J Korean Soc Spine Surg.
2004 Dec;11(4):253-260.
Selection of the Optimal Distal Fusion Level in Posterior Instrumentation and Fusion for Thoracic Hyperkyphosis: The Sagittal Stable Vertebra Concept
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Inha University, Incheon, Korea. srp2002@inha.com
- 2Washington University, Department of Orthopedic Surgery, St. Louis, USA.
Abstract
- STUDY DESIGN: A retrospective study for clinical, radiographic assessment.
OBJECTIVES
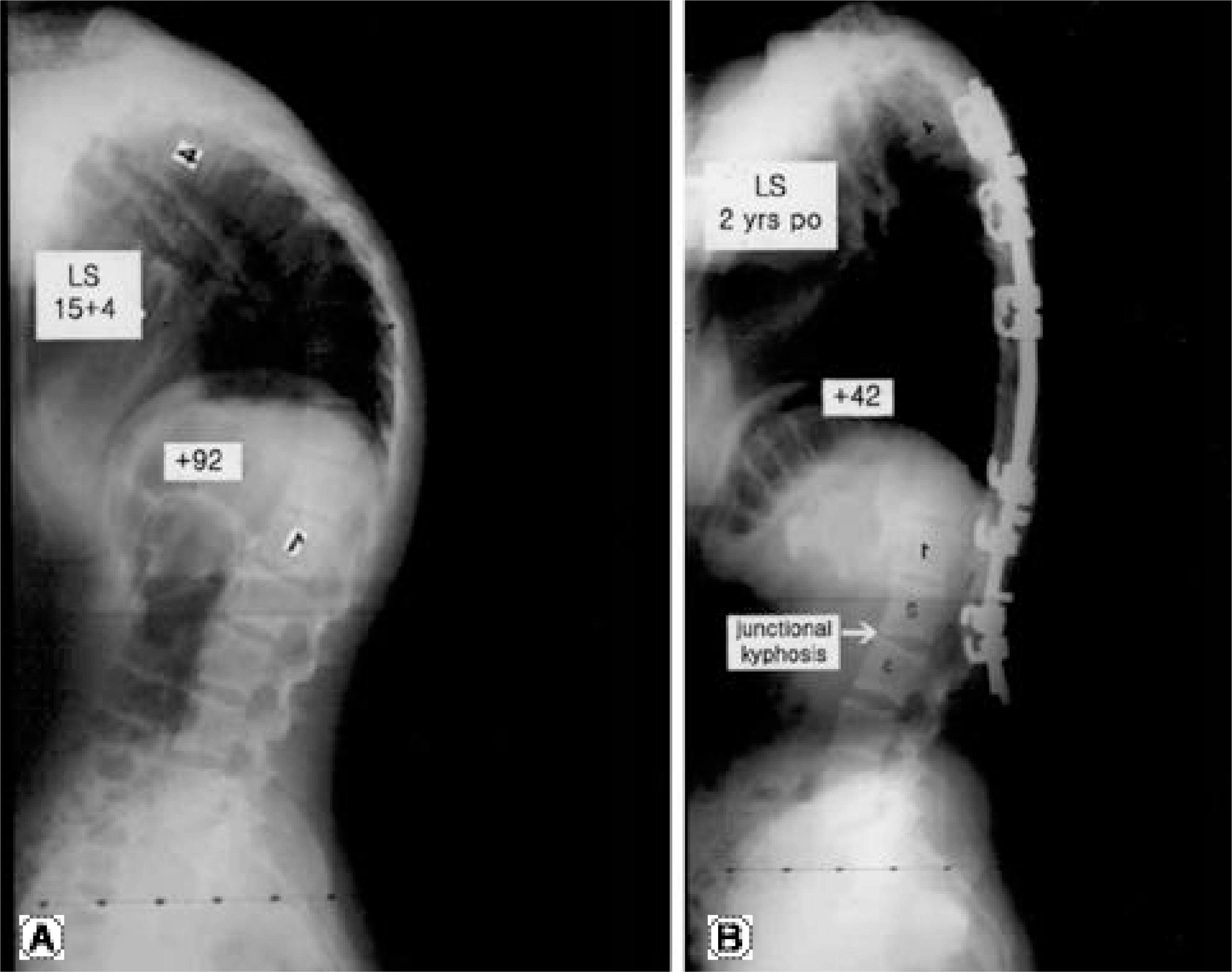
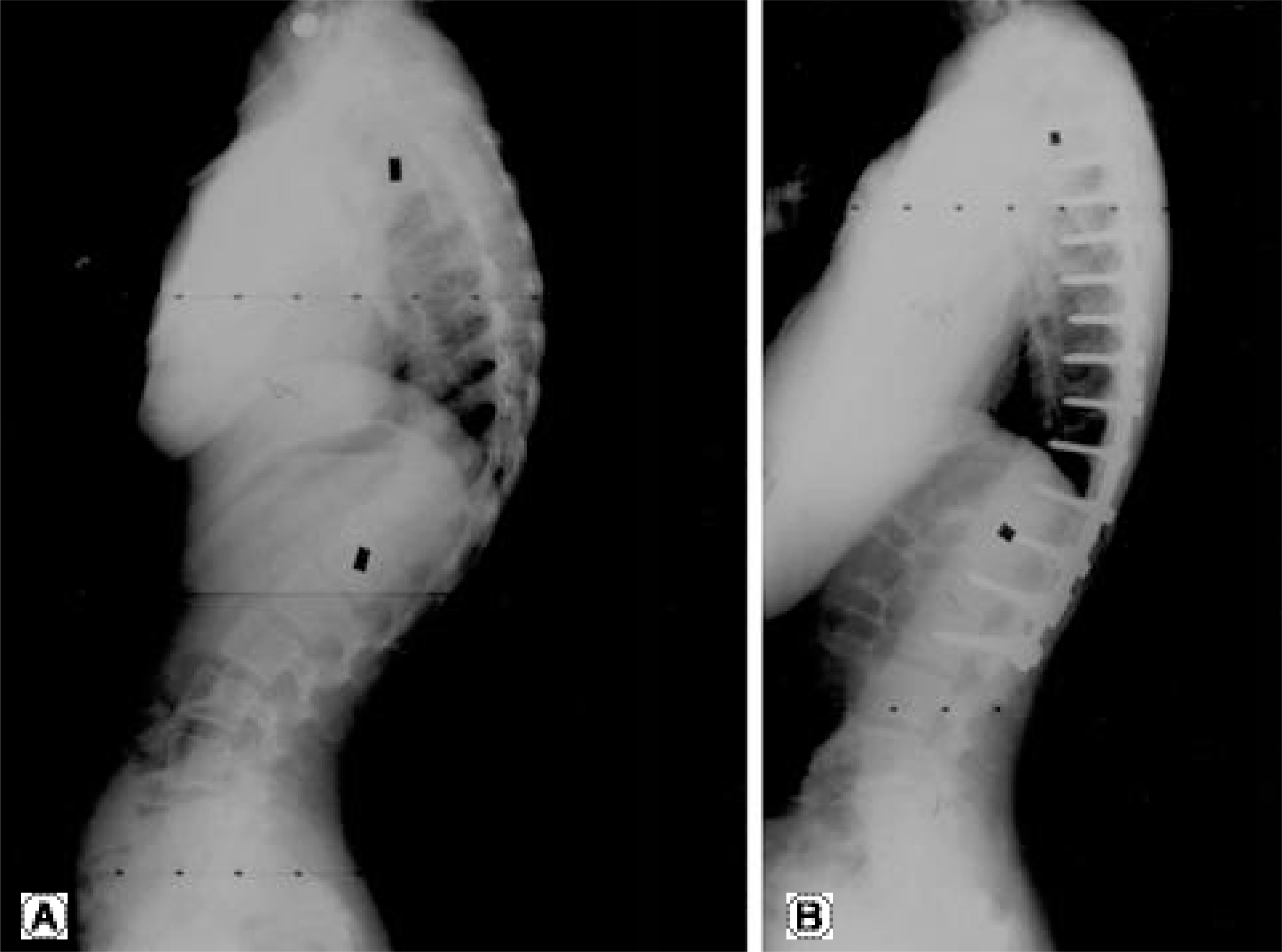
To determine the appropriate level of distal fusion for the posterior instrumentation and fusion for thoracic hyperkyphosis by investigating the relationship between the sagittal stable (the most proximal vertebra touched by the vertical line from the posterior-superior corner of the sacrum), first lordotic (just caudal to the first lordotic disc) and lowest instrumented vertebrae. LITERATURE REVIEW SUMMARY: It has been recommended that the distal level of fusion for thoracic hyperkyphosis should include not only the distal end vertebra of kyphosis, but also the first lordotic disc beyond the transitional zone, distally. However, distal junctional breakdown was noted, even when these rules have been followed.
MATERIALS AND METHODS
Thirty-one patients, with a mean age of 18, ranging from 13 to 38 years, who underwent long posterior instrumentation and fusion for thoracic hyperkyphosis, with a minimum of 2 years of follow up, were reviewed. The preoperative diagnosis included: Scheuermann`s disease (n=29), posttraumatic kyphosis (n=1) and postlaminectomy kyphosis (n=1). According to the level of distal fusion, the patients were divided into two groups. Group I (n=24): lowest instrumented vertebra (LIV), including the sagittal stable vertebra (SSV), Group II (n=7): lowest instrumented vertebra proximal to the sagittal stable vertebra. Patients were evaluated utilizing both standing radiographs and chart reviews.
RESULTS
The mean thoracic kyphosis was 86.6+/-8.5 before surgery, which had been corrected to 53.0+/-10.4 by the final follow-up, with a correction rate of 39%. The average sagittal balance was slightly negative (0.24+/-3.8 cm) before surgery, and became more negative (1.33+/-2.8 cm) by the final follow-up. There were no statistical differences in the thoracic kyphosis between the two groups. However, there was a statistically significant difference, with Group II having a more posterior translation of the center of the LIV from the posterior sacral vertical line, preoperatively, than at the final follow-up in Group I (p=0.003). In Group I, distal junctional problems developed in only 2 of the 24 (8%) patients, whereas in Group II, they occurred in 5 of the 7 (71%) patients (p<0.05). Despite extending the fusion to the first lordotic vertebra, distal junctional problems developed in 3 of the 8 (38%) patients.
CONCLUSIONS
The distal end of the fusion for thoracic hyperkyphosis should include the sagittal stable vertebra. The levels of distal fusion that include the first lordotic vertebra, but not the sagittal stable vertebra, are not always appropriate for the prevention of postoperative distal junctional kyphosis.
Figure
Reference
-
1). Ferreira-Alves A, Resina J, Palma-Rodrigues R. Scheuermann’s kyphosis. The Protuguese technique of surgical treamtment. J Bone Joint Surg. 1995; 77-B:943–950.2). Speck GR, Chopin DC. The surgical treatment of Scheuermann's kyphosis. J Bone Joint Surg. 1986; 68-B:189–193.
Article3). Sturm PF, Dobson JC, Armstrong GW. The surgical management of Scheuermann’s disease. Spine. 1993; 18:685–691.
Article4). Taylor TC, Wenger DR, Stephen J, Gillespie R, Bobechko WP. Surgical management of thoracic kyphosis in adolescents. J Bone Joint Surg. 1979; 61-A:496–503.
Article5). De Jonge T, Illes T, Bellyei A. Surgical correction of Scheuermann’s kyphosis. Int Orthop. 2001; 25:70–73.
Article6). Lowe TG, Kasten MD. An analysis of sagittal curves and balance after Cotrel-Dubousset instrumentation for kyphosis secondary to Scheuermann’s disease: a review of 32 patients. Spine. 1994; 19:1680–1685.7). Papagelopoulos PJ, Klassen RA, Peterson HA, Dekutoski MB. Surgical treatment of Scheuermann’s disease with segmental compression instrumentation. Clin Orthop. 2001; 385:139–149.
Article8). Wenger DR and Frick SL. Scheuermann kyphosis. Spine. 1999; 24:2630–2639.
Article9). Ascani E, La Rosa G. Scheuermann's kyphosis. Weinstein SL, editor. The Pediatric Spine: Principles and Practice. New York: Raven Press;1994. p. 557–584.10). Hosman AJ, Langeloo DD, de Kleuver M, Anderson PG, Veth RP, Slot GH. Analysis of the sagittal plane after surgical management for Scheuermann’s disease. Spine. 2002; 27:267–275.
Article11). Otsuka NY, Hall JE, Mah JY. Posterior fusion for Scheuermann's kyphosis. Clin Orthop. 1990; 134-139.
Article12). Bradford DS, Ahmed KB, Moe JH, et al. The surgical management of patients with Scheuermann’s disease: a review of twenty-four cases managed by combined anterior and posterior spine fusion. J Bone Joint Surg. 1980; 62-A:705–712.13). Bernhardt M, Bridwell KH. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989; 14:717–721.
Article14). King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg. 1983; 65-A:1302–1313.
Article15). Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size: a prospective controlled clinical study. Spine. 1994; 19:1611–1618.16). Herndon WA, Emans JB, Micheli LJ, Hall JE. Combined anterior and posterior fusion for Scheuermann’s kyphosis. Spine. 1981; 6:125–129.
Article17). Poolman RW, Been HD, Ubags LH. Clinical outcome and radiographic results after operative treatment of Scheuermann’s disease. Eur Spine J. 2002; 10:561–569.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Change of Segmental Sagittal angle in Low - grade spondylolisthesis after Pedicular Screw Fixation with or without PLIF - PLIF + PLF versus PLF groups -
- Indications of Proximal Thoracic Curve Fusion in Thoracic Adolescent Idiopathic Scoliosis(AIS): Recognition and Treatment of Double Thoracic Curve Pattern in Adolescent Idiopathic Scoliosis Treated with Segmental Instrumentation
- Comparison of Short Fusion versus Long Fusion for Degenerative Lumbar Scoliosis
- Sagittal Plane Lumbar Responses after Anterior Selective Thoracic Fusion for Main Thoracic Adolescent Idiopathic Scoliosis
- Acute Paraplegia Secondary to Thoracic Disc Herniation of the Adjacent Segment Following Thoracolumbar Fusion and Instrumentation