Korean J Urol.
2009 Nov;50(11):1133-1137.
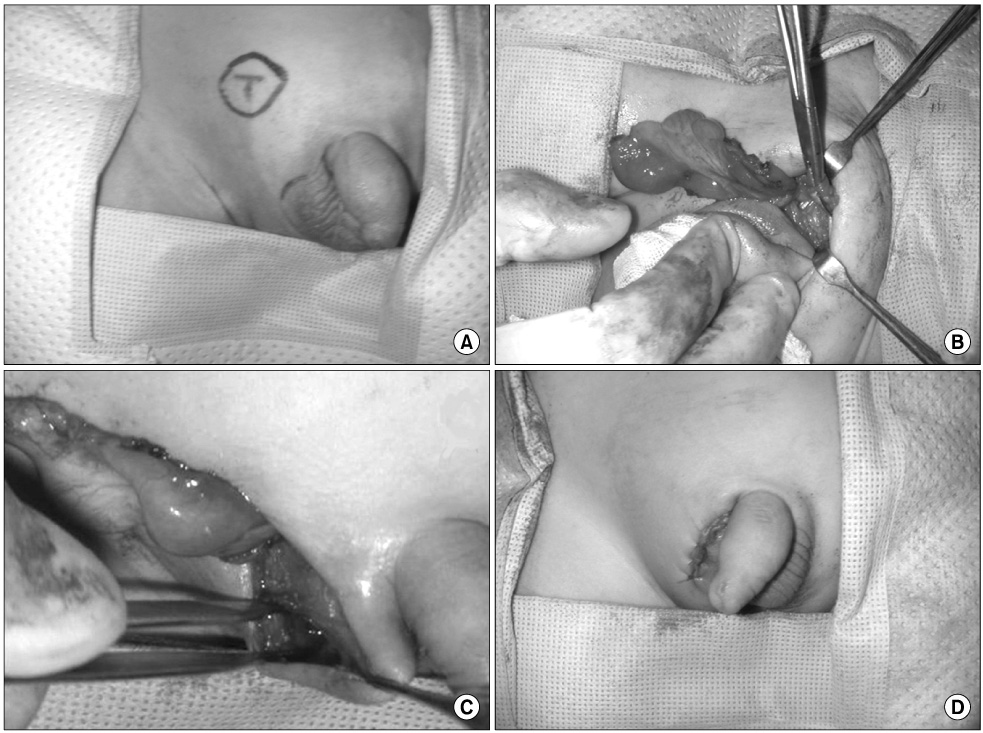
A Comparison between Single Scrotal Incision Orchiopexy and the Inguinal Approach in Patients with Palpable Undescended Testes Distal to the External Inguinal Ring
- Affiliations
-
- 1Department of Urology, The Catholic University of Korea College of Medicine, Seoul, Korea. gostraight@catholic.ac.kr
Abstract
- PURPOSE
Single scrotal incision orchiopexy is emerging as an alternative to the traditional inguinal approach. The purpose of this study was to compare the operative time, success rates, and complications of single scrotal incision orchiopexy with the traditional inguinal approach.
MATERIALS AND METHODS
We reviewed the charts of patients with palpable undescended testes treated with a single scrotal incision or inguinal orchiopexy from April 2004 to April 2008. The position of the testis was confirmed under general anesthesia before any incision. Retractile and ectopic testes were excluded. We compared preoperative and postoperative testicular position, operative time, prevalence of patent processus vaginalis, and complications between the two groups.
RESULTS
There were 43 patients who had palpable undescended testes below the external inguinal ring. A total of 57 orchiopexies were performed in 43 patients by either the single scrotal approach (group 1; n=25, mean age 3.12+/-1.99 years) or the inguinal approach (group 2; n=32, mean age 2.56+/-1.92 years). The average operative times for groups 1 and 2 were 39.76+/-7.66 and 53.31+/-6.33 minutes, respectively (p<0.05). Only 1 patient required conversion to an inguinal incision because of inappropriate mobilization. The complication rates were similar between the two groups. Testicular atrophy, hernia, or hydrocele formation did not occur during the follow-up period (4-41 months).
CONCLUSIONS
Single scrotal incision orchiopexy is an effective procedure in selected patients regardless of patency of the processus vaginalis. It has the advantages of a shorter operative time and a more cosmetically appealing result compared with the inguinal two-incision approach.
Keyword
MeSH Terms
Figure
Reference
-
1. Berkowitz GS, Lapinski RH, Dolgin SE, Gazella JG, Bodian CA, Holzman IR. Prevalence and natural history of cryptorchidism. Pediatrics. 1993. 92:44–49.2. Russinko PJ, Siddiq FM, Tackett LD, Caldamone AA. Prescrotal orchiopexy: an alternative surgical approach for the palpable undescended testis. J Urol. 2003. 170:2436–2438.3. Moul JW, Belman AB. A review of surgical treatment of undescended testes with emphasis on anatomical position. J Urol. 1988. 140:125–128.4. Bianchi A, Squire BR. Trans-scrotal orchidopexy: orchidopexy revised. Pediatr Surg Int. 1989. 4:189–192.5. Al-Mandil M, Khoury AE, El-Hout Y, Kogon M, Dave S, Farhat WA. Potential complications with the prescrotal approach for the palpable undescended testis? A comparison of single prescrotal incision to the traditional inguinal approach. J Urol. 2008. 180:686–689.6. Lais A, Ferro F. Trans-scrotal approach for surgical correction of cryptorchidism and congenital anomalies of the processus vaginalis. Eur Urol. 1996. 29:235–238.7. Bassel YS, Scherz HC, Kirsch AJ. Scrotal incision orchiopexy for undescended testes with or without a patent processus vaginalis. J Urol. 2007. 177:1516–1518.8. Caruso AP, Walsh RA, Wolach JW, Koyle MA. Single scrotal incision orchiopexy for the palpable undescended testicle. J Urol. 2000. 164:156–158.9. Koyle MA, Walsh R, Caruso A, Wilson E. Scrotal (Bianchi) approach to patent processus vaginalis in children. Tech Urol. 1999. 5:95–99.10. Hutcheson JC, Cooper CS, Snyder HM 3rd. The anatomical approach to inguinal orchiopexy. J Urol. 2000. 164:1702–1704.11. Dayanc M, Kibar Y, Tahmaz L, Yildirim I, Peker AF. Scrotal incision orchiopexy for undescended testis. Urology. 2004. 64:1216–1218.12. Handa R, Kale R, Harjai M, Minocha A. Single scrotal incision orchiopexy for palpable undescended testis. Asian J Surg. 2006. 29:25–27.13. Rajimwale A, Brant WO, Koyle MA. High scrotal (Bianchi) single-incision orchidopexy: a "tailored" approach to the palpable undescended testis. Pediatr Surg Int. 2004. 20:618–622.14. Clarnette TD, Rowe D, Hasthorpe S, Hutson JM. Incomplete disappearance of the processus vaginalis as a cause of ascending testis. J Urol. 1997. 157:1889–1891.15. Park E, Lee SD, Choi KW. The timing of surgery in unilateral inguinal cryptorchidism: In the aspect of histomorphological changes. Korean J Urol. 2004. 45:43–48.16. Lim HS, Kim HT, Moon KH. Five year follow-up testicular growth results after orchiopexy in palpable cryptorchid testis. Korean J Urol. 2008. 49:271–276.17. Lee JH, Han JJ, Song SY, Park KH. Histological changes of the cryptorchid testis according to the age. Korean J Urol. 2002. 43:631–637.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Single Scrotal Incision Orchiopexy for Children with Palpable Low-Lying Undescended Testis: Early Outcome of a Prospective Randomized Controlled Study
- A Comparative Study of Single Scrotal Incision Orchiopexy of Children with Palpable Low-Lying Undescended Testis with Traditional Inguinal Method
- Orchidopexy: a 10-year Clinical Experience
- Guideline for the Surgical Diagnosis and Treatment of Nonpalpable Testis Based on Experiences with Laparoscopic Procedure
- Clinical Observation on Undescended Testis