Nutr Res Pract.
2014 Feb;8(1):103-111.
Nutritional education for management of osteodystrophy (NEMO) trial: Design and patient characteristics, Lebanon
- Affiliations
-
- 1Department of Health Promotion, Maastricht University, 6200 MD Maastricht, Netherlands. kmirey@gmail.com
Abstract
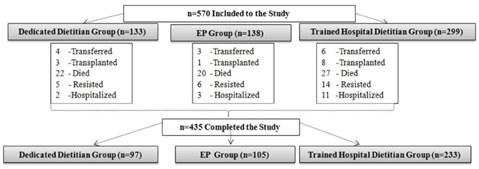
- This study aims to determine the effect of a trained dedicated dietitian on clinical outcomes among Lebanese hemodialysis (HD) patients: and thus demonstrate a viable developing country model. This paper describes the study protocol and baseline data. The study was a multicenter randomized controlled trial with parallel-group design involving 12 HD units: assigned to cluster A (n = 6) or B (n = 6). A total of 570 patients met the inclusion criteria. Patients in cluster A were randomly assigned as per dialysis shift to the following: Dedicated Dietitian (DD) (n = 133) and Existing Practice (EP) (n = 138) protocols. Cluster B patients (n = 299) received Trained Hospital Dietitian (THD) protocol. Dietitians of the DD and THD groups were trained by the research team on Kidney Disease Outcomes Quality Initiative nutrition guidelines. DD protocol included: individualized nutrition education for 2 hours/month/HD patient for 6 months focusing on renal osteodystrophy and using the Trans-theoretical theory for behavioral change. EP protocol included nutrition education given to patients by hospital dietitians who were blinded to the study. The THD protocol included nutrition education to patients given by hospital dietitian as per the training received but within hospital responsibilities, with no set educational protocol or tools. Baseline data revealed that 40% of patients were hyperphosphatemics (> 5.5 mg/dl) with low dietary adherence and knowledge of dietary P restriction in addition to inadequate daily protein intake (58.86%+/- 33.87% of needs) yet adequate dietary P intake (795.52 +/- 366.94 mg/day). Quality of life (QOL) ranged from 48-75% of full health. Baseline differences between the 3 groups revealed significant differences in serum P, malnutrition status, adherence to diet and P chelators and in 2 factors of the QOL: physical and social functioning. The data show room for improvement in the nutritional status of the patients. The NEMO trial may be able to demonstrate a better nutritional management of HD patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Lebanese National Kidney Registry (LB). Lebanese National Kidney Registry [Internet]. Lebanon: Lebanon Society of Nephrology and Hypertension;2012. cited 2014 Jan 15. Available from: http://kidneyregistrylb.com/pages/wp-content/uploads/2013/09/Upload-NKRCh319Sep13.pdf.2. Eknoyan G, Lameire N, Barsoum R, Eckardt KU, Levin A, Levin N, Locatelli F, MacLeod A, Vanholder R, Walker R, Wang H. The burden of kidney disease: improving global outcomes. Kidney Int. 2004; 66:1310–1314.
Article3. Mallat S, Hatoum A, Kabalan S, Elzein H, Abdallah A. 183 demographic and clinical profile of patients initiated on hemodialysis in lebanon. Am J Kidney Dis. 2011; 57:B62.
Article4. Central Intelligence Agency (US). The World Factbook [Internet]. Washington D.C.: Central Intelligence Agency;2012. cited 2014 Jan 15. Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/le.html.5. Denhaerynck K, Manhaeve D, Dobbels F, Garzoni D, Nolte C, De Geest S. Prevalence and consequences of nonadherence to hemodialysis regimens. Am J Crit Care. 2007; 16:222–235.
Article6. Lee SH, Molassiotis A. Dietary and fluid compliance in Chinese hemodialysis patients. Int J Nurs Stud. 2002; 39:695–704.
Article7. Karavetian M, Ghaddar S. Nutritional education for the management of osteodystrophy (nemo) in patients on haemodialysis: a randomised controlled trial. J Ren Care. 2013; 39:19–30.
Article8. Richard CJ. Self-care management in adults undergoing hemodialysis. Nephrol Nurs J. 2006; 33:387–394.9. American Dietetic Association's Evidence Analysis Library (US). Is MNT Provided by a Registered Dietitian for Chronic Kidney Disease (CKD) in Adults Effective? Chicago (IL): American Dietetic Association's Evidence Analysis Library;2010.10. Karavetian M, Elzein H, Hwalla N, de Vries N. Dietetic practices in hemodialysis units in lebanon and their conformity with KDOQI nutrition guidelines. Int J Health Nutr. 2013; 4:1–8.11. Gregory MC. Cost-effective dialysis for the developing world. Ethn Dis. 2009; 19:S1-65–S1-67.12. Griva K, Mooppil N, Seet P, Krishnan DS, James H, Newman SP. The NKF-NUS hemodialysis trial protocol - a randomized controlled trial to determine the effectiveness of a self management intervention for hemodialysis patients. BMC Nephrol. 2011; 12:4.
Article13. Prochaska JO. Decision making in the transtheoretical model of behavior change. Med Decis Making. 2008; 28:845–849.
Article14. Finckenor M, Byrd-Bredbenner C. Nutrition intervention group program based on preaction-stage-oriented change processes of the Transtheoretical Model promotes long-term reduction in dietary fat intake. J Am Diet Assoc. 2000; 100:335–342.
Article15. Mason J, Khunti K, Stone M, Farooqi A, Carr S. Educational interventions in kidney disease care: a systematic review of randomized trials. Am J Kidney Dis. 2008; 51:933–951.
Article16. Ford JC, Pope JF, Hunt AE, Gerald B. The effect of diet education on the laboratory values and knowledge of hemodialysis patients with hyperphosphatemia. J Ren Nutr. 2004; 14:36–44.
Article17. Hoelscher DM, Day RS, Kelder SH, Ward JL. Reproducibility and validity of the secondary level School-Based Nutrition Monitoring student questionnaire. J Am Diet Assoc. 2003; 103:186–194.
Article18. Welch JL. Hemodialysis patient beliefs by stage of fluid adherence. Res Nurs Health. 2001; 24:105–112.
Article19. Kalantar-Zadeh K, Kopple JD, Block G, Humphreys MH. A malnutrition-inflammation score is correlated with morbidity and mortality in maintenance hemodialysis patients. Am J Kidney Dis. 2001; 38:1251–1263.
Article20. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36).I. Conceptual framework and item selection. Med Care. 1992; 30:473–483.21. Sabbah I, Drouby N, Sabbah S, Retel-Rude N, Mercier M. Quality of life in rural and urban populations in Lebanon using SF-36 health survey. Health Qual Life Outcomes. 2003; 1:30.22. Shaw-Stuart NJ, Stuart A. The effect of an educational patient compliance program on serum phosphate levels in patients receiving hemodialysis. J Ren Nutr. 2000; 10:80–84.
Article23. Reddy V, Symes F, Sethi N, Scally AJ, Scott J, Mumtaz R, Stoves J. Dietitian-led education program to improve phosphate control in a single-center hemodialysis population. J Ren Nutr. 2009; 19:314–320.
Article24. Rambod M, Peyravi H, Shokrpour N, Sareban MT. Dietary and fluid adherence in Iranian hemodialysis patients. Health Care Manag (Frederick). 2010; 29:359–364.
Article25. Kugler C, Maeding I, Russell CL. Non-adherence in patients on chronic hemodialysis: an international comparison study. J Nephrol. 2011; 24:366–375.
Article26. Lam LW, Twinn SF, Chan SW. Self-reported adherence to a therapeutic regimen among patients undergoing continuous ambulatory peritoneal dialysis. J Adv Nurs. 2010; 66:763–773.
Article27. Kaveh K, Kimmel PL. Compliance in hemodialysis patients: multidimensional measures in search of a gold standard. Am J Kidney Dis. 2001; 37:244–266.
Article28. Muehrer RJ, Schatell D, Witten B, Gangnon R, Becker BN, Hofmann RM. Factors affecting employment at initiation of dialysis. Clin J Am Soc Nephrol. 2011; 6:489–496.
Article29. Ashurst Ide B, Dobbie H. A randomized controlled trial of an educational intervention to improve phosphate levels in hemodialysis patients. J Ren Nutr. 2003; 13:267–274.
Article30. Sun CY, Chang KC, Chen SH, Chang CT, Wu MS. Patient education: an efficient adjuvant therapy for hyperphosphatemia in hemodialysis patients. Ren Fail. 2008; 30:57–62.
Article31. Lim S, Gun NT. Secondary hyperparathyroidism and calcium phosphate control in a hemodialysis population. Acta Med Indones. 2007; 39:71–74.32. Qunibi WY. Consequences of hyperphosphatemia in patients with end-stage renal disease (ESRD). Kidney Int Suppl. 2004; S8–S12.
Article33. Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004; 15:2208–2218.
Article34. Mayne TJ, Benner D, Ricketts K, Burgess M, Wilson S, Poole L, Smyth M, Colson C, Krishnan M. Results of a pilot program to improve phosphorus outcomes in hemodialysis patients. J Ren Nutr. 2012; 22:472–479.
Article35. Cupisti A, Ferretti V, D'Alessandro C, Petrone I, Di Giorgio A, Meola M, Panichi V, Conti P, Lippi A, Caprioli R, Capitanini A. Nutritional knowledge in hemodialysis patients and nurses: focus on phosphorus. J Ren Nutr. 2012; 22:541–546.
Article36. Durose CL, Holdsworth M, Watson V, Przygrodzka F. Knowledge of dietary restrictions and the medical consequences of noncompliance by patients on hemodialysis are not predictive of dietary compliance. J Am Diet Assoc. 2004; 104:35–41.
Article37. Nerbass FB, Morais JG, dos Santos RG, Krüger TS, Koene TT, da Luz Filho HA. Adherence and knowledge about hyperphosphatemia treatment in hemodialysis patients with hyperphosphatemia. J Bras Nefrol. 2010; 32:149–155.38. Andrew NH, Engel B, Hart K, Passey C, Beaden S. Micronutrient intake in haemodialysis patients. J Hum Nutr Diet. 2008; 21:375–376.
Article39. Locatelli F, Fouque D, Heimburger O, Drüeke TB, Cannata-Andía JB, Hörl WH, Ritz E. Nutritional status in dialysis patients: a European consensus. Nephrol Dial Transplant. 2002; 17:563–572.
Article40. Morais AA, Silva MA, Faintuch J, Vidigal EJ, Costa RA, Lyrio DC, Trindade CR, Pitanga KK. Correlation of nutritional status and food intake in hemodialysis patients. Clinics (Sao Paulo). 2005; 60:185–192.
Article41. CKD mineral and bone disorder. In : McCann L, editor. Pocket Guide to Nutrition Assessment of the Patient with Chronic Kidney Disease. 4th ed. New York (NY): National Kidney Foundation;2009. p. 8.8–8.9.42. Mochari-Greenberger H, Terry MB, Mosca L. Does stage of change modify the effectiveness of an educational intervention to improve diet among family members of hospitalized cardiovascular disease patients? J Am Diet Assoc. 2010; 110:1027–1035.
Article43. Rambod M, Bross R, Zitterkoph J, Benner D, Pithia J, Colman S, Kovesdy CP, Kopple JD, Kalantar-Zadeh K. Association of Malnutrition-Inflammation Score with quality of life and mortality in hemodialysis patients: a 5-year prospective cohort study. Am J Kidney Dis. 2009; 53:298–309.
Article44. Tayyem RF, Mrayyan MT. Assessing the prevalence of malnutrition in chronic kidney disease patients in Jordan. J Ren Nutr. 2008; 18:202–209.
Article45. Kimmel PL, Emont SL, Newmann JM, Danko H, Moss AH. ESRD patient quality of life: symptoms, spiritual beliefs, psychosocial factors, and ethnicity. Am J Kidney Dis. 2003; 42:713–721.
Article46. Aghakhani N, Samadzadeh S, Mafi TM, Rahbar N. The impact of education on nutrition on the quality of life in patients on hemodialysis: a comparative study from teaching hospitals. Saudi J Kidney Dis Transpl. 2012; 23:26–30.
Article47. Covic A, Seica A, Gusbeth-Tatomir P, Gavrilovici O, Goldsmith DJ. Illness representations and quality of life scores in haemodialysis patients. Nephrol Dial Transplant. 2004; 19:2078–2083.
Article48. Han H, Burrowes JD, Houser R, Chung MC, Dwyer JT. What is the impact of nutritional status on health-related quality of life in hemodialysis patients? J Ren Nutr. 2012; 22:237–243.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coaching for Self-Management of Diabetes in Medical Nutrition Therapy
- Nutritional Intervention Process for a Patient with Kidney Transplantation: a Case Report
- Incontinentia Pigmenti in a Newborn with NEMO Mutation
- Epidural Hematoma after Minor Trauma on Patient with Biparietal Osteodystrophy
- Current status of nutritional screening in periodic health examination