Korean J Urol.
2006 Jan;47(1):13-19. 10.4111/kju.2006.47.1.13.
Comparative Study on the Treatment Outcome and Safety of TURP, ILC, TUNA and TEAP for Patients with Benign Prostatic Hyperplasia
- Affiliations
-
- 1Department of Urology, Kosin University Hospital, Busan, Korea. schoi@ns.kosinmed.or.kr
- KMID: 2294209
- DOI: http://doi.org/10.4111/kju.2006.47.1.13
Abstract
-
PURPOSE: We wanted to compare the treatment outcome, safety, efficacy and complications of transurethral resection of the prostate (TURP), interstitial laser coagulation (ILC), transurethral needle ablation (TUNA) and transurethral ethanol ablation of the prostate (TEAP) for the treatment of benign prostatic hyperplasia (BPH).
MATERIALS AND METHODS
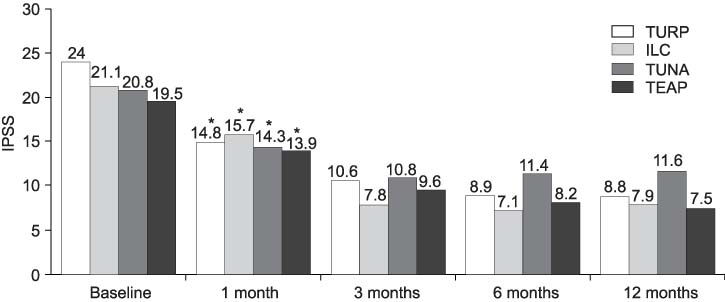
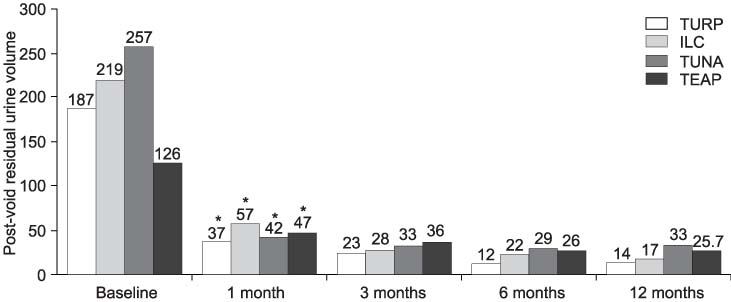
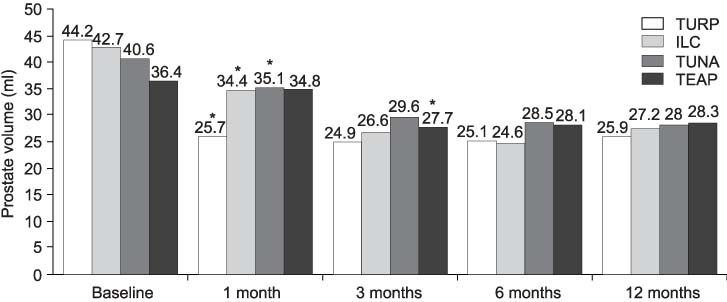
In this prospective, randomized study, a total of 403 patients with symptomatic BPH were treated by TURP, ILC, TUNA or TEAP from January 1998 to December 2002. ILC was performed using the Indigo 830e LaserOptic(TM) System with a specially designed interstitial thermotherapy light guide, TUNA was performed using the VidaMed TUNA System and TEAP was performed using the Prostaject(TM) device. The treatment outcomes were evaluated at 3 months, 6 months and 1 year with the International Prostate Symptom Score (IPSS), the prostate volume, the maximal urinary flow rate (Qmax), the post-void residual urine (PVR), and the quality of life (QoL) assessment score.
RESULTS
All the patients in the four groups showed significant improvement for all the parameters. After 1 year, the four groups showed significant improvement in the clinical and voiding parameters (IPSS, Qmax, PVR, prostate volume and QoL). Our results did not show significant differences in the IPSS, prostate volume and QoL among the four groups. However, the TURP group showed a higher Qmax, and the TEAP group showed a less reduced prostate volume than the other groups during the follow-up period (p<0.05). The period of hospital admission showed no significant difference between the ILC, TUNA and TEAP groups, but the TURP group showed a longer hospital admission period compared to the other groups. The TURP group was markedly associated with more complications than the other groups.
CONCLUSIONS
These early results indicate that ILC, TUNA and TEAP are safe, effective and useful alternative therapies to TURP for the patients with symptomatic BPH.
MeSH Terms
Figure
Reference
-
1. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984. 132:474–479.2. Perrin P, Barnes R, Hadley H, Bergman RT. Forty years of transurethral prostatic resection. J Urol. 1976. 116:757–758.3. Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989. 141:243–247.4. Greenberger M, Steiner MS. The University of Tennessee experience with the Indigo 830e laser device for the minimally invasive treatment of benign prostatic hyperplasia: interim analysis. World J Urol. 1998. 16:386–391.5. Kim HH, Kwak C, Seo SI, Chung H, Lee ES, Lee CW. The effects and complications of transurethral resection for benign prostatic hyperplasia: results of long-term follow-up. Korean J Urol. 1996. 37:268–280.6. Mueller-Lisse UG, Heuck AF, Schneede P, Muschter R, Scheidler J, Hofstetter AG, et al. Postoperative MRI in patients undergoing interstitial laser coagulation thermotheraphy of benign prostatic hyperplasia. J Comput Assist Tomogr. 1996. 20:273–278.7. Chandrasekar P, Virdi JS, Kapasi F. Interstitial laser ablation (Indigo®) of the prostate-a randomised prospective study, four year follow up. J Urol. 2002. 167:Suppl. 294. abstract 1162.8. McNicholas TA, Steger AC, Bown SG. Interstitial laser coagulation of the prostate. An experimental study. Br J Urol. 1993. 71:439–434.9. Williams JC. interstitial laser coagulation of the prostate. Tech Urol. 1996. 2:130–135.10. Calkins H, Langberg J, Sousa J, el-Atassi R, Leon A, Kou W, et al. Radiofrequency catheter ablation of accesory atrioventricular connections in 250 patients. Abbreviated therapeutic approach to Wolff-Parkinson-White syndrome. Circulation. 1992. 85:1337–1346.11. Organ LW. Electrophysiologic principles of radiofrequency lesion making. Appl Neurophysiol. 1976. 39:69–76.12. Ramon J, Lynch TH, Eardley I, Ekman P, Frick J, Jungwirth A, et al. Transurethral needle ablation of the prostate for the treatment of benign prostatic hyperplasia: a collaborative multicenter study. Br J Urol. 1997. 80:128–135.13. Naslund MJ, Benson RJ, Cohen ES, Aceves JG, Issa MM. Transurethral needle ablation (TUNA) for BPH in patients with median lobe enlargement-report of a prospective multicenter study. J Urol. 2000. 163:Suppl. 270. abstract 1198.14. Chandrasekar P, Virdi JS, Kapasi F. Transurethral needle ablation of the prostate (TUNA) in the treatment of benign prostatic hyperplasia: a prospective, randomised study, long term results. J Urol. 2003. 169:Suppl. 468. abstract 1754.15. Livraghi T, Festi D, Monti F, Salmi A, Velotti C. US-guided percutaneous alcohol injection of small hepatic and abdominal tumors. Radiology. 1986. 161:309–312.16. Solbiati L, Giangrande A, De Pra L, Bellotti E, Cantu P, Ravetto C. Percutaneous ethanol injection of parathyroid tumors under US guidance: treatment for secondary hyperparathyroidism. Radiology. 1985. 155:607–610.17. Zvara P, Karpman E, Stoppacher R, Esenler AC, Plante MK. Ablation of canine prostate using transurethral intraprostatic absolute ethanol injection. Urology. 1999. 54:411–415.18. Goya N, Ishikawa N, Ito F, Ryoji O, Tokumoto T, Toma H, et al. Ethanol injection therapy of the prostate for benign prostatic hyperplasia: preliminary report on application of a new technique. J Urol. 1999. 162:383–386.19. Aceves JG, Gilling P, Schettini M, Grise P, Sagarra JM, Hernandez C. Transurethral ethanol ablation of the prostate (TEAP), initial long term report of two prospective multicenter studies. J Urol. 2003. 169:Suppl. 466. abstract 1747.20. Koo JH, Choi S, Rhew HY. The comparative study of interstitial laser coagulation and transurethral resection for benign prostatic hyperplasia. Korean J Urol. 2000. 41:1125–1130.21. Schulman CC, Zlotta AR. Transurethral needle ablation of the prostate for treatment of benign prostatic hyperplasia: early clinical experience. Urology. 1995. 45:28–33.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Results Comparing Transurethral Needle Ablation with Transurethral Resection of Prostate for the Treatment of Benign Prostatic Hyperplasia
- A Comparative Study of Visual Laser Ablation of the Prostate(VLAP) and Interstitial Laser Coagulation(ILC) in Benign Prostatic Hyperplasia
- The Efficacy of Transurethral Resection of Prostate in the Patients with Benign Prostatic Hyperplasia of 30gm or Less
- Effect of Transurethral Ethanol Injection of Prostate for Recurrent Urinary Retention in Patients with a Poor Performace Status
- Is transurethral needle ablation of prostate out of fashion? Outcomes of single session office-based transurethral needle ablation of prostate in patients with symptomatic benign prostatic hyperplasia