Korean J Urol.
2011 Jan;52(1):49-54.
Impact of Lower Urinary Tract Symptoms/Benign Prostatic Hyperplasia Treatment with Tamsulosin and Solifenacin Combination Therapy on Erectile Function
- Affiliations
-
- 1Department of Urology, College of Medicine, Gyeongsang National University, Jinju, Korea. hyunjs@gnu.ac.kr
Abstract
- PURPOSE
To examine the effects on erectile function of concomitant treatment with an alpha-blocker (tamsulosin) and an antimuscarinic agent (solifenacin) in patients with lower urinary tract symptoms (LUTS)/benign prostatic hyperplasia (BPH).
MATERIALS AND METHODS
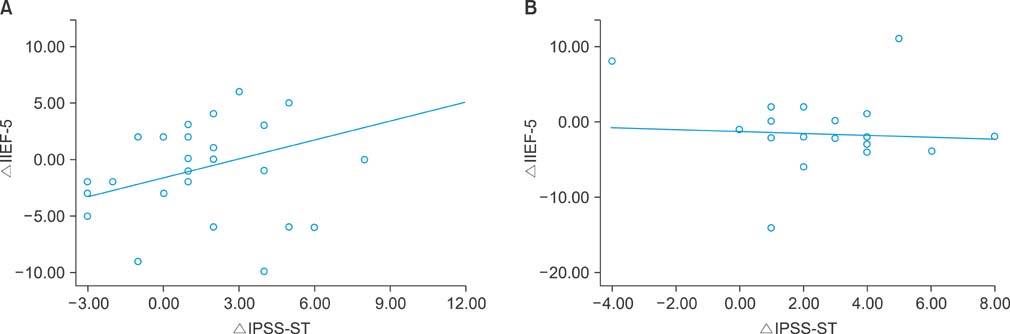
Fifty-seven male patients with LUTS/BPH were assessed for the degree of LUTS and erectile function. In group 1 (tamsulosin) and group 2 (tamsulosin and solifenacin), changes in the International Prostate Symptom Score [IPSS: total scores, storage symptoms (ST), voiding symptoms (VD), and quality of life (QoL)], prostate-specific antigen, trans-rectal ultrasonography, urine flowmetry, residual urine, and a 5-item version of the International Index of Erectile Function (IIEF-5) were assessed after a 3-month treatment period. In both groups, it was determined whether treatment was associated with changes in LUTS and erectile function and whether improvement in the IPSS was correlated with the IIEF-5. Comparative analysis was also done to examine the linear relationship between improved IPSS scores and IIEF-5 scores.
RESULTS
A comparison of the degree of improvement in all the parameters indicated that both groups showed significant improvement in total IPSS, IPSS-ST, IPSS-VD, and IPSS-QoL (p<0.05). A comparison of the degree of improved sexual function associated with improved LUTS in each patient showed significant improvement in the IIEF-5 score associated with the degree of improvement in the IPSS-ST domain in group 1, but no significant associations were found in group 2. In cases in which tamsulosin was administered, the IIEF-5 score significantly improved as the IPSS-ST domain score improved. In the group in which tamsulosin and solifenacin were concomitantly administered, improvement of the IPSS-ST domain score had no significant effect on the IIEF-5 score.
CONCLUSIONS
In patients with LUTS/BPH, tamsulosin and solifenacin combination therapy was effective for LUTS, but erectile function was not significantly improved. Therefore, although effective for improving LUTS, combination therapy with an alpha-blocker and an antimuscarinic agent was not effective for improving erectile function.
MeSH Terms
-
Humans
Lower Urinary Tract Symptoms
Male
Prostate
Prostate-Specific Antigen
Prostatic Hyperplasia
Quality of Life
Quinuclidines
Rheology
Sexual Dysfunction, Physiological
Sulfonamides
Tetrahydroisoquinolines
Urinary Tract
Solifenacin Succinate
Prostate-Specific Antigen
Quinuclidines
Sulfonamides
Tetrahydroisoquinolines
Figure
Reference
-
1. Rosen RC, Wei JT, Althof SE, Seftel AD, Miner M, Perelman MA. Association of sexual dysfunction with lower urinary tract symptoms of BPH and BPH medical therapies: results from the BPH Registry. Urology. 2009. 73:562–566.2. Taylor JM, Desouza R, Wang R. Common approach to managing lower urinary tract symptoms and erectile dysfunction. Asian J Androl. 2008. 10:45–53.3. McVary KT, McKenna KE. The relationship between erectile dysfunction and lower urinary tract symptoms: epidemiological, clinical, and basic science evidence. Curr Urol Rep. 2004. 5:251–257.4. McVary KT. Erectile dysfunction and lower urinary tract symptoms secondary to BPH. Eur Urol. 2005. 47:838–845.5. Rosen RC, Giuliano F, Carson CC. Sexual dysfunction and lower urinary tract symptoms (LUTS) associated with benign prostatic hyperplasia (BPH). Eur Urol. 2005. 47:824–837.6. Jung JH, Jae SU, Kam SC, Hyun JS. Correlation between lower urinary tract symptoms (LUTS) and sexual function in benign prostatic hyperplasia: impact of treatment of LUTS on sexual function. J Sex Med. 2009. 6:2299–2304.7. Irwin DE, Milsom I, Reilly K, Hunskaar S, Kopp Z, Herschorn S, et al. Overactive bladder is associated with erectile dysfunction and reduced sexual quality of life in men. J Sex Med. 2008. 5:2904–2910.8. Chung BH, Lee JY, Lee SH, Yoo SJ, Lee SW, Oh CY. Safety and efficacy of the simultaneous administration of udenafil and an alpha-blocker in men with erectile dysfunction concomitant with BPH/LUTS. Int J Impot Res. 2009. 21:122–128.9. Nickel JC, Elhilali M, Emberton M, Vallancien G. The beneficial effect of alfuzosin 10 mg once daily in 'real-life' practice on lower urinary tract symptoms (LUTS), quality of life and sexual dysfunction in men with LUTS and painful ejaculation. BJU Int. 2006. 97:1242–1246.10. Rhoden EL, Riedner CE, Fornari A, Fuchs SC, Ribeiro EP. Evaluation of the association between lower urinary tract symptoms and erectile dysfunction, considering its multiple risk factors. J Sex Med. 2008. 5:2662–2668.11. Lowe FC. Treatment of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: sexual function. BJU Int. 2005. 95:Suppl 4. 12–18.12. Köhler TS, McVary KT. The relationship between erectile dysfunction and lower urinary tract symptoms and the role of phosphodiesterase type 5 inhibitors. Eur Urol. 2009. 55:38–48.13. Rosen R, Altwein J, Boyle P, Kirby RS, Lukacs B, Meuleman E, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7). Eur Urol. 2003. 44:637–649.14. Morant S, Bloomfield G, Vats V, Chapple C. Increased sexual dysfunction in men with storage and voiding lower urinary tract symptoms. J Sex Med. 2009. 6:1103–1110.15. Tsai CC, Liu CC, Huang SP, Li WM, Wu WJ, Huang CH, et al. The impact of irritative lower urinary tract symptoms on erectile dysfunction in aging Taiwanese males. Aging Male. 2010. 13:179–183.16. Rosier PF, de la Rosette JJ, Wijkstra H, Van Kerrebroeck PE, Debruyne FM. Is detrusor instability in elderly males related to the grade of obstruction? Neurourol Urodyn. 1995. 14:625–633.17. Mitterberger M, Pallwein L, Gradl J, Frauscher F, Neuwirt H, Leunhartsberger N, et al. Persistent detrusor overactivity after transurethral resection of the prostate is associated with reduced perfusion of the urinary bladder. BJU Int. 2007. 99:831–835.18. Abrams P, Kelleher CJ, Kerr LA, Rogers RG. Overactive bladder significantly affects quality of life. Am J Manag Care. 2000. 6:11 Suppl. S580–S590.19. Novara G, Galfano A, Ficarra V, Artibani W. Anticholinergic drugs in patients with bladder outlet obstruction and lower urinary tract symptoms: a systematic review. Eur Urol. 2006. 50:675–683.20. Gallegos PJ, Frazee LA. Anticholinergic therapy for lower urinary tract symptoms associated with benign prostatic hyperplasia. Pharmacotherapy. 2008. 28:356–365.21. Kaplan SA, Roehrborn CG, Chancellor M, Carlsson M, Bavendam T, Guan Z. Extended-release tolterodine with or without tamsulosin in men with lower urinary tract symptoms and overactive bladder: effects on urinary symptoms assessed by the International Prostate Symptom Score. BJU Int. 2008. 102:1133–1139.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Benign Prostatic Hyperplasia and Sexual Dysfunction
- The Experience with Combination of Finasteride and Tamsulosin on Benign Prostatic Hyperplasia
- The Effect of Finasteride, Tamsulosin and Doxazosin Therapy on Sexual Function in Patients with Benign Prostatic Hyperplasia
- The Relationship between Benign Prostate Hyperplasia and Erectile Dysfunction: What is Reality?
- Improvement of Lower Urinary Tract Symptoms and Sexual Function after Treatment with Alpha-Blocker