Korean J Urol.
2006 Nov;47(11):1172-1177. 10.4111/kju.2006.47.11.1172.
CyberKnife for the Treatment of Nonmetastatic Prostate Cancer: Preliminary Results
- Affiliations
-
- 1Departments of Urology and 1Radiation Oncology, Korea Cancer Center Hospital, Seoul, Korea.
- KMID: 2294275
- DOI: http://doi.org/10.4111/kju.2006.47.11.1172
Abstract
- Purpose
Herein is reported our initial experience of the CyberKnife to show its safety and feasibility as a treatment modality for non-metastatic prostate cancer.
Materials and Methods
Twenty patients, with biopsy-proven prostate cancers, were recruited into a phase I clinical trial using the CyberKnife. The distribution of clinical risks, as assessed using the ASTRO criteria, was as follows: low (4), intermediate (5) and high (11). The mean age and follow up of the patients were 71.4 years and 15 months, respectively. The patients received 7.5-9Gy of radiation in a single fraction for 4-5 days. The total radiation dose to the prostate was 34-37.5Gy, which approximates to 86.4Gy in 2Gy fractions. The rectal and bladder acute toxicities were graded using the criteria of the Radiation Therapy Oncology Group (RTOG). The results of acute toxicities were compared to those of the historical control, which had been treated with conventional four field box techniques (received median dose 70.2Gy). The prostate-specific antigen (PSA)- based short-term efficacy was described.
Results
The acute rectal toxicity scores were 0, 1 and 2 in 13, 5, and 2 patients, respectively. The acute bladder toxicity scores were 0, 1 and 2 in 16, 3 and 1 patient, respectively. No grade 3 or 4 acute toxicity was noted. These figures contrast sharply with those found for the historical control. All toxicities spontaneously subsided within 3 months after treatment. Continuous PSA reduction was noted in all patients, and no PSA failure was noted during the follow up period.
Conclusions
Our data show the feasibility of the CyberKnife in terms of its efficacy and acute toxicity. Moreover, the capability of using a hypo-fractionation schedule lead to marked improvement in patient convenience, with substantial resource savings.
Keyword
MeSH Terms
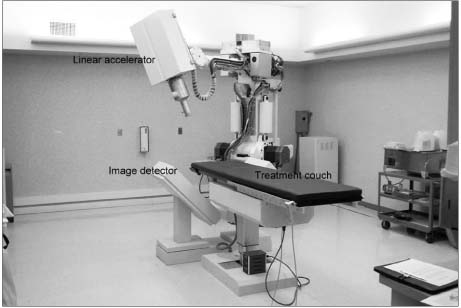
Figure
Cited by 1 articles
-
CyberKnifeTM for the Treatment of Non-Metastatic Prostate Cancer
Seung Joon Lee, Kanghyon Song, Jong Wook Park, Myung Cheol Gil, Moon Ki Jo
Korean J Urol. 2009;50(8):744-750. doi: 10.4111/kju.2009.50.8.744.
Reference
-
1. Horwitz EM, Hanlon AL, Pinover WH, Anderson PR, Hanks GE. Defining the optimal radiation dese with three dimensional conformal radiation therapy for patients with nonmetastatic prostate carcinoma by using recursive partitioning techniuques. Cancer. 2001. 92:1281–1287.2. Pollack A, Zagars G, Smith LG, Lee JJ, von Eschenbach AC, Antolak JA, et al. Preliminary results of a randomized radiotherapy dose-escalation study comparing 70Gy with 78Gy for prostate cancer. J Clin Oncol. 2000. 18:3904–3911.3. Zelefsy MJ, Leibel SA, Gaudin PB, Kutcher GJ, Fleshner NE, Venkatramen ES, et al. Dose escalation with three-dimensional conformal therapy affects the outcome in prostate cancer. Int J Radiat Oncol Biol Phys. 1998. 41:491–500.4. Brenner DJ. Toward optimal external-beam fractionation for prostate cancer. Int J Radiat Oncol Biol Phys. 2000. 48:315–316.5. Brenner DJ, Hall EJ. Fractionation and protraction for radiotherapy of prostate carcinoma. Int J Radiat Oncol Biol Phys. 1999. 43:1095–1101.6. Brenner DJ, Martinez AA, Edmundson GK, Mitchell C, Thames HD, Armour EP. Direct evidence that prostate tumors show high sensitivity to fractionation (low alpha/beta ratio), similar to late-responding normal tissue. Int J Radiat Oncol Biol Phys. 2002. 52:6–13.7. Fowler J, Chappell R, Ritter M. Is α/β for prostate really low? Int J Radiat Oncol Biol Phys. 2001. 50:1021–1033.8. King CR, Fowler JF. A simple analytic derivation suggests that prostate cancer α/β ration is low. Int J Radiat Oncol Biol Phys. 2001. 51:213–214.9. Kupelian PA, Reddy CA, Klein EA, Willoughby TR. Short-course intensity-modulated radiotherapy (70Gy at 2.5Gy per fraction) for localized prostate cancer: preliminary results on late toxicity and quality of life. Int J Radiat Oncol Biol Phys. 2001. 51:988–993.10. Lloyd-Davis RW, Collins CD, Swan AV. Carcinoma of prostate treated by radical external beam radiotherapy using hypofractionation: 22 years experience (1962-1984). Urology. 1990. 36:107–111.11. Martinez AA, Kestin LL, Stromberg JS, Gonzalez JA, Wallace M, Gustafson GS, et al. Interim report of image-guided conformal high-dose-rate brachytherapy for patients with unfavorable prostate cancer: the William Beaumont phase II dose-escalating trial. Int J Radiat Oncol Biol Phys. 2000. 47:343–352.12. Martinez AA, Pataki I, Edmundson G, Sebastian E, Brabbins D, Gustafson G. Phase II prospective study of the use of conformal high-dose-rate brachytherapy as monotherapy for the treatment of favorable stage prostate cancer: a feasibility report. Int J Radiat Oncol Biol Phys. 2001. 49:61–69.13. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998. 280:969–974.14. American Society for Therapeutic Radiology and Oncology Consensus Panel. Consensus statement: guidelines for PSA following radiation therapy. Int J Radiat Oncol Biol Phys. 1997. 37:1035–1041.15. Lawton CA, Won M, Pilepich MV, Asbell SO, Shipley WU, Hanks GE, et al. Long-term treatment sequelae following external beam irradiation for adenocarcinoma of the prostate: analysis of RTOG studies 7506 and 7706. Int J Radiat Oncol Biol Phys. 1991. 21:935–939.16. Zelefsky MJ, Fuks Z, Hunt M, Lee HJ, Lombardi D, Ling CC, et al. High dose radiation delivered by intensity modulated conformal radiotherapy improves the outcome of localized prostate cancer. J Urol. 2001. 166:876–881.17. King CR, Lehmann J, Adler JR, Hai J. CyberKnife radiotherapy for localized prostate cancer: rationale and technical feasibility. Technol Cancer Res Treat. 2003. 2:25–30.18. O'Brien PC, Franklin CI, Poulsen MG, Joseph DJ, Spry NS, Denham JW. Trans-Tasman Radiation Oncology Group. Acute symptoms, not rectally administered sucralfate, predict for late radiation proctitis: longer term follow-up of a phase III trial. Int J Radiat Oncol Biol Phys. 2002. 54:442–449.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- New Androgen Receptor Axis-Targeted Agents inthe Treatment of Nonmetastatic Castration-ResistantProstate Cancer: From Bench to Clinical Trials
- CyberKnife(TM) for the Treatment of Non-Metastatic Prostate Cancer
- Clinical Outcomes of CyberKnife Radiotherapy in Prostate Cancer Patients: Short-term, Single-Center Experience
- Hypofractionated stereotactic body radiotherapy in low- and intermediate-risk prostate carcinoma
- Early Experience of Prostate Cancer Treated with CyberKnife(TM) Radiotherapy