J Korean Soc Spine Surg.
2011 Sep;18(3):83-90.
Epidemiology of the Spinal Cord and Cauda Equina Injury in Korea: Multicenter Study
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chungnam National University School of Medicine, Daejeon, Korea. jyyang@cnu.ac.kr
- 2Department of Orthopaedic Surgery, School of Medicine, Wonkwang University Hospital, Iksan, Korea.
- 3Department of Orthopaedic Surgery, College of Medicine, Yonsei University, Seoul, Korea.
- 4Department of Orthopaedic Surgery, College of Medicine, Chosun University, Gwangju, Korea.
- 5Department of Orthopedic Surgery, Soonchunhyang University College of Medicine, Cheonan, Korea.
- 6Department of Orthopaedic Surgery, College of Medicine, The Catholic University of Korea.
Abstract
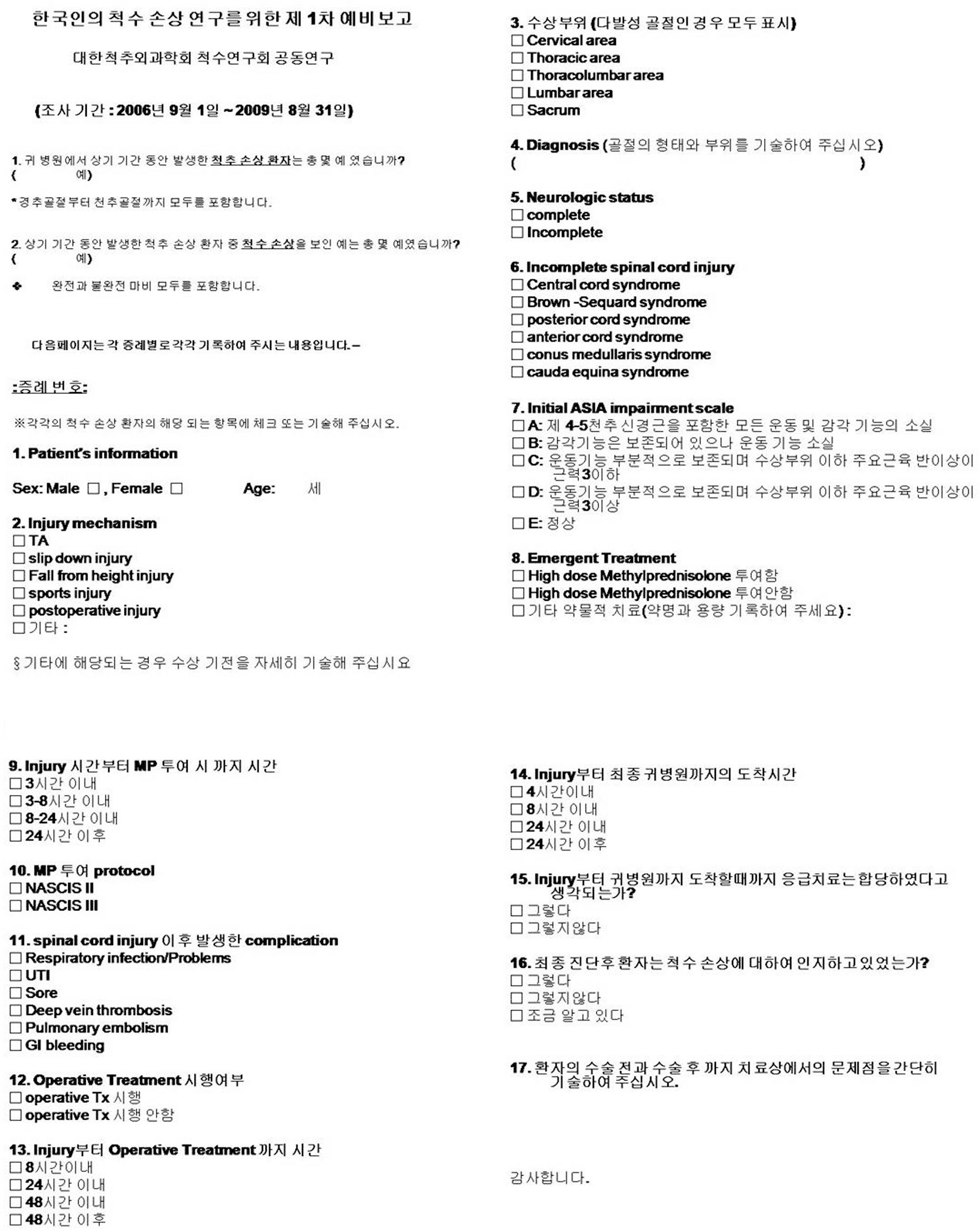
- STUDY DESIGN: Multi-center study, questionnaire survey.
OBJECTIVES
To offer a database of spinal cord injury (SCI) by reviewing statistics and literatures of other countries, investigating the overall mechanism, injury patterns and treatment of SCI. SUMMARY OF LITERATURE REVIEW: There are no preexisting domestic studies (collectively conducted by multi-centers) of the prevalence and treatment of SCI.
MATERIALS AND METHODS
From September 2006 to August 2009, 47 cases of SCI in 6 universities were investigated retrospectively. 17 questionnaire contents including the courses of injury-to-treatment were studied with data gathered from surveys.
RESULTS
The average age of patients was 48.4-years-old, male to female ratio was 33 to 14. The cases of falling from a height were 22 cases (47%), lumbar area 19 cases (40%), and unstable bursting fracture 24 cases (51%) the most. Complete and incomplete paralyses were 19 cases (40%) and 28 cases (60%), respectively. High dose steroids were injected in 16 cases (NASCIS II) and 9 cases (NASCIS III). 14 cases presented complications and operations were performed 46 cases (98%). 12 cases (26%) arrived at the hospital within 4 hours of injury, 11 cases (23%) in 8 hours. On the way to the hospital, proper emergency treatment was performed in 25 cases (53%), and 30 cases (64%) had a clear understanding of SCI after the final diagnosis.
CONCLUSIONS
This is the first study that offers a comprehensive database of spinal cord injury (SCI), by investigating the overall mechanism, injury patterns, and treatment of SCI; this study is expected to be used in the future as an important reference material for spinal cord injury statistics and a standard for care.
Keyword
MeSH Terms
Figure
Reference
-
1. Yang JY, Lee JK, Hong CH, Woo SM. Assessment of Quality of Life and Psychological Status in Spinal Cord Injury after Spinal Fracture. J Korean Soc Spine Surg. 2004; 11:285–90.
Article2. Na YW, Park CI, Chun S, Shin JS. Complications in spinal cord injured patients. J Korean Acad Rehabil Med. 1991; 15:12–21.3. Lee JK. Pathophysiology of Acute Spinal Cord Injury. J Korean Soc Spine Surg. 2009; 16:64–70.
Article4. Young JS, Burns PE, Bowen AM, McCutchen R. Spinal cord injury statistics: Experience of the regional spinal cord injury system. Good Samaritan Medical Center. Phoenix. Arizona. 1982.5. Eric S, Christine P, Michael W. Review of spinal cord injury statistics related to diving and diving board use. American Institutes for Research;2003.6. Stover SL, Fine PR. The epidemiology and economics of spinal cord injury. Paraplegia. 1987; 25:225–8.
Article7. French DD, Campbell RR, Sabharwal S, Nelson AL, Palacios PA, Gavin-Dreschnack D. Health care costs for patients with chronic spinal cord injury in the Veterans Health Administration. J Spinal Cord Med. 2007; 30:477–81.
Article8. Bracken MB, Shepard MJ, Collins WF, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med. 1990; 322:1405–11.9. Molloy S, Middleton F, Casey AT. Failure to administer methylprednisolone for acute traumatic spinal cord injury-a prospective audit of 100 patients from a regional spinal injuries unit. Injury. 2002; 33:575–8.
Article10. Frampton AE, Eynon CA. High dose methylprednisolone in the immediate management of acute, blunt spinal cord injury: what is the current practice in emergency departments, spinal units, and neurosurgical units in the UK? Emerg Med J. 2006; 23:550–3.
Article11. Eck JC, Nachtigall D, Humphreys SC, Hodges SD. Questionnaire survey of spine surgeons on the use of methylprednisolone for acute spinal cord injury. Spine (Phila Pa 1976). 2006; 31:E250–3.
Article12. Molloy S, Price M, Casey AT. Questionnaire survey of the views of the delegates at the European Cervical Spine Research Society meeting on the administration of methylprednisolone for acute traumatic spinal cord injury. Spine (Phila Pa 1976). 2001; 26:E562–4.
Article13. McCutcheon EP, Selassie AW, Gu JK, Pickelsimer EE. Acute traumatic spinal cord injury, 1993-2000A population-based assessment of methylprednisolone administration and hospitalization. J Trauma. 2004; 5:1076–83.
Article14. Ito Y, Sugimoto Y, Tomioka M, Kai N, Tanaka M. Does high dose methylprednisolone sodium succinate really improve neurological status in patient with acute cervical cord injury?: a prospective study about neurological recovery and early complications. Spine (Phila Pa 1976). 2009; 34:2121–4.15. Hurlbert RJ, Hamilton MG. Methylprednisolone for acute spinal cord injury: 5-year practice reversal. The Can J Neurol Sci. 2008; 35:41–5.
Article16. Peter Vellman W, Hawkes AP, Lammertse DP. Administration of corticosteroids for acute spinal cord injury: the current practice of trauma medical directors and emergency medical system physician advisors. Spine (Phila Pa 1976). 2003; 28:941–7.17. Eck JC, Nachtigall D, Humphreys SC, Hodges SD. Questionnaire survey of spine surgeons on the use of methylprednisolone for acute spinal cord injury. Spine (Phila Pa 1976). 2006; 31:E250–3.
Article18. Menon EB, Tan ES. Urinary tract infection in acute spinal cord injury. Singapore Med J. 1992; 33:359–61.19. Perkash I, Giroux J. Prevention, treatment, and management of urinary tract infections in neuropathic bladders. J Am Paraplegia Soc. 1985; 8:15–7.
Article20. Liguori PA, Cardenas DD, Ullrich P. Social and functional variables associated with urinary tract infections in persons with spinal cord injury. Arch Phys Med Rehabil. 1997; 78:156–60.
Article21. Kim NH, Lee HM, Chun IM. Neurologic injury and recovery in patients with burst fracture of the thoracolumbar spine. Spine (Phila Pa 1976). 1999; 24:290–3.
Article22. Guttmann L, Frankel H. The value of intermittent catheterisation in the early management of traumatic paraplegia and tetraplegia. Paraplegia. 1966; 4:63–84.
Article23. Munro D. Thoracic and lumbar cord injuries. JAMA. 1943; 122:1055.24. Biering-S⊘rensen E, Pedersen V, Clausen S. Epidemiology of spinal cord lesions in Denmark. Paraplegia. 1990; 28:105–18.25. Tyroch AH, Davis JW, Kapaus KL, Lorenzo M. Spinal cord injury. A preventable public burden. Arch Surg. 1997; 132:778–81.26. Rish BL, Dilustro JF, Salazar AM, Schwab KA, Brown HR. Spinal cord injury: a 25-year morbidity and mortality study. Mil Med. 1997; 162:141–8.27. Hartkopp A, Br⊘nnum-Hansen H, Seidenschnur AM, Biering-S⊘rensen F. Survival and cause of death after traumatic spinal cord injury. A longterm epidemiological survey from Denmark. Spinal Cord. 1997; 35:76–85.
Article28. Johnson RL, Brooks CA, Whiteneck GG. Cost of traumatic spinal cord injury in a population-based registry. Spinal Cord. 1996; 34:470–80.
Article