Korean J Androl.
2012 Apr;30(1):40-44. 10.5534/kja.2012.30.1.40.
Impact of Nocturia on Abnormal Daytime Sleepiness in Men with Lower Urinary Tract Symptoms/Benign Prostate Hyperplasia
- Affiliations
-
- 1Department of Urology, Soonchunhyang University School of Medicine, Seoul, Korea. yssong@hosp.sch.ac.kr
- 2Medical Research Institute, Chung-Ang University School of Medicine, Seoul, Korea.
- 3Hankuk Academy of Foreign Studies, Yongin, Korea.
- KMID: 2298807
- DOI: http://doi.org/10.5534/kja.2012.30.1.40
Abstract
- PURPOSE
Nocturia is one of the most bothersome lower urinary tract symptoms (LUTS). The aim of the present study is to determine whether severe-nocturia have impact on the abnormal daytime sleepiness in men with LUTS/benign prostate hyperplasia (BPH).
MATERIALS AND METHODS
Severe-nocturia was classified as twice or more per night. A total of 85 men met the criteria and constituted the study cohort. The patients had a detailed clinical evaluation, including a complete history, physical examination, urine analysis, urine culture, a digital rectal examination, serum prostate-specific antigen (PSA) level, prostate volume by transrectal ultrasonography, uroflowmetry and postvoid residual urine volume. LUTS and symptom-specific quality of life (QoL) were assessed using the IPSS. Patients were asked to complete an Epworth Sleepiness Scale questionnaire for daytime sleepiness.
RESULTS
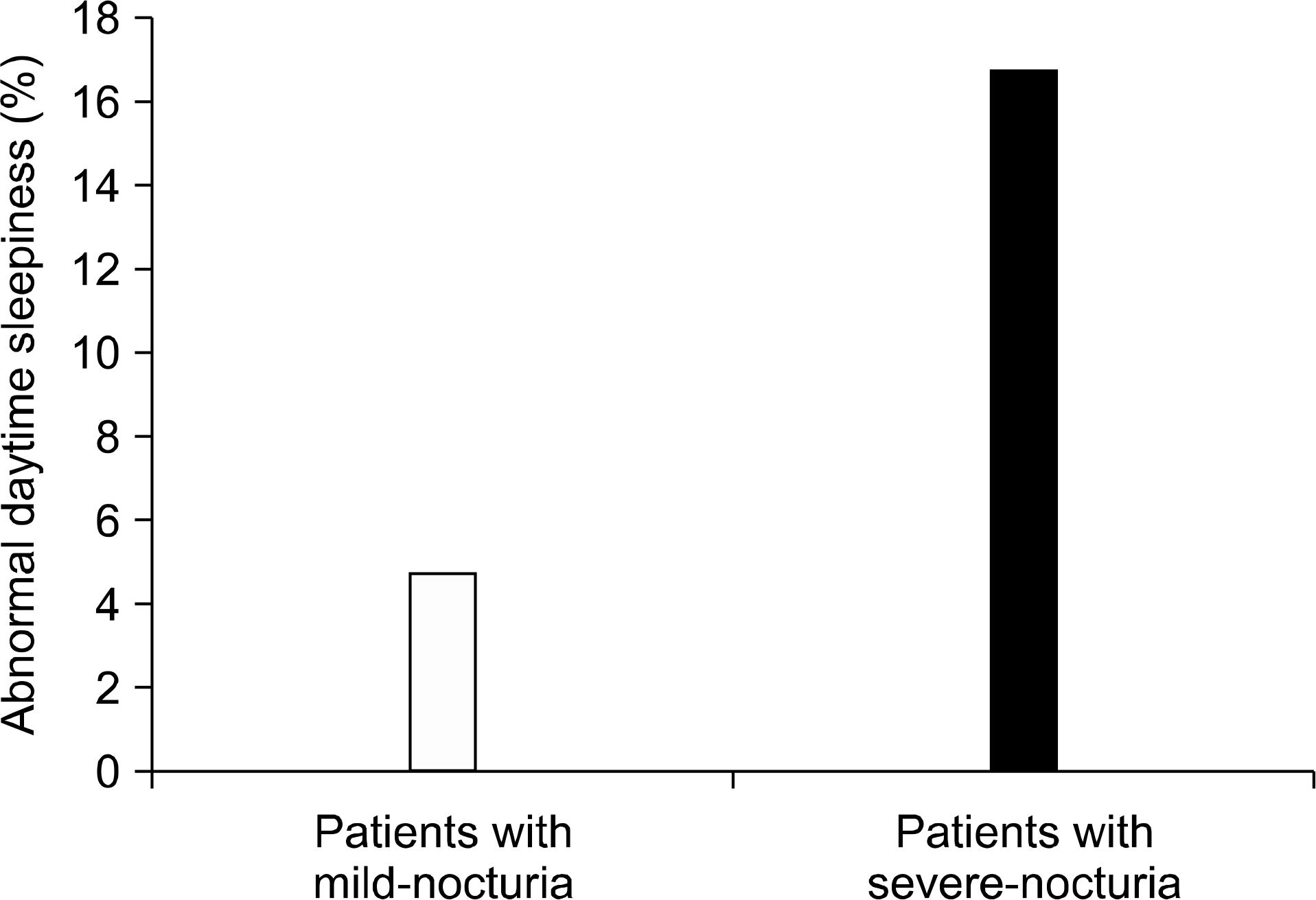
43 patients had less than one, 42 patients had more than two episodes of nocturia. There was no significant difference of age, total prostate volume, PSA levels between patients with mild-nocturia and severe-nocturia. There was no significant difference of maximum flow rate (Qmax), voided volume and postvoid residual urine volume (PVR) between patients with mild-nocturia and severe-nocturia. There was significant decrease of total International Prostate Symptom Score (IPSS) scores and QoL index in patients with severe-nocturia compared in patients with mild-nocturia. The number of patients with abnormal daytime sleepiness in mild-nocturia and severe-nocturia were 4.7% (2/43), 16.7% (7/42), respectively (p<0.05). Regression coefficiency between percent of nocturia and total score of daytime sleepiness was significant (p<0.05) and regression coefficient (R) was 0.29.
CONCLUSIONS
Our results indicate that severe-nocturia had impact on the abnormal daytime sleepiness in patients with LUTS.
MeSH Terms
Figure
Reference
-
1). Yoshimura K, Ohara H, Ichioka K, Terada N, Matsui Y, Terai A, et al. Nocturia and benign prostatic hyperplasia. Urology. 2003; 61:786–90.
Article2). Asplund R, Aberg H. Health of the elderly with regard to sleep and nocturnal micturition. Scand J Prim Health Care. 1992; 10:98–104.
Article3). Shim JB, Lee SH, Kim H. A study of minimal change in nocturia affecting quality of life. Korean J Urol. 2009; 50:241–5.
Article4). Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991; 14:540–5.
Article5). Johns MW. Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the epworth sleepiness scale: failure of the MSLT as a gold standard. J Sleep Res. 2000; 9:5–11.
Article6). Johns MW. Sleep propensity varies with behaviour and the situation in which it is measured: the concept of somnificity. J Sleep Res. 2002; 11:61–7.
Article7). Johns M. Rethinking the assessment of sleepiness. Sleep Med Rev. 1998; 2:3–15.
Article8). Chen NH, Johns MW, Li HY, Chu CC, Liang SC, Shu YH, et al. Validation of a Chinese version of the Epworth sleepiness scale. Qual Life Res. 2002; 11:817–21.9). Gander PH, Marshall NS, Harris R, Reid P. The Epworth Sleepiness Scale: influence of age, ethnicity, and socioeconomic deprivation. Epworth Sleepiness scores of adults in New Zealand. Sleep. 2005; 28:249–53.
Article10). Chervin RD, Aldrich MS, Pickett R, Guilleminault C. Comparison of the results of the Epworth Sleepiness Scale and the Multiple Sleep Latency Test. J Psychosom Res. 1997; 42:145–55.
Article11). Olson LG, Cole MF, Ambrogetti A. Correlations among Epworth Sleepiness Scale scores, multiple sleep latency tests and psychological symptoms. J Sleep Res. 1998; 7:248–53.
Article12). Mitler MM, Doghramji K, Shapiro C. The maintenance of wakefulness test: normative data by age. J Psychosom Res. 2000; 49:363–5.13). Gottlieb DJ, Whitney CW, Bonekat WH, Iber C, James GD, Lebowitz M, et al. Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study. Am J Respir Crit Care Med. 1999; 159:502–7.14). Kingshott RN, Engleman HM, Deary IJ, Douglas NJ. Does arousal frequency predict daytime function? Eur Respir J. 1998; 12:1264–70.
Article15). Chervin RD. The multiple sleep latency test and Epworth sleepiness scale in the assessment of daytime sleepiness. J Sleep Res. 2000; 9:399–401.
Article16). Chervin RD, Aldrich MS. The Epworth Sleepiness Scale may not reflect objective measures of sleepiness or sleep apnea. Neurology. 1999:52:125–31.
Article17). Broman JE, Lundh LG, Hetta J. Insufficient sleep in the general population. Neurophysiol Clin. 1996; 26:30–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nocturia is the Lower Urinary Tract Symptom With Greatest Impact on Quality of Life of Men From a Community Setting
- Strong Impact of Nocturia on Sleep Quality in Patients with Lower Urinary Tract Symptoms
- The Urinary Tract Microbiome in Male Genitourinary Diseases: Focusing on Benign Prostate Hyperplasia and Lower Urinary Tract Symptoms
- Pathophysiology of Male Lower Urinary Tract Symptoms
- The Relationship between Benign Prostate Hyperplasia and Erectile Dysfunction: What is Reality?