Korean J Urol.
2009 Aug;50(8):791-796. 10.4111/kju.2009.50.8.791.
Significance of Intraprostatic Inflammation in Patients with Lower Urinary Tract Symptoms Suggestive of Benign Prostatic Hyperplasia
- Affiliations
-
- 1Department of Urology, Keimyung University School of Medicine, Daegu, Korea. cikim@dsmc.or.kr
- 2Department of Pathology, Keimyung University School of Medicine, Daegu, Korea.
- KMID: 1780484
- DOI: http://doi.org/10.4111/kju.2009.50.8.791
Abstract
- PURPOSE
Histological evidence of intraprostatic inflammation is a common finding of transrectal ultrasonography (TRUS)-guided needle biopsy of the prostate in patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia (BPH). The aim of this study was to evaluate the relationship between intraprostatic inflammation and lower urinary tract symptoms depending on the severity of intraprostatic inflammation. MATERIALS AND METHODS: Between January 2002 and December 2006, 141 BPH patients with prostate-specific antigen (PSA) of 4.0-10.0 ng/ml underwent TRUS-guided biopsy of the prostate. The extent and aggressiveness of intraprostatic inflammation were classified into 4 grades. The relationship between the grades of extent and aggressiveness of inflammation and the International Prostate Symptom Score (IPSS) was evaluated. The IPSS was evaluated according to voiding and storage symptom scores. RESULTS: Mean storage symptom scores were increased by grade of the extent of intraprostatic inflammation (grade 0, 6.3; grade 1, 10.1; grade 2, 11.0; and grade 3, 11.3) (p<0.001). The aggressiveness of intraprostatic inflammation also showed increasing storage symptom scores with grade (grade 0, 6.3; grade 1, 10.2; grade 2, 10.9; and grade 3, 11.6) (p<0.001). Voiding symptom scores had no relationship with extent or aggressiveness of intraprostatic inflammation (p=0.942 and p=0.449, respectively). CONCLUSIONS: BPH patients with intraprostatic inflammation complained of more severe storage symptoms than did patients without inflammation. Therefore, if storage symptoms are severe, we might consider medical treatment for intraprostatic inflammation in BPH patients.
Keyword
MeSH Terms
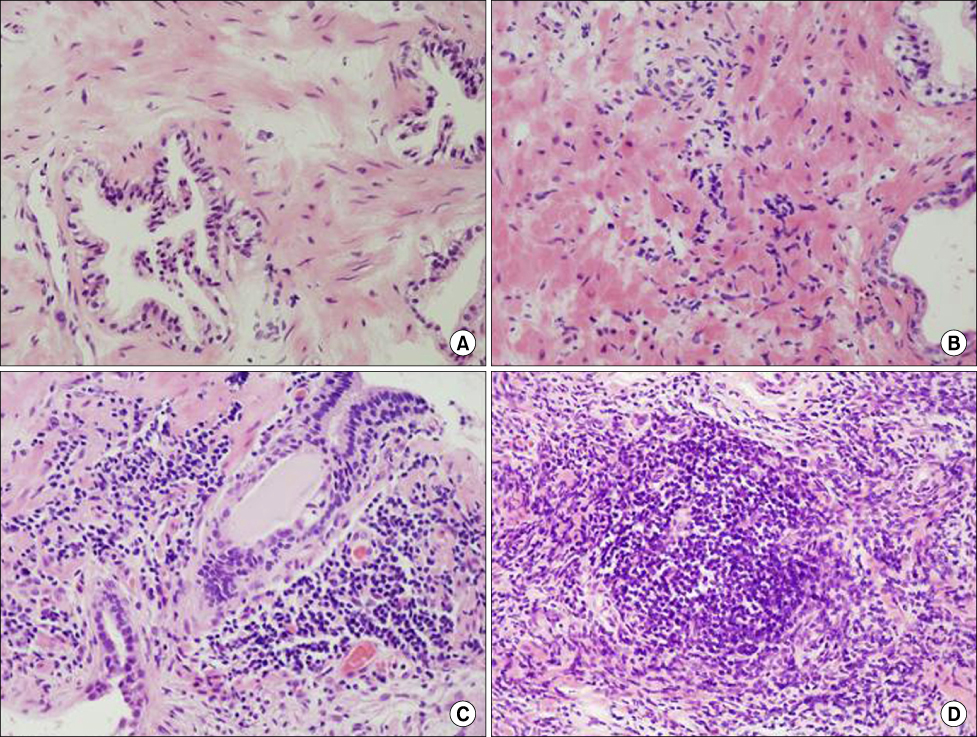
Figure
Reference
-
1. Verhamme KM, Dieleman JP, Bleumink GS, Van der Lei J, Sturkenboom MC, Artibani W, et al. Incidence and prevalence of lower urinary tract symptoms suggestive of benign prostatic hyperplasia in primary care-the Triumph project. Eur Urol. 2002. 42:323–328.2. Verhamme KM, Dieleman JP, Bleumink GS, Bosch JL, Stricker BH, Sturkenboom MC. Treatment strategies, patterns of drug use and treatment discontinuation in men with LUTS suggestive of benign prostatic hyperplasia: the Triumph project. Eur Urol. 2003. 44:539–545.3. Chung TG, Chung J, Lee MS, Ahn H. Prevalence of benign prostatic hyperplasia in Jeong-Eup area: community-based study. Korean J Urol. 1999. 40:52–58.4. Collins MM, Stafford RS, O'Leary MP, Barry MJ. How common is prostatitis? A national survey of physician visits. J Urol. 1998. 159:1224–1224.5. Roberts RO, Lieber MM, Rhodes T, Girman CJ, Bostwick DG, Jacobsen SJ. Prevalence of a physician-assigned diagnosis of prostatitis: the Olmsted county study of urinary symptoms and health status among men. Urology. 1998. 51:578–584.6. Woo YN. Prostatitis. Korean J Urol. 1994. 35:575–585.7. Roberts RO, Jacobson DJ, Girman CJ, Rhodes T, Lieber MM, Jacobsen SJ. Prevalence of prostatitis-like symptoms in a community based cohort of older men. J Urol. 2002. 168:2467–2471.8. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999. 282:236–237.9. Nickel JC, Downey J, Young I, Boag S. Asymptomatic inflammation and/or infection in benign prostatic hyperplasia. BJU Int. 1999. 84:976–981.10. Roehrborn CG, Kaplan SA, Noble WD, Lucia MS, Slawin KM, McVary KT, et al. The impact of acute or chronic inflammation in baseline biopsy on the risk of clinical progression of BPH: results from the MTOPS study. J Urol. 2005. 173:Suppl. 346. abstract 1277.11. Mishra VC, Allen DJ, Nicolaou C, Sharif H, Hudd C, Karim OM, et al. Does intraprostatic inflammation have a role in the pathogenesis and progression of benign prostatic hyperplasia? BJU Int. 2007. 100:327–331.12. Irani J, Levillain P, Goujon JM, Bon D, Dore B, Aubert J. Inflammation in benign prostatic hyperplasia: correlation with prostate specific antigen value. J Urol. 1997. 157:1301–1303.13. Kohnen PW, Drach GW. Patterns of inflammation in prostatic hyperplasia: a histologic and bacteriologic study. J Urol. 1979. 121:755–760.14. Nickel JC. Prostatic inflammation in benign prostatic hyperplasia-the third component? Can J Urol. 1994. 1:1–4.15. Odunjo EO, Elebute EA. Chronic prostatitis in benign prostatic hyperplasia. Br J Urol. 1971. 43:333–337.16. McNeal JE. Regional morphology and pathology of the prostate. Am J Clin Pathol. 1968. 49:347–357.17. Maksem JA, Johenning PW, Galang CF. Prostatitis and aspiration biopsy cytology of prostate. Urology. 1988. 32:263–268.18. Lee SY, Park YY. Clinical characteristics of the associated histopathological findings in benign prostatic hyperplasia. Korean J Urol. 1991. 32:915–920.19. Nickel JC, Roehrborn CG, O'Leary MP, Bostwick DG, Somerville MC, Rittmaster RS. The relationship between prostate inflammation and lower urinary tract symptoms: examination of baseline data from the REDUCE trial. J Urol. 2007. 177:Suppl. 34. abstract 98.20. Okada K, Kojima M, Naya Y, Kamoi K, Yokoyama K, Takamatsu T, et al. Correlation of histological inflammation in needle biopsy specimens with serum prostate-specific antigen levels in men with negative biopsy for prostate cancer. Urology. 2000. 55:892–898.21. Kramer G, Marberger M. Could inflammation be a key component in the progression of benign prostatic hyperplasia? Curr Opin Urol. 2006. 16:25–29.22. Emberton M, Elhilali M, Matzkin H, Harving N, van Moorselaar J, Hartung R, et al. Symptom deterioration during treatment and history of AUR are the strongest predictors for AUR and BPH-related surgery in men with LUTS treated with alfuzosin 10 mg once daily. Urology. 2005. 66:316–322.23. Kaplan SA, Te AE, Pressler LB, Olsson CA. Transition zone index as a method of assessing benign prostatic hyperplasia: correlation with symptoms, urine flow and detrusor pressure. J Urol. 1995. 154:1764–1769.24. McConnell JD, Roehrborn CG, Bautista OM, Andriole GL Jr, Dixon CM, Kusek JW, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003. 349:2387–2398.25. Di Silverio F, Bosman C, Salvatori M, Albanesi L, Proietti Pannunzi L, Ciccariello M, et al. Combination therapy with rofecoxib and finasteride in the treatment of men with lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH). Eur Urol. 2005. 47:72–78.26. Merendino RA, Salvo F, Saija A, Di Pasquale G, Tomaino A, Minciullo PL, et al. Malondialdehyde in benign prostate hypertrophy: a useful marker? Mediators Inflamm. 2003. 12:127–128.27. Rohrmann S, De Marzo AM, Smit E, Giovannucci E, Platz EA. Serum C-reactive protein concentration and lower urinary tract symptoms in older men in the Third National Health and Nutrition Examination Survey (NHANES III). Prostate. 2005. 62:27–33.28. Castro P, Xia C, Gomez L, Lamb DJ, Ittmann M. Interleukin-8 expression is increased in senescent prostatic epithelial cells and promotes the development of benign prostatic hyperplasia. Prostate. 2004. 60:153–159.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between Acute Urinary Retention and Intraprostatic Inflammation in Benign Prostatic Hyperplasia
- Current Trend of the Primary Treatment in Lower Urinary Tract Symptom/Benign Prostatic Hyperplasia
- Insertion of intraprostatic spiral(urospiral@) in high risk patients with benign prostatic hyperplasia
- Initial experience of 5 cases of intraprostatic spiral(PROSTAKA(TH))
- A Study on Physiological Index, Anxiety and Depression by the Severity of Lower Urinary Tract Symptoms in Patients with Benign Prostatic Hyperplasia