Korean J Urol.
2008 Dec;49(12):1081-1086.
Relationship between Acute Urinary Retention and Intraprostatic Inflammation in Benign Prostatic Hyperplasia
- Affiliations
-
- 1Department of Urology, Keimyung University School of Medicine, Daegu, Korea. cikim@dsmc.or.kr
- 2Department of Pathology, Keimyung University School of Medicine, Daegu, Korea.
Abstract
-
PURPOSE: Acute or chronic prostatic inflammation exists to varying degrees in surgical specimens of prostates, extirpated for the treatment of benign prostatic hyperplasia(BPH). We investigated the relationship between acute urinary retention(AUR) and intraprostatic inflammation.
MATERIALS AND METHODS
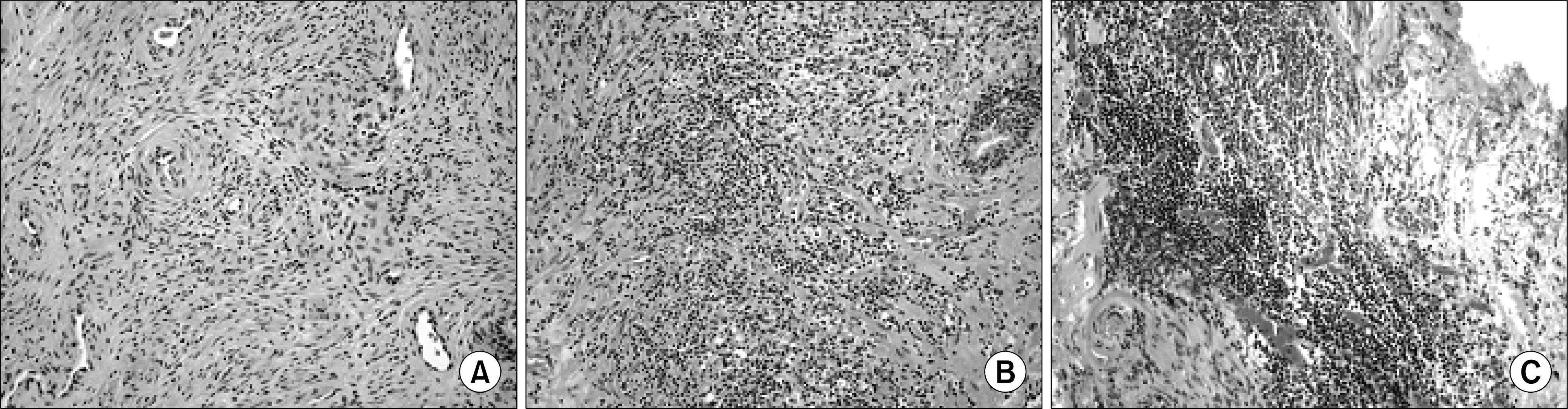
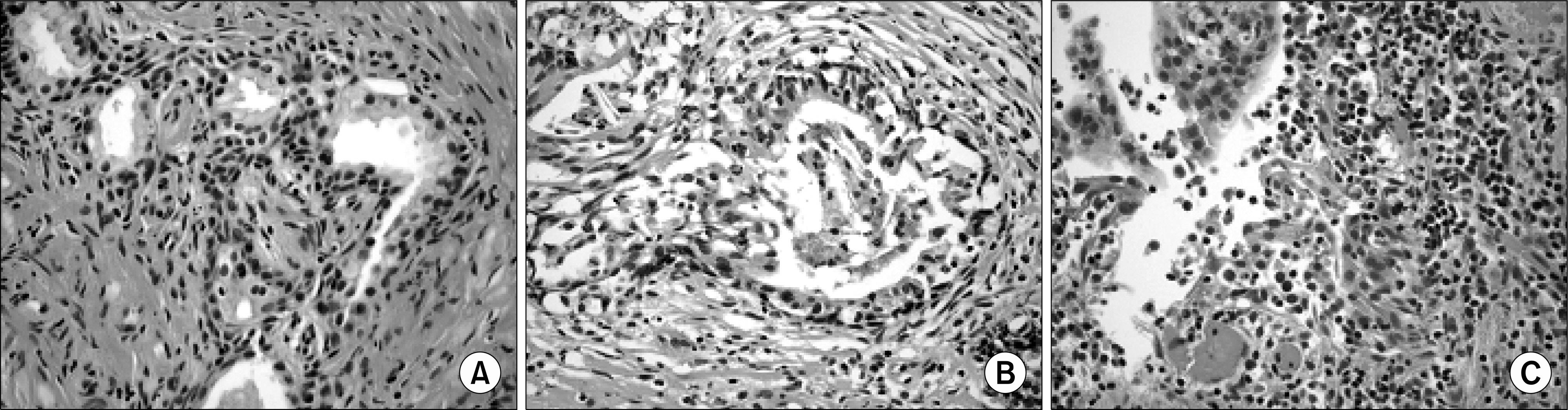
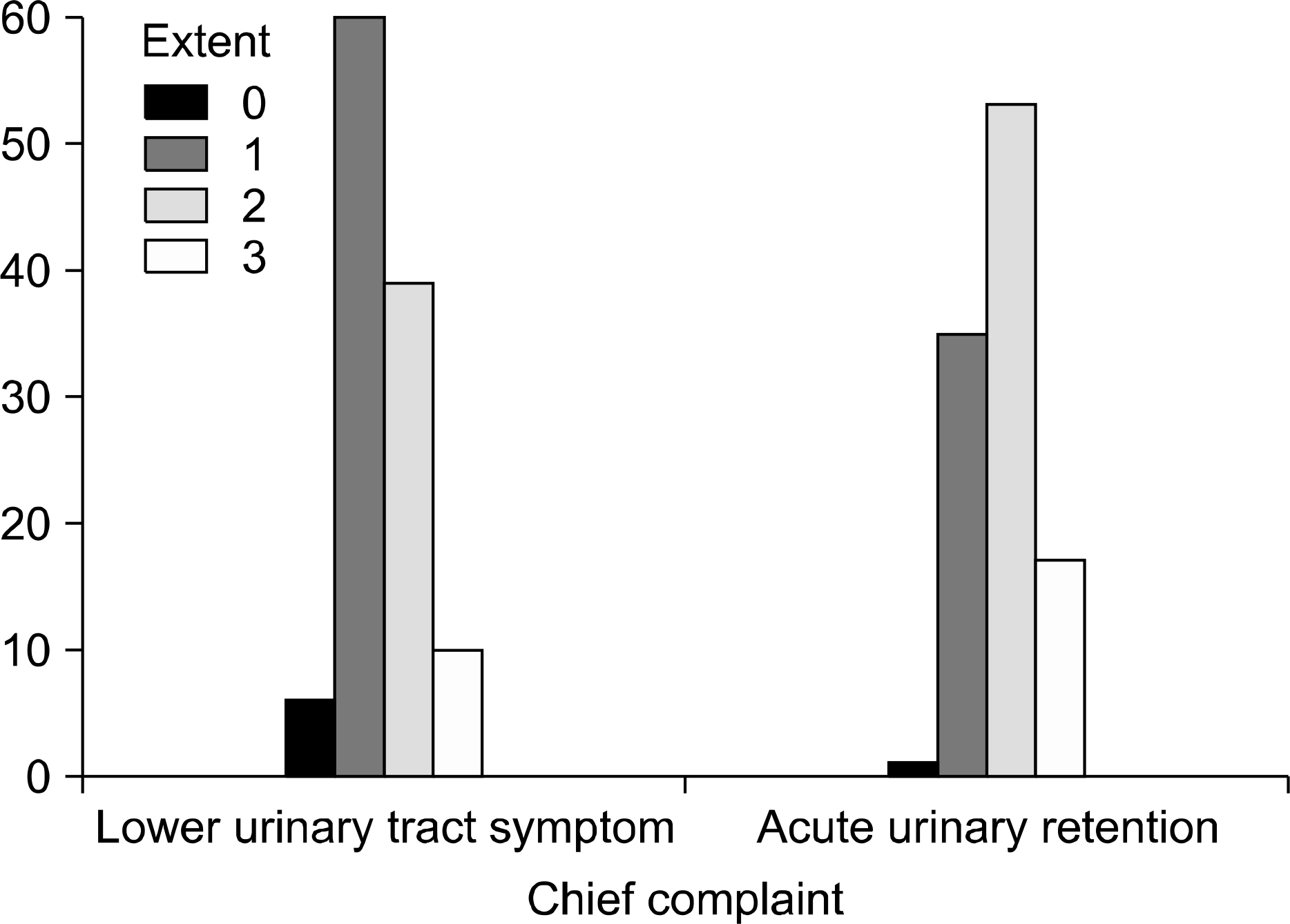
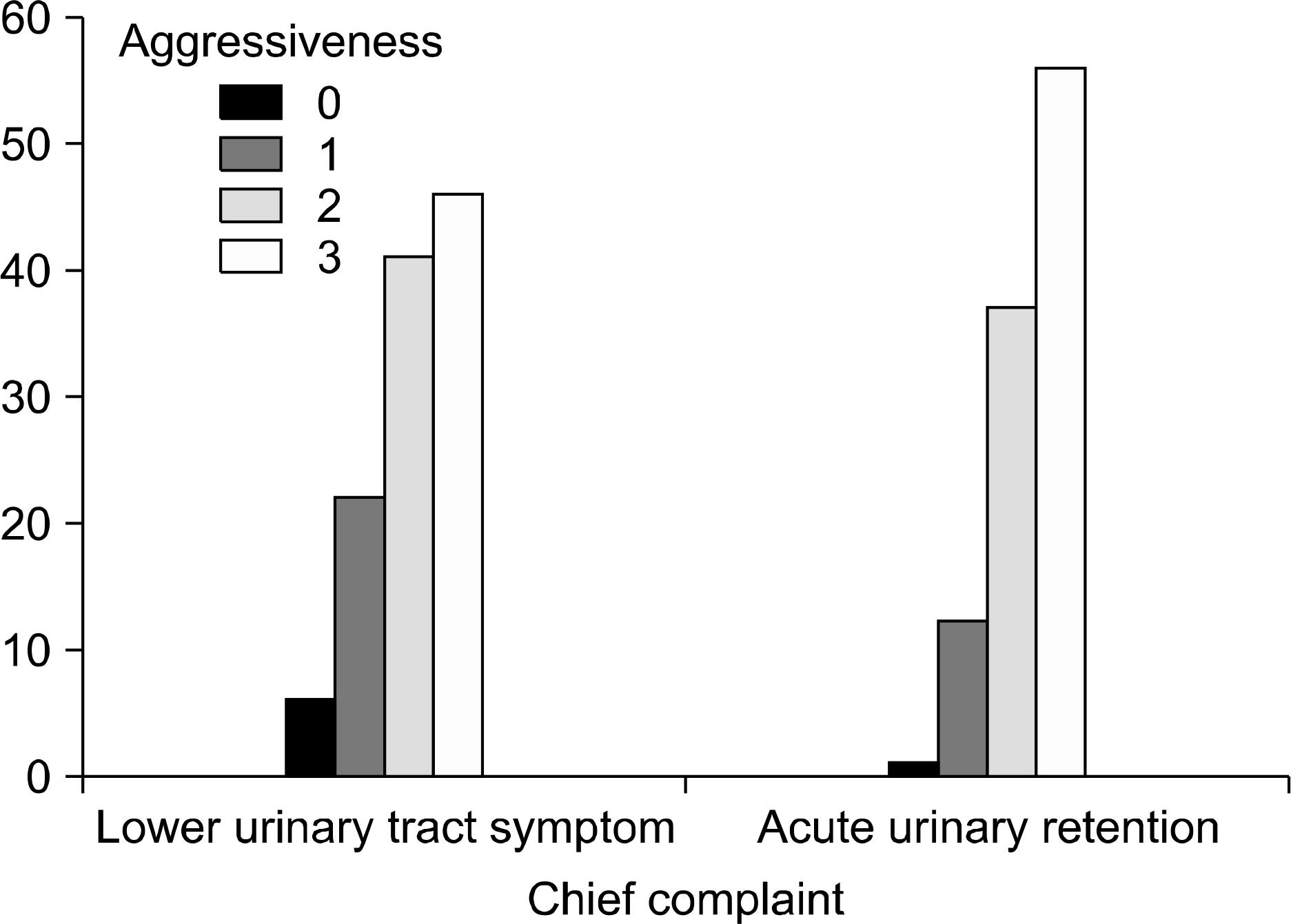
Between January 1997 and December 2006, 221 patients underwent transurethral resection of the prostate(TURP) for the treatment of BPH. The patients were divided into 2 groups based on the indication for surgery; an AUR group and a lower urinary tract symptoms (LUTS) group. The area of acute inflammation, the extent, and the aggressiveness of chronic inflammation were classified into four grades. The grades of inflammation, prostate volume, age, serum prostate-specific antigen(PSA), and prior medical treatment were compared between the two groups. All specimens were reviewed by one pathologist.
RESULTS
The AUR group consisted of 106(47.9%) patients, and the LUTS group consisted of 115(52.1%) patients. There were no statistical differences between the two groups with respect to the mean values of the age, prostate size, and severity of chronic inflammation. There was a significant relationship between AUR and the areas of acute inflammation, and the extent of chronic inflammation(p=0.014 and p=0.003, respectively). The aggressiveness of chronic inflammation had no relationship with AUR (p=0.062). The serum PSA level was higher in the AUR group than the LUTS group(11.5 vs. 5.3ng/ml, respectively).
CONCLUSIONS
The association for AUR with acute and chronic inflammation was stronger than that which existed with prostate size. Thus intraprostatic inflammation is an important risk factor in AUR.
MeSH Terms
Figure
Reference
-
References
1. Emberton M, Anson K. Acute urinary retention in men: an age old problem. BMJ. 1999; 318:921–5.2. Shah T, Palit V, Biyani S, Elmasry Y, Puri R, Flannigan GM. Randomised, placebo controlled, double blind study of alfuzosin SR in patients undergoing trial without catheter following acute urinary retention. Eur Urol. 2002; 42:329–32.
Article3. Kefi A, Koseoglu H, Celebi I, Yorukoglu K, Esen A. Relation between acute urinary retention, chronic prostatic inflammation and accompanying elevated prostate-specific antigen. Scand J Urol Nephrol. 2006; 40:155–60.
Article4. Tuncel A, Uzun B, Eruyar T, Karabulut E, Seckin S, Atan A. Do prostatic infarction, prostatic inflammation and prostate morphology play a role in acute urinary retention? Eur Urol. 2005; 48:277–83.
Article5. Mishra VC, Allen DJ, Nicolaou C, Sharif H, Hudd C, Karim OM, et al. Does intraprostatic inflammation have a role in the pathogenesis and progression of benign prostatic hyperplasia? BJU Int. 2007; 100:327–31.
Article6. Kim MJ, Lee JG, Cheon J. The factors that influence the success rate of treatment without using a catheter for the management of acute urinary retention: comparison of in-and-out catheterization and Foley indwelling catheterization. Korean J Urol. 2008; 49:337–42.
Article7. Chang HS, Park CH, Kim CI. Transitional zone volume: a predictor of acute urinary retention in patients with benign prostatic hyperplasia. Korean J Urol. 2005; 46:259–63.8. Lee SJ, Kim YT, Lee TY, Woo YN. Analysis of risk factors for acute urinary retention after non-urogenital surgery. Korean J Urol. 2007; 48:1277–84.
Article9. Irani J, Levillain P, Goujon JM, Bon D, Dore B, Aubert J. Inflammation in benign prostatic hyperplasia: correlation with prostate specific antigen value. J Urol. 1997; 157:1301–3.
Article10. Delongchamps NB, de la Roza G, Chandan V, Jones R, Sunheimer R, Threatte G, et al. Evaluation of prostatitis in autopsied prostates – Is chronic inflammation more associated with benign prostatic hyperplasia or cancer? J Urol. 2008; 179:1736–40.11. Jacobsen SJ, Jacobson DJ, Girman CJ, Roberts RO, Rhodes T, Guess HA, et al. Natural history of prostatism: risk factors for acute urinary retention. J Urol. 1997; 158:481–7.
Article12. Kurita Y, Masuda H, Terada H, Suzuki K, Fujita K. Transition zone index as a risk factor for acute urinary retention in benign prostatic hyperplasia. Urology. 1998; 51:595–600.
Article13. Kim JH, Kim HG, Park WH. The predictors of acute urinary retention in patients with benign prostatic hyperplasia. Korean J Urol. 2002; 43:949–55.14. Fowler FJ Jr, Wennberg JE, Timothy RP, Barry MJ, Mulley AG Jr, Hanley D. Symptom status and quality of life following prostatectomy. JAMA. 1988; 259:3018–22.
Article15. Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989; 141:243–7.16. Roehrborn CG, McConnell JD, Lieber M, Kaplan S, Geller J, Malek GH, et al. Serum prostate-specific antigen concentration is a powerful predictor of acute urinary retention and need for surgery in men with clinical benign prostatic hyperplasia. Urology. 1999; 53:473–80.
Article17. Kim CI, Chang HS, Kim BK, Park CH. Long-term results of medical treatment in benign prostatic hyperplasia. Urology. 2006; 68:1015–9.
Article18. Lynch TH. Doxazosin and finasteride alone or in combination: the PREDICT study. BJU Int. 2003; 91:591–2.
Article19. McConnell JD, Roehrborn CG, Bautista OM, Andriole GL Jr, Dixon CM, Kusek JW, et al. The longterm effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003; 349:2387–98.
Article20. Di Silverio F, Gentile V, De Matteis A, Mariotti G, Giuseppe V, Luigi PA, et al. Distribution of inflammation, pre-malignant lesions, incidental carcinoma in histologically confirmed benign prostatic hyperplasia: a retrospective analysis. Eur Urol. 2003; 43:164–75.
Article21. Roberts RO, Lieber MM, Rhodes T, Girman CJ, Bostwick DG, Jacobsen SJ. Prevalence of a physician-assigned diagnosis of prostatitis: the Olmsted County Study of Urinary Symptoms and Health Status Among Men. Urology. 1998; 51:578–84.
Article22. Roberts RO, Jacobson DJ, Girman CJ, Rhodes T, Lieber MM, Jacobsen SJ. Prevalence of prostatitis-like symptoms in a community based cohort of older men. J Urol. 2002; 168:2467–71.
Article23. Roehrborn CG, Kaplan SA, Noble WD, Slawin KM, McVary KT, Kusek JW. The impact of acute or chronic inflammation in baseline biopsy on the risk of clinical progression of BPH. Results from the MTOPS study. J Urol. 2005; 173(Suppl):346. abstract 1277.24. Isaacs JT, Coffey DS. Etiology and disease process of benign prostatic hyperplasia. Prostate. 1989; 2(Suppl):33–50.
Article25. Nickel JC, Downey J, Young I, Boag S. Asymptomatic inflammation and/or infection in benign prostatic hyperplasia. BJU Int. 1999; 84:976–81.
Article26. Collins MM, Meigs JB, Barry MJ, Walker Corkery E, Giovannucci E, Kawachi I. Prevalence and correlates of prostatitis in the health professionals follow-up study cohort. J Urol. 2002; 167:1363–6.
Article27. Kramer G, Marberger M. Could inflammation be a key component in the progression of benign prostatic hyperplasia? Curr Opin Urol. 2006; 16:25–9.
Article28. Andriole G, Bostwick D, Brawley O, Gomella L, Margerger M, Tindall D, et al. Chemoprevention of prostate cancer in men at high risk: rationale and design of the reduction by dutasteride of prostate cancer events (REDUCE) trial. J Urol. 2004; 172:1314–7.
Article29. Nickel JC. Inflammation and benign prostatic hyperplasia. Urol Clin North Am. 2008; 35:109–15.
Article30. Minnery CH, Getzenberg RH, Robert H. Benign prostatic hyperplasia cell line viability and modulation of JM-27 by doxazosin and ibuprofen. J Urol. 2005; 174:375–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Insertion of intraprostatic spiral(urospiral@) in high risk patients with benign prostatic hyperplasia
- Significance of Intraprostatic Inflammation in Patients with Lower Urinary Tract Symptoms Suggestive of Benign Prostatic Hyperplasia
- The recovery of the destusor muscle function in acute urinary retention patients due to benign prostatic hyperplasia
- Clinical Observation for Complications of Non-Surgical Treatment of Benign Prostatic Hyperplasia
- The Effect of Chronic Prostatic Inflammation on Acute Urinary Retention in the Setting of Benign Prostatic Hyperplasia