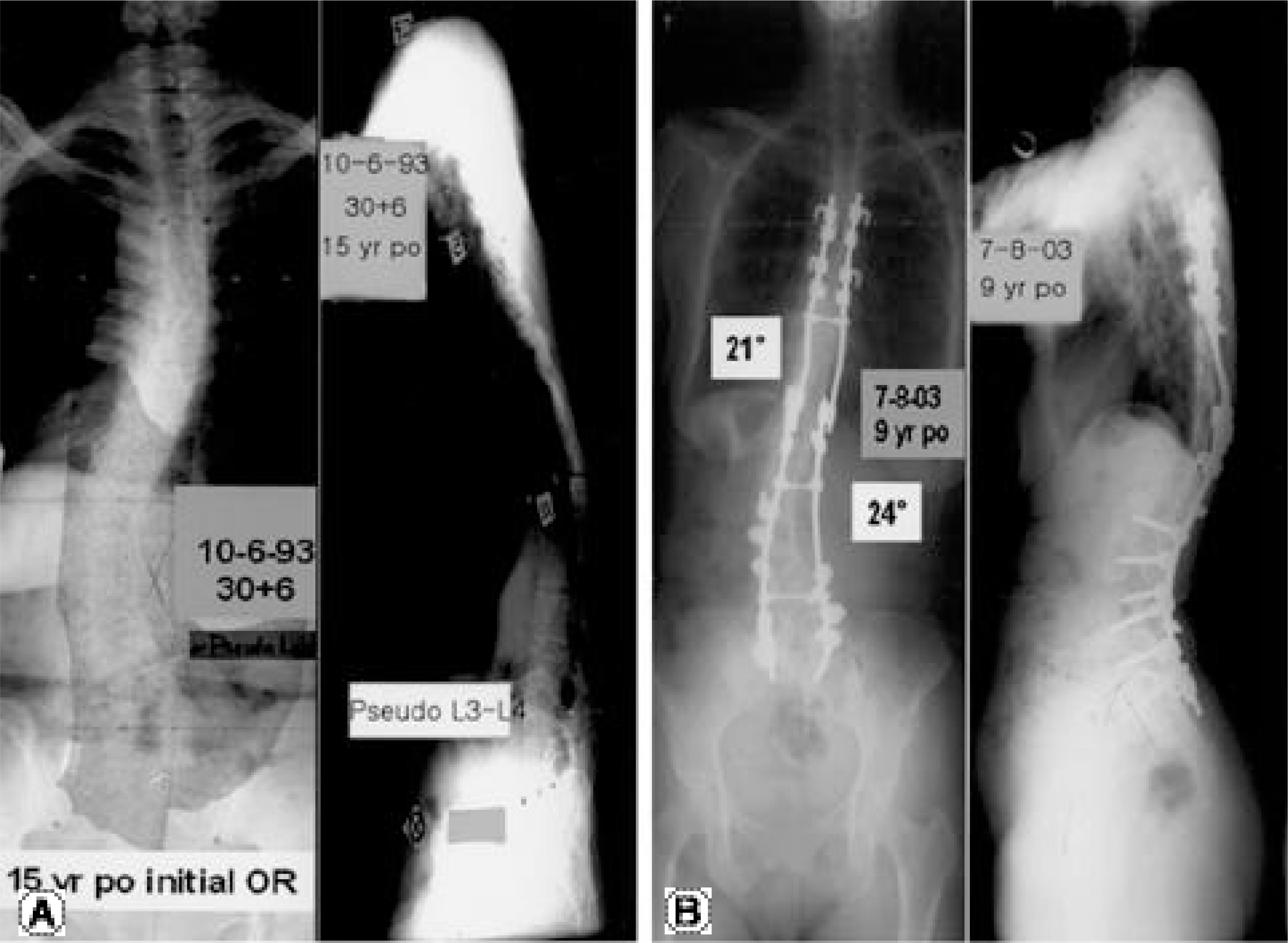
The mean correction of the kyphotic angle at the osteotomy sites for the SPOs was 10.7 per segment, and for those with 3 SPOs and the PSO group the average total corrections were 33.0+/-9.2 and 31.7+/-9.0, respectively. However, the improvement in sagittal balance was less statistically significantly with 3 SPOs (5.5+/-4.5 cm) than with a PSO (11.2+/-7.2 cm; p<0.01). Comparing 3 SPOs to one PSO, the SPO group decompensated the patients more substantially to the concavity (p<0.02). The mean estimated blood loss (adding up all anterior and posterior surgeries) for the procedures were 1398+/-738 (1392+/-664 mL in the 3 SPO group), and 2617+/-1645 mL in the SPO and PSO groups, respectively (p<0.001; p<0.01). The total operative times for the SPO versus the PSO groups were similar, with no statistical difference. There were substantial complications in both groups, with 13 in the 30 SPO and 30 in the 41 PSO patients. In the SPO group, 1 patient had a non-union at an osteotomy site; in the PSO group, 2 patients had a non-union at an osteotomy site. The mean Oswestry score improved from 42.3+/-14.2 to 21.3+/-14.8 postoperatively at the last visit for the SPO group and, it improved from 47.9+/-15.8 preoperatively to 29.7+/-18.3 at the last visit in PSO group (p=0.35).
CONCLUSIONS
When comparing 3 Smith-Petersen osteotomies to one pedicle subtraction osteotomy, the corrections of kyphosis were almost identical, but the improvement in the C7 plumb was significantly better in the PSO group. There was a significantly greater likelihood of decompensating the patient to the concavity with the 3 SPOs than with a single PSO (p<0.02). The total operative time for the SPO versus the PSO groups showed no statistical difference. However, the blood loss was substantially greater in the PSO group (p<0.001).
MeSH Terms
Figure
Reference
-
1). Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. J Bone Joint Surg. 1945; 27-A:1–11.
Article2). LaChapelle EH. Osteotomy of the lumbar spine for correction of kyphosis in a case of ankylosing spondylarthri -tis. J Bone Joint Surg. 1946; 28-A:851–858.3). Hehne HJ, Zielke K, Bohm H. Polysegmental lumbar osteotomies and transpedicled fixation for correction of long-curved kyphotic deformities in ankylosing spondylitis. Report on 177 cases. Clin Orthop. 1990; 258:49–55.4). Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop. 1985; 194:142–52.
Article5). Bridwell KH, Lewis SJ, Lenke LG, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg. 2003; 85-A:454–463.
Article6). Thiranont N, Netrawichien P. Transpedicular decancel -lation closed wedge vertebral osteotomy for treatment of fixed flexion deformity of spine in ankylosing spondylitis. Spine. 1993; 18:2517–22.7). Van Royen BJ, Slot GH. Closing-wedge posterior osteotomy for ankylosing spondylitis: partial corpectomy and transpedicular fixation in 22 cases. J Bone Joint Surg. 1995; 77-B:117–21.8). Booth KC, Bridwell KH, Lenke LG, et al. Complications and predictive factors for the successful treatment for flatback deformity (fixed sagittal imbalance). Spine. 1999; 24:1712–20.9). Law WA. Lumbar spinal osteotomy. J Bone Joint Surg. 1959; 41-B:270–278.
Article10). Chen IH, Chien JT, Yu TC. Transpedicular wedge osteotomy for correction of thoracolumbar kyphosis in ankylosing spondylitis. Experience with 78 patients. Spine. 2001; 26:E354–360.11). Lagrone MO, Bradford DS, Moe JH, et al. Treatment of symptomatic flatback after spinal fusion. J Bone Joint Surg. 1988; 70-A:569–80.
Article12). Voos K, Boachie-Adjei O, Rawlins BA. Multiple vertebral osteotomies in the treatment of rigid adult spine deformities. Spine. 2001; 26:526–533.
Article13). Berven SH, Deviren V, Smith JA, Emami A, Hu SH, Bradford DS. Management of fixed sagittal plane deformity: Results of the transpedicular wedge resection osteotomy. Spine. 2001; 26:2036–2043.14). Bridwell KH, Lenke LG, Lewis SJ. Treatment of spinal stenosis and fixed sagittal imbalance. Clin Orthop. 2001; 384:35–44.
Article15). McMaster MJ. A technique for lumbar spinal osteotomy in ankylosing spondylitis. J Bone Joint Surg. 1985; 67-B:204–210.
Article16). Weatherly C, Jaffray D, Terry A. Vascular complications associated with osteotomy in ankylosing spondylitis: a report of two cases. Spine. 1988; 13:43.
Article17). Adams JC. Technique, dangers and safeguards in osteotomy of the spine. J Bone Joint Surg. 1952; 34-B:226–232.
Article18). Van Royen BJ, DeGast A. Lumbar osteotomy for correction of thoracolumbar kyphotic deformity in ankylosing spondylitis: a structured review of three methods of treatment. Ann Rheum Dis. 1999; 58:399–406.
Article19). Bridwell K, Lewis SJ, Edwards C, et al. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine. 2003; 28:2093–2101.
Article20). Weale AE, Marsh CH, Yeoman PM. Secure fixation of lumbar osteotomy. Surgical experience with 50 patients. Clin Orthop. 1995; 321:216–222.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pedicle Subtraction and Extension Wedge Osteotomy for the Correction of Fixed Kyphotic Deformity of the Lumbar Spine: Technical Note
- Osteotomy of the Spine to Correct the Spinal Deformity
- Loss of Sagittal Balance and Clinical Outcomes following Corrective Osteotomy for Lumbar Degenerative Kyphosis
- Analysis of Correction Loss after Pedicle Subtraction Osteotomy in Patients with Sagittal Imbalance: Radiologic Aspects
- Changes of Spinopelvic Parameter using Iliac Screw In Surgical Correction of Sagittal Imbalance Patients