Ann Rehabil Med.
2016 Apr;40(2):197-205. 10.5535/arm.2016.40.2.197.
Usefulness of Submental Ultrasonographic Evaluation for Dysphagia Patients
- Affiliations
-
- 1Department of Rehabilitation Medicine, Bundang Jesaeng General Hospital, Seongnam, Korea. rhsrhs2u@gmail.com
- KMID: 2309917
- DOI: http://doi.org/10.5535/arm.2016.40.2.197
Abstract
OBJECTIVE
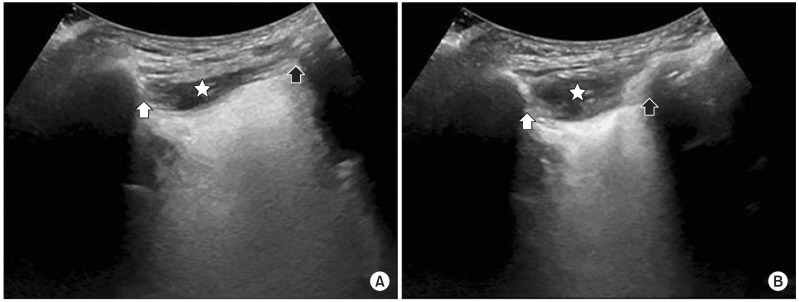
To investigate the usefulness of ultrasonographic measurement of hyoid bone movement during swallowing.
METHODS
Fifty-two patients who had swallowing dysfunction were enrolled in this study. When a patient swallowed 5 mL of water while maintaining an upright sitting position, hyoid bone movement during swallowing was measured with ultrasonography. Recorded images were analyzed to measure the maximum change in hyoid bone displacement. Mandible was used as reference point to calculate hyoid bone displacement. The farthest distance from resting position and the nearest distance during swallowing were measured and their differences were recorded. Participants also underwent videofluoroscopic swallowing study (VFSS). Based on penetration-aspiration scale (PAS), they were grouped to non-aspirators (PAS 1), penetrators (PAS 2-5), or aspirators (PAS 6-8). Measured hyoid bone displacements by submental ultrasonography were compared among groups.
RESULTS
The mean hyoid bone displacement in non-aspirators group (n=21, 15.9±2.7 mm) was significantly (p<0.05) greater than that in penetrators group (n=20, 11.5±2.8 mm) or aspirators group (n=11, 8.0±1.0 mm). Hyoid bone displacement below 13.5 mm as a cutoff point for detecting penetration or aspiration had a sensitivity and specificity of 83.9% and 81.0%, respectively.
CONCLUSION
Submental ultrasonographic evaluation was well correlated with PAS measured by VFSS. Therefore, submental ultrasonographic evaluation could be a useful screening tool for dysphagic patients.
MeSH Terms
Figure
Reference
-
1. Ishida R, Palmer JB, Hiiemae KM. Hyoid motion during swallowing: factors affecting forward and upward displacement. Dysphagia. 2002; 17:262–272. PMID: 12355141.
Article2. Logemann JA, Kahrilas PJ, Cheng J, Pauloski BR, Gibbons PJ, Rademaker AW, et al. Closure mechanisms of laryngeal vestibule during swallow. Am J Physiol. 1992; 262(2 Pt 1):G338–G344. PMID: 1539666.
Article3. Martino R, Pron G, Diamant N. Screening for oropharyngeal dysphagia in stroke: insufficient evidence for guidelines. Dysphagia. 2000; 15:19–30. PMID: 10594255.
Article4. Yabunaka K, Sanada H, Sanada S, Konishi H, Hashimoto T, Yatake H, et al. Sonographic assessment of hyoid bone movement during swallowing: a study of normal adults with advancing age. Radiol Phys Technol. 2011; 4:73–77. PMID: 20945118.
Article5. Hsiao MY, Chang YC, Chen WS, Chang HY, Wang TG. Application of ultrasonography in assessing oropharyngeal dysphagia in stroke patients. Ultrasound Med Biol. 2012; 38:1522–1528. PMID: 22698507.
Article6. Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005; 86:1516–1520. PMID: 16084801.
Article7. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–98. PMID: 8721066.
Article8. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–682. PMID: 11346847.
Article9. Elmståhl S, Bülow M, Ekberg O, Petersson M, Tegner H. Treatment of dysphagia improves nutritional conditions in stroke patients. Dysphagia. 1999; 14:61–66. PMID: 10028034.
Article10. Poertner LC, Coleman RF. Swallowing therapy in adults. Otolaryngol Clin North Am. 1998; 31:561–579. PMID: 9628950.
Article11. Dodds WJ, Logemann JA, Stewart ET. Radiologic assessment of abnormal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol. 1990; 154:965–974. PMID: 2108570.
Article12. DePippo KL, Holas MA, Reding MJ. The Burke dysphagia screening test: validation of its use in patients with stroke. Arch Phys Med Rehabil. 1994; 75:1284–1286. PMID: 7993165.
Article13. Yoon K, Kim SB, Lee KW, Park SH. Clinical utility of the bedside swallowing evaluations for dysphagia. J Korean Acad Rehabil Med. 2003; 27:489–493.14. Shawker TH, Sonies B, Stone M, Baum BJ. Real-time ultrasound visualization of tongue movement during swallowing. J Clin Ultrasound. 1983; 11:485–490. PMID: 6417184.
Article15. Kellen PM, Becker DL, Reinhardt JM, Van Daele DJ. Computer-assisted assessment of hyoid bone motion from videofluoroscopic swallow studies. Dysphagia. 2010; 25:298–306. PMID: 19856024.
Article16. Dengel G, Robbins J, Rosenbek JC. Image processing in swallowing and speech research. Dysphagia. 1991; 6:30–39. PMID: 1884636.
Article17. Logemann JA, Kahrilas PJ, Begelman J, Dodds WJ, Pauloski BR. Interactive computer program for biomechanical analysis of videoradiographic studies of swallowing. AJR Am J Roentgenol. 1989; 153:277–280. PMID: 2750613.
Article18. Braddom RL, Chan L, Harrast HA, Kowalske KJ, Matthews DJ, Ragnarsson KT, et al. Physical medicine and rehabilitation. 4th ed. Philadelphia: Saunders;2011. p. 581–600.19. Yokoyama M, Mitomi N, Tetsuka K, Tayama N, Niimi S. Role of laryngeal movement and effect of aging on swallowing pressure in the pharynx and upper esophageal sphincter. Laryngoscope. 2000; 110(3 Pt 1):434–439. PMID: 10718434.
Article20. Steele CM, Bailey GL, Chau T, Molfenter SM, Oshalla M, Waito AA, et al. The relationship between hyoid and laryngeal displacement and swallowing impairment. Clin Otolaryngol. 2011; 36:30–36. PMID: 21414151.
Article21. Eisenhuber E, Schima W, Schober E, Pokieser P, Stadler A, Scharitzer M, et al. Videofluoroscopic assessment of patients with dysphagia: pharyngeal retention is a predictive factor for aspiration. AJR Am J Roentgenol. 2002; 178:393–398. PMID: 11804901.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound Utilization in the Diagnosis and Management of Dysphagia
- Changes in Hyolaryngeal Movement and Swallowing Function After Neuromuscular Electrical Stimulation in Patients With Dysphagia
- The Usefulness of Flexible Endoscopic Evaluation of Swallowing in Head and Neck Cancer Patients
- Effects of Neuromuscular Electrical Stimulation on the Swallowing Function in a Child - A Case Report
- Evaluation of safety and usefulness of submental intubation in panfacial trauma surgery