J Korean Orthop Assoc.
2007 Dec;42(6):795-802. 10.4055/jkoa.2007.42.6.795.
Comparison of Short Fusion versus Long Fusion for Degenerative Lumbar Scoliosis
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Inha University, Incheon, Korea. srp2002@inha.com
- 2Seoul Spine Institute, Inje University, Sanggye-Paik Hospital, Seoul, Korea.
- KMID: 1947787
- DOI: http://doi.org/10.4055/jkoa.2007.42.6.795
Abstract
-
PURPOSE: To compare the results of short fusion versus long fusion for degenerative lumbar scoliosis.
MATERIALS AND METHODS
Forty-seven patients undergoing short fusion (n=28) and long fusion and instrumentation (n=19) were evaluated. Short fusion was defined as fusion within the deformity, not exceeding the upper end vertebra. Long fusion was defined as fusion extended above the upper end vertebra. The number of levels fused in the short and long fusion groups was 3.14 and 6.89 segments, respectively.
RESULTS
Before surgery, the Cobb angle was 16.3 degrees in the short fusion group and 22 degrees in the long fusion group, which changed to 10.1 degrees and 8.47 degrees, respectively, at the last visit. The correction of coronal imbalance was better in the long fusion group. In contrast, the correction of sagittal imbalance was similar in both groups. The mean estimated blood loss in the short and long fusion groups was 1,671 ml and 2,742 ml, respectively. Early perioperative complications developed frequently in the long fusion group. Adjacent segment disease occurred more frequently in the short fusion group.
CONCLUSION
Long fusion and instrumentation for degenerative lumbar scoliosis was better at correcting the coronal deformity and imbalance than short fusion but was ineffective in correcting the sagittal imbalance.
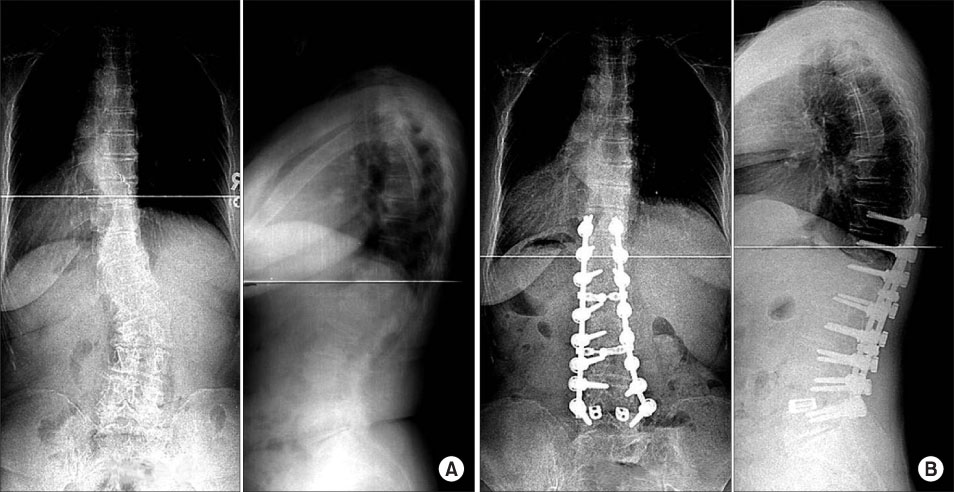
Figure
Cited by 1 articles
-
Treatment of Multiple Thoracolumbar and Lumbar Spine Fractures: Comparison of Contiguous and Non-Contiguous Fractures in Non-Osteoporotic Patients
Yi Gyu Park, Sin Wook Kang, Hong Moon Sohn
J Korean Soc Spine Surg. 2018;25(1):9-17. doi: 10.4184/jkss.2018.25.1.9.
Reference
-
1. Aebi M. The adult scoliosis. Eur Spine J. 2005. 14:925–948.
Article2. Bradford DS, Tay BK, Hu SS. Adult scoliosis: surgical indications, operative management, complications, and outcomes. Spine. 1999. 24:2617–2629.
Article3. Bridwell KH, Edwards CC 2nd, Lenke LG. The pros and cons to saving the L5-S1 motion segment in a long scoliosis fusion construct. Spine. 2003. 28:S234–S242.
Article4. Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003. 85:2089–2092.
Article5. Daffner SD, Vaccaro A. Adult degenerative lumbar scoliosis. Am J Orthop. 2003. 32:77–82.6. Grubb SA, Lipscomb HJ, Suh PB. Results of surgical treatment of painful adult scoliosis. Spine. 1994. 19:1619–1627.
Article7. Gupta MC. Degenerative scoliosis. Options for surgical management. Orthop Clin North Am. 2003. 34:269–279.8. Kim YT, Lee CS, Kim JH, Kim JM, Park JH. Clinical features of degenerative scoliosis. J Korean Spine Soc Surg. 2001. 8:15–20.
Article9. Marchesi DG, Aebi M. Pedicle fixation devices in the treatment of adult lumbar scoliosis. Spine. 1992. 17:S304–S309.
Article10. Pritchett JW, Bortel DT. Degenerative symptomatic lumbar scoliosis. Spine. 1993. 18:700–703.
Article11. Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine. 2002. 27:387–392.12. Shufflebarger H, Suk SI, Mardjetko S. Debate: determining the upper instrumented vertebra in the management of adult degenerative scoliosis: stopping at T10 versus L1. Spine. 2006. 31:S185–S194.13. Simmons ED. Surgical treatment of patients with lumbar spinal stenosis with associated scoliosis. Clin Orthop Relat Res. 2001. 384:45–53.
Article14. Simmons ED Jr, Simmons EH. Spinal stenosis with scoliosis. Spine. 1992. 17:S117–S120.
Article15. Tribus CB. Degenerative lumbar scoliosis: evaluation and management. J Am Acad Orthop Surg. 2003. 11:174–183.
Article16. Vaccaro AR, Ball ST. Indications for instrumentation in degenerative lumbar spinal disorders. Orthopedics. 2000. 23:260–271.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiographic Progression of Degenerative Lumbar Scoliosis after Short Segment Decompression and Fusion
- Surgical Treatment of Adult Degenerative Scoliosis
- Lumbosacral Fixation Using the Diagonal S2 Screw for Long Fusion in Degenerative Lumbar Deformity: Technical Note Involving 13 Cases
- Principles of Lumbar Spine Stabilization
- Posterior Lumbar Interbody Fusion in Multilevel Lumbar Spinal Stenosis Associated with Degenerative Scoliosis