Pediatr Gastroenterol Hepatol Nutr.
2013 Jun;16(2):116-122.
Clinical Factors Affecting Lipid Metabolism and Optimal Dose of Heparin in Preterm Infants on Parenteral Nutrition
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seoul, Korea. hryang@snubh.org
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea.
Abstract
- PURPOSE
Preterm infants on parenteral nutrition are at a relatively high risk for hypertriglyceridemia because they have immature lipoprotein lipase activity. The purpose of this study was to analyze the clinical factors affecting lipid metabolism in preterm infants receiving parenteral nutrition and to evaluate the influence of intravenous heparin on serum triglycerides to determine the adequate heparin dose to prevent hypertriglyceridemia in preterm infants.
METHODS
A single-center retrospective review was conducted among preterm infants receiving parenteral nutrition between January 2006 and February 2011. In 75 patients, 110 determinations were performed within 28 days postnatal age. Demographic and clinical data, including laboratory parameters, the dose and the duration of lipid administration, and the amount of intravenous heparin, were analyzed.
RESULTS
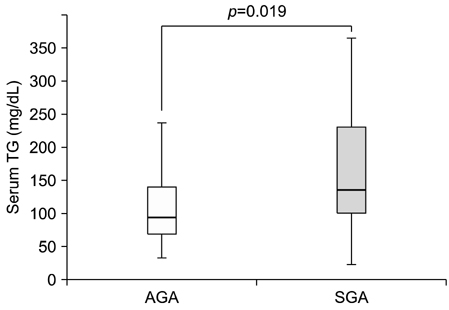
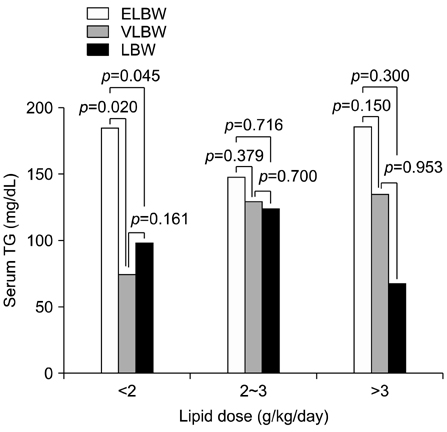
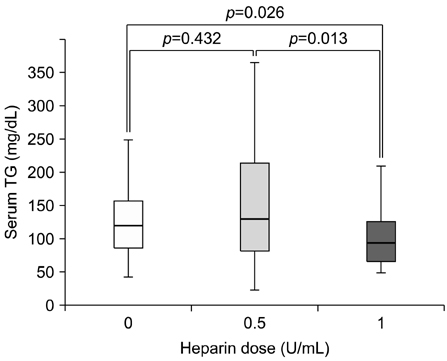
Serum triglycerides were higher in the small for gestational age (SGA) infants than in the appropriate for gestational age infants (185.5+/-134.9 mg/dL vs. 126.9+/-101.9 mg/dL, p=0.019). Birth weight, gestational age, and body weight were negatively correlated with serum triglyceride level (r=-0.289, p=0.002; r=-0.208, p=0.029; r=-0.287, p=0.002, respectively). The serum triglyceride level was statistically lower in preterm infants receiving 1 U/mL of heparin than in those receiving 0.5 U/mL heparin or no heparin.
CONCLUSION
Preterm infants receiving parenteral nutrition, particularly SGA and extremely low birth weight infants, tend to have hypertriglyceridemia. Thus, administration of 1 U/mL of heparin rather than 0.5 U/mL or none may be helpful to prevent hypertriglyceridemia in preterm infants.
MeSH Terms
Figure
Reference
-
1. Shennan AT, Bryan MH, Angel A. The effect of gestational age on intralipid tolerance in newborn infants. J Pediatr. 1977; 91:134–137.
Article2. Andrew G, Chan G, Schiff D. Lipid metabolism in the neonate. I. The effects of Intralipid infusion on plasma triglyceride and free fatty acid concentrations in the neonate. J Pediatr. 1976; 88:273–278.3. Adamkin DH, Gelke KN, Andrews BF. Fat emulsions and hypertriglyceridemia. JPEN J Parenter Enteral Nutr. 1984; 8:563–567.
Article4. Wang H, Eckel RH. Lipoprotein lipase: from gene to obesity. Am J Physiol Endocrinol Metab. 2009; 297:E271–E288.
Article5. Rovamo L, Nikkilä EA, Taskinen MR, Raivio KO. Postheparin plasma lipoprotein and hepatic lipases in preterm neonates. Pediatr Res. 1984; 18:1104–1107.
Article6. Simmer K, Rao SC. Early introduction of lipids to parenterally-fed preterm infants. Cochrane Database Syst Rev. 2005; (2):CD005256.
Article7. Yun ES, Park YH, Choi KH. Risk factors of non-alcoholic steatohepatitis in childhood obesity. Korean J Pediatr Gastroenterol Nutr. 2007; 10:179–184.
Article8. Hong YM, Kang YJ, Suh SJ. Correlation between High Blood Pressure and Lipid Profile in School Children. J Korean Pediatr Soc. 1995; 38:1645–1652.9. Rovamo LM, Nikkilä EA, Raivio KO. Lipoprotein lipase, hepatic lipase, and carnitine in premature infants. Arch Dis Child. 1988; 63:140–147.
Article10. Zhang L, Lookene A, Wu G, Olivecrona G. Calcium triggers folding of lipoprotein lipase into active dimers. J Biol Chem. 2005; 280:42580–42591.
Article11. Magkos F, Mittendorfer B. Gender differences in lipid metabolism and the effect of obesity. Obstet Gynecol Clin North Am. 2009; 36:245–265.
Article12. Drenckpohl D, McConnell C, Gaffney S, Niehaus M, Macwan KS. Randomized trial of very low birth weight infants receiving higher rates of infusion of intravenous fat emulsions during the first week of life. Pediatrics. 2008; 122:743–751.
Article13. Connelly PW. The role of hepatic lipase in lipoprotein metabolism. Clin Chim Acta. 1999; 286:243–255.
Article14. Neuger L, Vilaró S, Lopez-Iglesias C, Gupta J, Olivecrona T, Olivecrona G. Effects of heparin on the uptake of lipoprotein lipase in rat liver. BMC Physiol. 2004; 4:13.15. Shah PS, Ng E, Sinha AK. Heparin for prolonging peripheral intravenous catheter use in neonates. Cochrane Database Syst Rev. 2005; (4):CD002774.
Article16. Silvers KM, Darlow BA, Winterbourn CC. Pharmacologic levels of heparin do not destabilize neonatal parenteral nutrition. JPEN J Parenter Enteral Nutr. 1998; 22:311–314.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Parenteral Nutrition Support in Preterm Infants
- Selenium deficiency and supplementation in infants: a narrative review
- Early Effective Parenteral Nutrition for Preterm Infants
- The Effect of Parenteral Nutrition and Respiratory Distress Syndrome in the Early Neonatal Period on Bone Mineralization at the Time of Reaching 2 kg Body Weight in Premature Infants
- Enteral Feeding for Preterm Infants-Benefits and Risks