Korean J Urol.
2008 Jul;49(7):598-603.
Long-term Follow up of Augmentation Ileocystoplasty with Goodwin's Ileal Cup Patched Bladder
- Affiliations
-
- 1Department of Urology, Yongdong Severance Hospital, Yonsei University Health System, Seoul, Korea. mahsy@yuhs.ac
Abstract
-
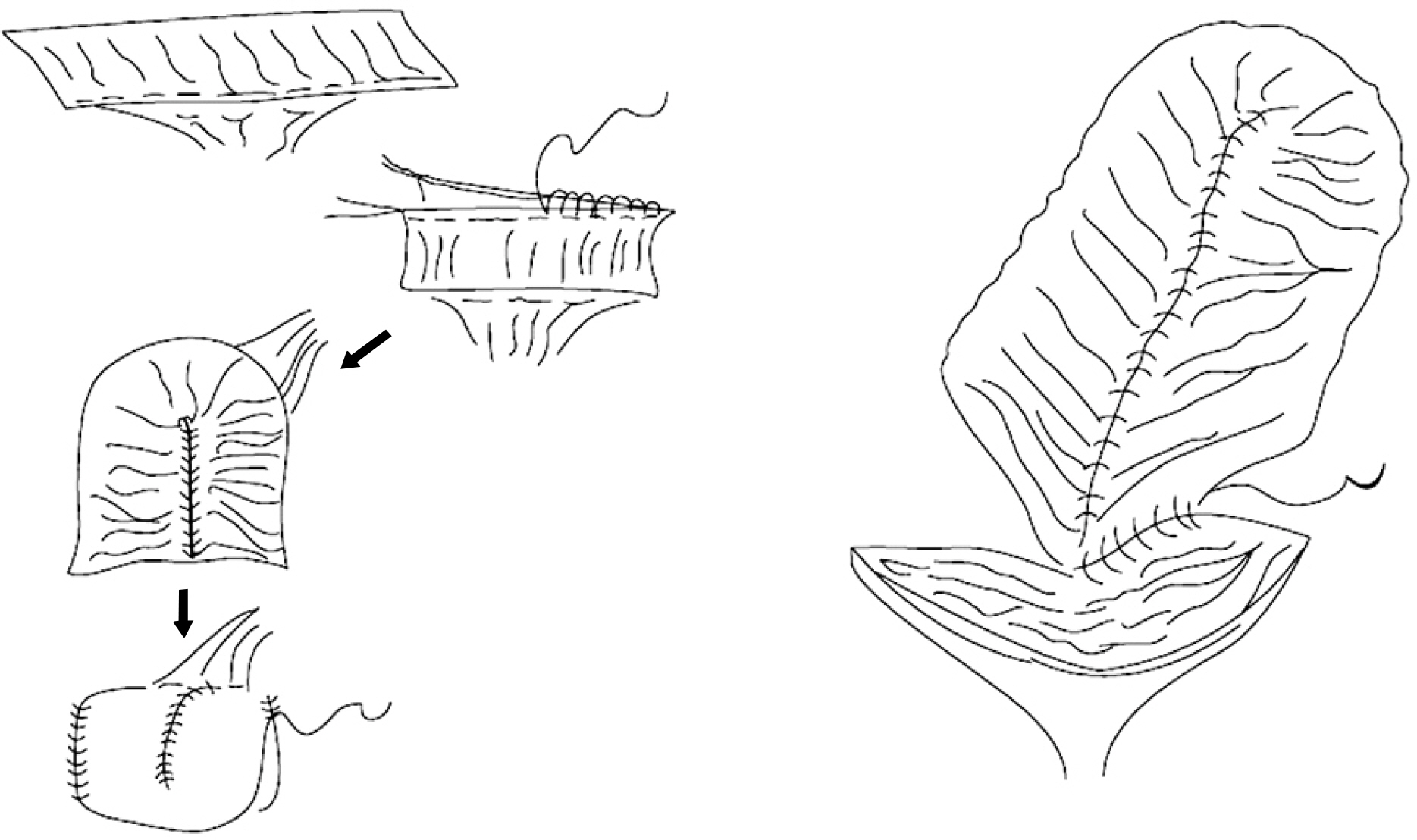
PURPOSE: We evaluated the long-term outcomes in patients undergoing augmentation ileocystoplasty with Goodwin(')s ileal cup patched bladder.
MATERIALS AND METHODS
This was a retrospective study of 72 consecutive patients who underwent augmentation ileocystoplasty because of decreased bladder capacity, vesico-ureteral reflux and urinary incontinence. The outcomes assessed included the continence status, bladder capacity, upper tract status, and significant post-operative complications.
RESULTS
The 72 patients studied(61 men and 11 women) were 12 to 62 years old(mean age 35.6). The follow up was 0.3 to 7.9 years(mean 5.4). The preoperative diagnoses were a neurogenic bladder from spinal cord injury in 54 patients, meningomyelocele in 5, pelvic trauma in 3, polymyelitis in 2, GU tuberculosis in 2, cerebrovascular diseases in 2, and disc rupture in 2. The bladder capacity was significantly increased from 168cc to 392cc postoperatively and the maximal bladder capacity was increased along with the decreased number of daily clean intermittent catheterizations. The most common complication related to surgery was a paralytic ileus. While most cases of unilateral reflux disappeared, bilateral or high grade reflux remained during the postoperative follow up period.
CONCLUSIONS
Bladder augmentation provided durable clinical and urodynamic improvement for patients with neurogenic and contracted bladders.
Keyword
MeSH Terms
Figure
Reference
-
1.Greenwell TJ., Venn SN., Mundy AR. Augmentation cystoplasty. BJU Int. 2001. 88:511–25.
Article2.Blaivas JG., Weiss JP., Desai P., Flisser AJ., Stember DS., Stahl PJ. Long-term followup of augmentation enterocystoplasty and continent diversion in patients with benign disease. J Urol. 2005. 173:1631–4.
Article3.Kurzrock EA., Baskin LS., Kogan BA. Gastrocystoplasty: long-term followup. J Urol. 1998. 160:2182–6.
Article4.Smith JJ 3rd., Swierzewski SJ 3rd. Augmentation cystoplasty. Urol Clin North Am. 1997. 24:745–54.
Article5.Chong CI., Yoon KH., Sung GT., Kwon HY., Yoon JH. An experience of augmentation gastrocystoplasty in the treatment of a child with spastic neurogenic bladder. Korean J Urol. 1995. 36:1128–34.6.Yang KM., Jeon HJ., Han SW. The clinical experience of the ureterocystoplasty in neurogenic bladder. Korean J Urol. 2005. 46:708–12.7.Landau EH., Jayanthi VR., Khoury AE., Churchill BM., Gilmour RF., Steckler RE, et al. Bladder augmentation: ureterocysto-plasty versus ileocystoplasty. J Urol. 1994. 152:716–9.
Article8.Leng WW., Blalock HJ., Fredriksson WH., English SF., McGuire EJ. Enterocystoplasty or detrusor myectomy? Comparison of indications and outcomes for bladder augmentation. J Urol. 1999. 161:758–63.
Article9.Goodwin WE., Winter CC., Barker WF. "Cup-patch" technique of ileocystoplasty for bladder enlargement or partial substitution. J Urol. 2002. 168:667–70.
Article10.Kim YB., Park WH., Shim HB. The long-term outcomes of augmentation cystoplasty in spinal cord injury patients. Korean J Urol. 2003. 44:529–33.11.Lee JS., Mah SY. The clinical experience of the bladder augmentation with Goodwin's ileal cup-patched bladder. Korean J Urol. 2003. 44:882–8.12.Cho MK., Song HC., Seo KS., Kim JS., Rim JS. An experience of spastic neurogenic bladder treated with augmentation cystoplasty and external urethral sphincterotomy. Korean J Urol. 1998. 39:195–9.13.Hendren WH., Hendren RB. Bladder augmentation: experience with 129 children and young adults. J Urol. 1990. 144:445–53.
Article14.Gough DC. Enterocystoplasty. BJU Int. 2001. 88:739–43.
Article15.Khoury JM., Timmons SL., Corbel L., Webster GD. Complications of enterocystoplasty. Urology. 1992. 40:9–14.
Article16.Quek ML., Ginsberg DA. Long-term urodynamics followup of bladder augmentation for neurogenic bladder. J Urol. 2003. 169:195–8.
Article17.Simforoosh N., Tabibi A., Basiri A., Noorbala MH., Danesh AD., Ijadi A. Is ureteral reimplantation necessary during augmentation cystoplasty in patients with neurogenic bladder and vesicoureteral reflux? J Urol. 2002. 168:1439–41.
Article18.Hayashi Y., Kato Y., Okazaki T., Lane GJ., Kobayashi H., Yamataka A. The effectiveness of ureteric reimplantation during bladder augmentation for high-grade vesicoureteric reflux in patients with neurogenic bladder: long-term outcome. J Pediatr Surg. 2007. 42:1998–2001.
Article19.Guven A., Onal B., Kogan BA. Spontaneous bladder perforations following augmentation cystoplasty in children. Nat Clin Pract Urol. 2006. 3:584–5.
Article20.Kim JH., Park EC., Lee SE. The long-term results of augmentation cystoplasty in contracted bladder. Korean J Urol. 2001. 42:59–64.21.Flood HD., Malhotra SJ., O'Connell HE., Ritchey MJ., Bloom DA., McGuire EJ. Long-term results and complications using augmentation cystoplasty in reconstructive urology. Neurourol Urodyn. 1995. 14:297–309.
Article22.Atala A. Future trends in bladder reconstructive surgery. Semin Pediatr Surg. 2002. 11:134–42.
Article23.Byun SS., Chung YS., Lee SS., Lee HN., Lee JY., Lee JY. Augmentation cystoplasty using hydroxapatite/chitosan composite sheet seeded with autologous muscle-derived stem cells. Korean J Urol. 2007. 48:433–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Experience of the Bladder Augmentation with Goodwin's Ileal Cup-patched Bladder
- The experience of the bladder augmentation and substitution with Studer's ileal cup-patched bladder
- Functional Analysis of Anti-Refluxing Augmentation Cystoplasty
- Clinical Observation and Follow-up Study on Ileocystoplasty
- Experimental Study on Ileocystoplasty: 2. Production of Collateral Blood Supply to the Ileac Segment After Ileocystoplasty