J Korean Neurosurg Soc.
2016 Jul;59(4):363-367. 10.3340/jkns.2016.59.4.363.
Matched Comparison of Fusion Rates between Hydroxyapatite Demineralized Bone Matrix and Autograft in Lumbar Interbody Fusion
- Affiliations
-
- 1Department of Neurosurgery, Spine and Spinal Cord Institute, Yonsei University College of Medicine, Seoul, Korea. hayoon@yuhs.ac
- KMID: 2315971
- DOI: http://doi.org/10.3340/jkns.2016.59.4.363
Abstract
OBJECTIVE
To compare the fusion rate of a hydroxyapatite demineralized bone matrix (DBM) with post-laminectomy acquired autograft in lumbar interbody fusion surgery and to evaluate the correlation between fusion rate and clinical outcome.
METHODS
From January 2013 to April 2014, 98 patients underwent lumbar interbody fusion surgery with hydroxyapatite DBM (HA-DBM group) in our institute. Of those patients, 65 received complete CT scans for 12 months postoperatively in order to evaluate fusion status. For comparison with autograft, we selected another 65 patients who underwent lumbar interbody fusion surgery with post-laminectomy acquired autograft (Autograft group) during the same period. Both fusion material groups were matched in terms of age, sex, body mass index (BMI), and bone mineral density (BMD). To evaluate the clinical outcomes, we analyzed the results of visual analogue scale (VAS), Oswestry Disability Index (ODI), and Short Form Health Survey (SF-36).
RESULTS
We reviewed the CT scans of 149 fusion levels in 130 patients (HA-DBM group, 75 levels/65 patients; Autograft group, 74 levels/65 patients). Age, sex, BMI, and BMD were not significantly different between the groups (p=0.528, p=0.848, p=0.527, and p=0.610, respectively). The HA-DBM group showed 39 of 75 fused levels (52%), and the Autograft group showed 46 of 74 fused levels (62.2%). This difference was not statistically significant (p=0.21). In the HA-DBM group, older age and low BMD were significantly associated with non-fusion (61.24 vs. 66.68, p=0.027; -1.63 vs. -2.29, p=0.015, respectively). VAS and ODI showed significant improvement after surgery when fusion was successfully achieved in both groups (p=0.004, p=0.002, HA-DBM group; p=0.012, p=0.03, Autograft group).
CONCLUSION
The fusion rates of the hydroxyapatite DBM and Autograft groups were not significantly different. In addition, clinical outcomes were similar between the groups. However, older age and low BMD are risk factors that might induce non-union after surgery with hydroxyapatite DBM.
Keyword
MeSH Terms
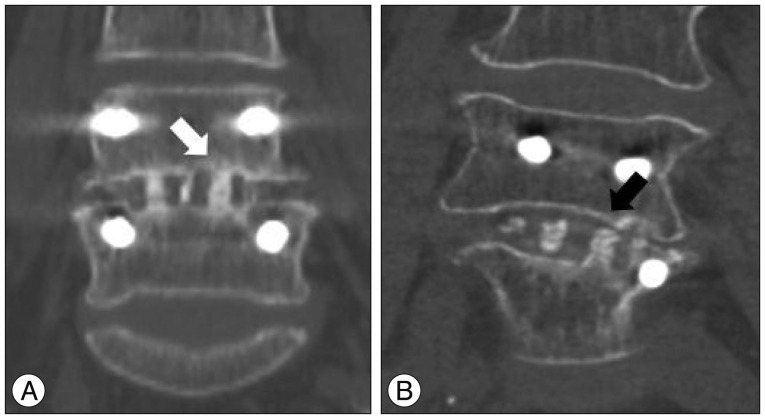
Figure
Cited by 1 articles
-
Demineralized Bone Matrix (DBM) as a Bone Void Filler in Lumbar Interbody Fusion: A Prospective Pilot Study of Simultaneous DBM and Autologous Bone Grafts
Bum-Joon Kim, Se-Hoon Kim, Haebin Lee, Seung-Hwan Lee, Won-Hyung Kim, Sung-Won Jin
J Korean Neurosurg Soc. 2017;60(2):225-231. doi: 10.3340/jkns.2017.0101.006.
Reference
-
1. Agrillo U, Mastronardi L, Puzzilli F. Anterior cervical fusion with carbon fiber cage containing coralline hydroxyapatite : preliminary observations in 45 consecutive cases of soft-disc herniation. J Neurosurg. 2002; 96(3 Suppl):273–276. PMID: 11990834.
Article2. An HS, Simpson JM, Glover JM, Stephany J. Comparison between allograft plus demineralized bone matrix versus autograft in anterior cervical fusion. A prospective multicenter study. Spine (Phila Pa 1976). 1995; 20:2211–2216. PMID: 8545714.
Article3. Andersen T, Christensen FB, Laursen M, Høy K, Hansen ES, Bünger C. Smoking as a predictor of negative outcome in lumbar spinal fusion. Spine (Phila Pa 1976). 2001; 26:2623–2628. PMID: 11725245.
Article4. Antoni M, Charles YP, Walter A, Schuller S, Steib JP. Fusion rates of different anterior grafts in thoracolumbar fractures. J Spinal Disord Tech. 2015; 28:E528–E533. PMID: 24077416.
Article5. Bak B, Andreassen TT. The effect of aging on fracture healing in the rat. Calcif Tissue Int. 1989; 45:292–297. PMID: 2509018.
Article6. Boden SD. Bone repair and enhancement clinical trial design. Spine applications. Clin Orthop Relat Res. 1998; (355 Suppl):S336–S346. PMID: 9917652.7. Bono CM, Lee CK. Critical analysis of trends in fusion for degenerative disc disease over the past 20 years : influence of technique on fusion rate and clinical outcome. Spine (Phila Pa 1976). 2004; 29:455–463. discussion Z5. PMID: 15094543.
Article8. Cammisa FP Jr, Lowery G, Garfin SR, Geisler FH, Klara PM, McGuire RA, et al. Two-year fusion rate equivalency between Grafton DBM gel and autograft in posterolateral spine fusion : a prospective controlled trial employing a side-by-side comparison in the same patient. Spine (Phila Pa 1976). 2004; 29:660–666. PMID: 15014276.
Article9. Carreon LY, Glassman SD, Djurasovic M. Reliability and agreement between fine-cut CT scans and plain radiography in the evaluation of posterolateral fusions. Spine J. 2007; 7:39–43. PMID: 17197331.
Article10. Dimar JR, Glassman SD, Burkus KJ, Carreon LY. Clinical outcomes and fusion success at 2 years of single-level instrumented posterolateral fusions with recombinant human bone morphogenetic protein-2/compression resistant matrix versus iliac crest bone graft. Spine (Phila Pa 1976). 2006; 31:2534–2539. discussion 2540. PMID: 17047540.
Article11. Finkemeier CG. Bone-grafting and bone-graft substitutes. J Bone Joint Surg Am. 2002; 84-A:454–464. PMID: 11886919.
Article12. Glassman SD, Alegre G, Carreon L, Dimar JR, Johnson JR. Perioperative complications of lumbar instrumentation and fusion in patients with diabetes mellitus. Spine J. 2003; 3:496–501. PMID: 14609695.
Article13. Glassman SD, Carreon L, Djurasovic M, Campbell MJ, Puno RM, Johnson JR, et al. Posterolateral lumbar spine fusion with INFUSE bone graft. Spine J. 2007; 7:44–49. PMID: 17197332.
Article14. Inoue K, Ohgushi H, Yoshikawa T, Okumura M, Sempuku T, Tamai S, et al. The effect of aging on bone formation in porous hydroxyapatite : biochemical and histological analysis. J Bone Miner Res. 1997; 12:989–994. PMID: 9169360.
Article15. Ito Z, Matsuyama Y, Sakai Y, Imagama S, Wakao N, Ando K, et al. Bone union rate with autologous iliac bone versus local bone graft in posterior lumbar interbody fusion. Spine (Phila Pa 1976). 2010; 35:E1101–E1105. PMID: 20885279.
Article16. Kang J, An H, Hilibrand A, Yoon ST, Kavanagh E, Boden S. Grafton and local bone have comparable outcomes to iliac crest bone in instrumented single-level lumbar fusions. Spine (Phila Pa 1976). 2012; 37:1083–1091. PMID: 22076647.
Article17. Ko KI, Coimbra LS, Tian C, Alblowi J, Kayal RA, Einhorn TA, et al. Diabetes reduces mesenchymal stem cells in fracture healing through a TNFα-mediated mechanism. Diabetologia. 2015; 58:633–642. PMID: 25563724.
Article18. Koerner JD, Yalamanchili P, Munoz W, Uko L, Chaudhary SB, Lin SS, et al. The effects of local insulin application to lumbar spinal fusions in a rat model. Spine J. 2013; 13:22–31. PMID: 23295034.
Article19. Lee HS, Lee JH, Lee JH. A comparison of dynamic views using plain radiographs and thin-section three-dimensional computed tomography in the evaluation of fusion after posterior lumbar interbody fusion surgery. Spine J. 2013; 13:1200–1207. PMID: 24075026.
Article20. Lee JH, Lee KM, Baek HR, Jang SJ, Lee JH, Ryu HS. Combined effects of porous hydroxyapatite and demineralized bone matrix on bone induction : in vitro and in vivo study using a nude rat model. Biomed Mater. 2011; 6:015008. PMID: 21205997.21. Lee KJ, Roper JG, Wang JC. Demineralized bone matrix and spinal arthrodesis. Spine J. 2005; 5(6 Suppl):217S–223S. PMID: 16291116.
Article22. Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Influence of bone mineral density on pedicle screw fixation : a study of pedicle screw fixation augmenting posterior lumbar interbody fusion in elderly patients. Spine J. 2001; 1:402–407. PMID: 14588296.23. Suetsuna F, Yokoyama T, Kenuka E, Harata S. Anterior cervical fusion using porous hydroxyapatite ceramics for cervical disc herniation. A two-year follow-up. Spine J. 2001; 1:348–357. PMID: 14588314.
Article24. Tan GH, Goss BG, Thorpe PJ, Williams RP. CT-based classification of long spinal allograft fusion. Eur Spine J. 2007; 16:1875–1881. PMID: 17497188.
Article25. Thalgott JS, Giuffre JM, Fritts K, Timlin M, Klezl Z. Instrumented posterolateral lumbar fusion using coralline hydroxyapatite with or without demineralized bone matrix, as an adjunct to autologous bone. Spine J. 2001; 1:131–137. PMID: 14588393.
Article26. Yi J, Lee GW, Nam WD, Han KY, Kim MH, Kang JW, et al. A prospective randomized clinical trial comparing bone union rate following anterior cervical discectomy and fusion using a polyetheretherketone cage : hydroxyapatite/B-tricalcium phosphate mixture versus hydroxyapatite/demineralized bone matrix mixture. Asian Spine J. 2015; 9:30–38. PMID: 25705332.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Clinical and Radiological Outcomes of Lumbar Interbody Fusion Using a Combination of Hydroxyapatite and Demineralized Bone Matrix and Autografts for Lumbar Degenerative Spondylolisthesis
- Comparison of Fusion Rate between Demineralized Bone Matrix versus Autograft in Lumbar Fusion : Meta-Analysis
- Lumbar Posterolateral Fusion Using Demineralized Bone Matrix
- Volumetric Assessment of Fusion Mass and Its Clinical Correlations in Posterior Lumbar Interbody Fusion Depending on the Type of Bone Graft
- Bone Union Rate Following Instrumented Posterolateral Lumbar Fusion: Comparison between Demineralized Bone Matrix versus Hydroxyapatite