Korean J Urol.
2011 Feb;52(2):130-135.
Realistic Anatomical Prostate Models for Surgical Skills Workshops Using Ballistic Gelatin for Nerve-Sparing Radical Prostatectomy and Fruit for Simple Prostatectomy
- Affiliations
-
- 1Department of Urology and Surgical Oncology, Princess Margaret Hospital, University of Toronto, Toronto, Canada. lawrentschuk@gmail.com
- 2Department of Urology, University of Toronto, Sunnybrook Health Sciences Centre, Toronto, Canada.
Abstract
- PURPOSE
Understanding of prostate anatomy has evolved as techniques have been refined and improved for radical prostatectomy (RP), particularly regarding the importance of the neurovascular bundles for erectile function. The objectives of this study were to develop inexpensive and simple but anatomically accurate prostate models not involving human or animal elements to teach the terminology and practical aspects of nerve-sparing RP and simple prostatectomy (SP).
MATERIALS AND METHODS
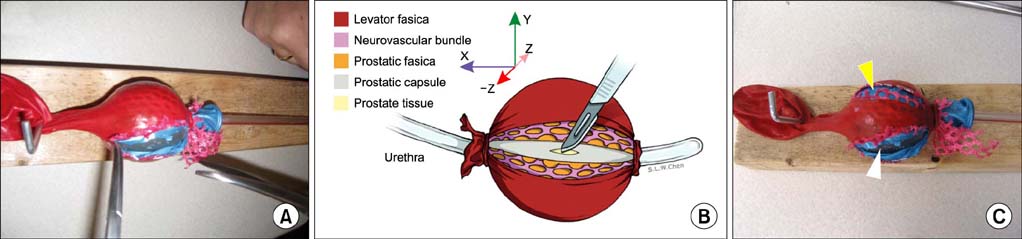
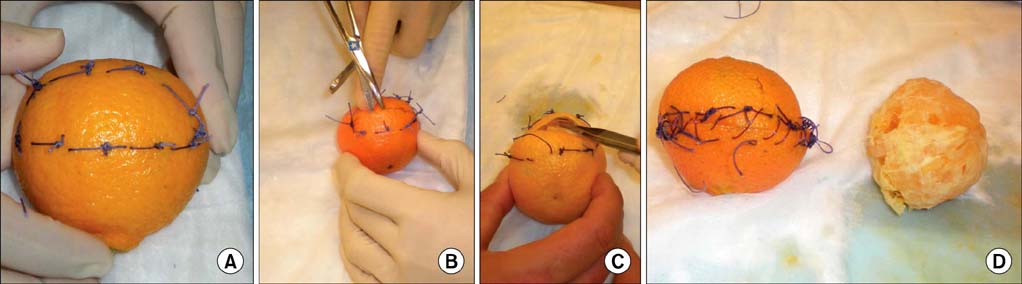
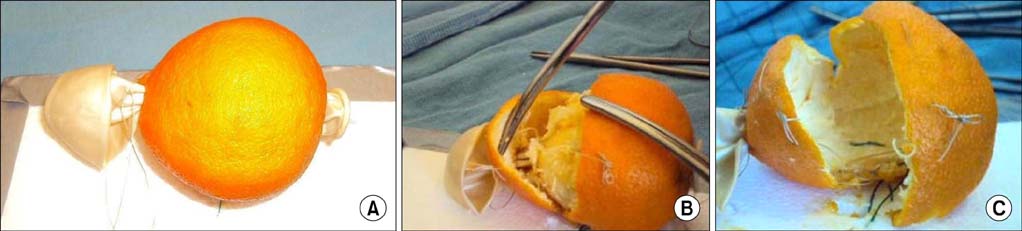
The RP model used a Foley catheter with ballistics gelatin in the balloon and mesh fabric (neurovascular bundles) and balloons (prostatic fascial layers) on either side for the practice of inter- and intrafascial techniques. The SP model required only a ripe clementine, for which the skin represented compressed normal prostate, the pulp represented benign tissue, and the pith mimicked fibrous adhesions. A modification with a balloon through the fruit center acted as a "urethra."
RESULTS
Both models were easily created and successfully represented the principles of anatomical nerve-sparing RP and SP. Both models were tested in workshops by urologists and residents of differing levels with positive feedback.
CONCLUSIONS
Low-fidelity models for prostate anatomy demonstration and surgical practice are feasible. They are inexpensive and simple to construct. Importantly, these models can be used for education on the practical aspects of nerve-sparing RP and SP. The models will require further validation as educational and competency tools, but as we move to an era in which human donors and animal experiments become less ethical and more difficult to complete, so too will low-fidelity models become more attractive.
Keyword
MeSH Terms
Figure
Reference
-
1. Lawrentschuk N, Fleshner N. An interactive multimedia approach to urological anatomy. BJU Int. 2010. 105:904–906.2. Lawrentschuk N, Lindner U, Fleshner N. Current textbooks and anatomy of the prostate--a case for an update. BJU Int. 2009. 103:1319–1322.3. Walsh PC. The discovery of the cavernous nerves and development of nerve sparing radical retropubic prostatectomy. J Urol. 2007. 177:1632–1635.4. Kourambas J, Angus DG, Hosking P, Chou ST. A histological study of Denonvilliers' fascia and its relationship to the neurovascular bundle. Br J Urol. 1998. 82:408–410.5. Costello AJ, Brooks M, Cole OJ. Anatomical studies of the neurovascular bundle and cavernosal nerves. BJU Int. 2004. 94:1071–1076.6. Grober ED, Roberts M, Shin EJ, Mahdi M, Bacal V. Intraoperative assessment of technical skills on live patients using economy of hand motion: establishing learning curves of surgical competence. Am J Surg. 2010. 199:81–85.7. Chipman JG, Schmitz CC. Using objective structured assessment of technical skills to evaluate a basic skills simulation curriculum for first-year surgical residents. J Am Coll Surg. 2009. 209:364–370.8. Xylinas E, Ploussard G, Salomon L, Paul A, Gillion N, Laet KD, et al. Intrafascial nerve-sparing radical prostatectomy with a laparoscopic robot-assisted extraperitoneal approach: early oncological and functional results. J Endourol. 2010. 24:577–582.9. Walker JB, Perkins E, Harkey HL. A novel simulation model for minimally invasive spine surgery. Neurosurgery. 2009. 65:6 Suppl. 188–195.10. Schöffl H, Froschauer SM, Dunst KM, Hager D, Kwasny O, Huemer GM. Strategies for the reduction of live animal use in microsurgical training and education. Altern Lab Anim. 2008. 36:153–160.11. Reed AB, Crafton C, Giglia JS, Hutto JD. Back to basics: use of fresh cadavers in vascular surgery training. Surgery. 2009. 146:757–762.12. Bach T, Geavlete B, Herrmann TR, Gross AJ. "Homemade" TURsimulator for less than $40 U.S.? The "Tupper" experience. J Endourol. 2009. 23:509–513.13. Jussila J. Preparing ballistic gelatine--review and proposal for a standard method. Forensic Sci Int. 2004. 141:91–98.14. Qayumi K. Surgical skills lab: a hub for competency training. J Invest Surg. 2010. 23:48–56.15. Scalese RJ, Obeso VT, Issenberg SB. Simulation technology for skills training and competency assessment in medical education. J Gen Intern Med. 2008. 23:Suppl 1. 46–49.16. Dahm P, Preminger GM, Scales CD Jr, Fesperman SF, Yeung LL, Cohen MS. Evidence-based medicine training in residency: a survey of urology programme directors. BJU Int. 2009. 103:290–293.17. Piechaud PT, Pansadoro A. Transfer of skills from the experimental model to the patients. Curr Urol Rep. 2006. 7:96–99.18. Davis JW, Kamat A, Munsell M, Pettaway C, Pisters L, Matin S. Initial experience of teaching robot-assisted radical prostatectomy to surgeons-in-training: can training be evaluated and standardized? BJU Int. 2009. Epub ahead of print.19. Rowan RL. A test to determine transurethral resection ability. Br J Urol. 1961. 33:323–325.20. Ooi J, Lawrentschuk N, Murphy DL. Training model for open or laparoscopic pyeloplasty. J Endourol. 2006. 20:149–152.21. Bartoletti R, Cai T, Tosoratti N, Amabile C, Crisci A, Tinacci G, et al. In vivo microwave-induced porcine kidney thermoablation: results and perspectives from a pilot study of a new probe. BJU Int. 2010. 106:1817–1821.22. McDougall EM, Kolla SB, Santos RT, Gan JM, Box GN, Louie MK, et al. Preliminary study of virtual reality and model simulation for learning laparoscopic suturing skills. J Urol. 2009. 182:1018–1025.23. Seixas-Mikelus SA, Kesavadas T, Srimathveeravalli G, Chandrasekhar R, Wilding GE, Guru KA. Face validation of a novel robotic surgical simulator. Urology. 2010. 76:357–360.24. Schout BM, Muijtjens AM, Hendrikx AJ, Ananias HJ, Dolmans VE, Scherpbier AJ, et al. Acquisition of flexible cystoscopy skills on a virtual reality simulator by experts and novices. BJU Int. 2010. 105:234–239.25. Sharma D, Shaban A, Riddell A, Kalsi V, Arya M, Grange P. Video-games station or minimally invasive skills training station? BJU Int. 2009. 104:159–160.26. Shane MD, Pettitt BJ, Morgenthal CB, Smith CD. Should surgical novices trade their retractors for joysticks? Videogame experience decreases the time needed to acquire surgical skills. Surg Endosc. 2008. 22:1294–1297.27. Wilson M, Coleman M, McGrath J. Developing basic hand-eye coordination skills for laparoscopic surgery using gaze training. BJU Int. 2010. 105:1356–1358.28. Sugand K, Abrahams P, Khurana A. The anatomy of anatomy: a review for its modernization. Anat Sci Educ. 2010. 3:83–93.29. Kim DK, Lee JW, Park SY, Kim YT, Park HY, Lee TY. Initial experience with robotic-assisted laparoscopic partial cystectomy in urachal diseases. Korean J Urol. 2010. 51:318–322.30. Yun HK, Kwon JB, Cho SR, Kim JS. Early experience with laparoscopic retropubic simple prostatectomy in patients with voluminous benign prostatic hyperplasia (BPH). Korean J Urol. 2010. 51:323–329.