Korean J Urol.
2006 Mar;47(3):293-297. 10.4111/kju.2006.47.3.293.
The Efficacy of Imaging Studies after a First Febrile Urinary Tract Infection in Young Children with Normal Prenatal Ultrasonographic Findings
- Affiliations
-
- 1Department of Urology, Hanyang University College of Medicine, Seoul, Korea. qpqp@hanyang.ac.kr
- KMID: 2294177
- DOI: http://doi.org/10.4111/kju.2006.47.3.293
Abstract
-
PURPOSE: The primary purpose for imaging the urinary tract of children with urinary tract infection is to detect congenital anomalies that may predispose the children to persistent or recurrent infection and also to prevent progressive renal deterioration. We evaluated the efficacy of imaging studies after a first febrile urinary tract infection in young children with normal prenatal ultrasonographic findings.
MATERIALS AND METHODS
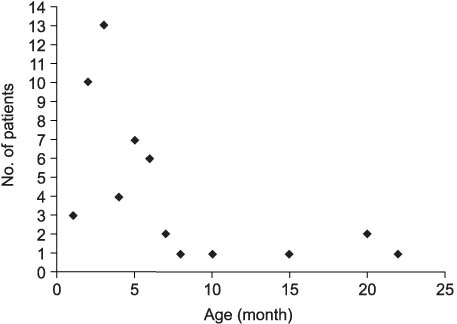
We retrospectively reviewed 52 young children who were treated due to their first febrile urinary tract infection between 2001 and 2003. In all cases, urine specimens were collected via suprapubic aspiration. An the ultrasonogram and dimercaptosuccinic acid (DMSA) renal scans were obtained within 48 and 72 hours after hospitalization. Contrast voiding cystourethrograms were obtained within 1 to 4 week later after controlling the urinary tract infection.
RESULTS
On the ultrasonographic studies, 43 children (90%) were normal and 9 children (10%) were abnormal, and all of these abnormalities were upper tract dilatation that was not due to obstructive uropathy. DMSA renal scans revealed acute pyelonephritis in 34 children (65%) and normal findings in 18 (35%). Voiding cystourethrogram revealed reflux in 15 children (31%). 4 children had Grade II reflux, 1 child had III reflux and 9 children had grade IV reflux.
CONCLUSIONS
After the first febrile urinary tract infection in young children with normal prenatal ultrasonographic findings, an ultrasonogram performed at the time of acute illness is of limited value for the clinical decision about further treatment. A DMSA renal scan is useful for identifying pyelonephritis and renal scar, but its effect on the outcomes is unclear. Voiding cystourethrogram is most useful imaging study for identifying the reflux that needs antimicrobial prophylaxis for reducing reinfections and to prevent renal scarring.
MeSH Terms
Figure
Reference
-
1. Spencer JR, Schaeffer AJ. Pediatric urinary tract infections. Urol Clin North Am. 1986. 13:661–672.2. American Academy of Pediatrics. Practice parameter: the diagnosis, treatment and evaulation of the initial urinary tract infection in febrile infants and young children. Pediatrics. 1999. 103:843–852.3. Dick PT, Feldman W. Routine diagnostic imaging for childhood urinary tract infections: a systematic overview. J Pediatr. 1996. 128:15–22.4. Hellerstein S. Recurrent urinary tract infections in children. Pediatr infect Dis. 1982. 1:271–281.5. Medical versus surgical treatment of primary vesicoureteral reflux report of the International Reflux Study Committee. Pediatrics. 1981. 67:392–400.6. Hoberman A, Chao HP, Keller DM, Hickey R, Davis HW, Ellis D. Prevalence of urinary tract infection in febrile infants. J Pediatr. 1993. 123:17–23.7. Andrich MA, Majd M. Diagnostic imaging in the evaluation of the first urinary tract infection in infants and young children. Pediatrics. 1992. 90:436–441.8. Kang YS, Han SW, Choi SK. The ultrasonographic follow up results and the prognosis of prenatal hydronephrosis. Korean J Urol. 1995. 36:1100–1105.9. Chitty LS, Pembrey ME, Chudleigh PM, Campbell S. Multicentre study of antenatal calyceal dilatation detected by ultrasound. Lancet. 1990. 336:875.10. Zerin JM, Richey ML, Chang AC. Incidental vesicoureteral reflux in neonates with antenatally detected hydronephrosis and other renal abnormalities. Radiology. 1993. 187:157–160.11. Foresman WH, Hulbert WC Jr, Rabinowitz R. Does urinary tract ultrasonography at hospitalization for acute pyelonephritis predict vesicoureteral reflux? J Urol. 2001. 165:2232–2234.12. Kass EJ, Fink-Bennett D, Cacciarelli AA, Balon H, Pavlock S. The sensitivity of renal scintigraphy and sonography in detecting nonobstructive acute pyelonephritis. J Urol. 1992. 148:606–608.13. Nguyen HT, Bauer SB, Peters CA, Connolly LP, Gobet R, Borer JG, et al. 99mTc dimercapto-succinic acid renal scintigraphy abnormalities in infants sterile high grade vesicoureteral reflux. J Urol. 2000. 164:1674–1678.14. Hoberman A, Charron M, Hickey RW, Baskin M, Kearney DH, Wald ER. Imaging studies after a first febrile urinary tract infection in young children. N Engl J Med. 2003. 348:195–202.15. Corteville JE, Gray DL, Crane JP. Congenital hydronephrosis: correlation of fetal ultrasonographic findings with infant outcome. Am J Obstet Gynecol. 1991. 165:384–388.16. Stokland E, Hellstrom M, Hansson S, Jodal U, Oden A, Jacobsson B. Reliability of ultrasonography in identification of reflux nephropathy in children. BMJ. 1994. 309:235–239.17. Benador D, Benador N, Slosman DO, Nussle D, Mermillord B, Girardin E. Cortical scintigraphy in the evaluation of renal parenchymal changes in children with pyelonephritis. J Pediatr. 1994. 124:17–20.18. Melis K, Vandevivere J, Hoskens C, Vervaet A, Sand A, Van Acker KJ. Involvement of the renal parenchyma in acute urinary tract infection : the contribution of 99mTc dimercaptosuccinic acid scan. Eur J Pediatr. 1992. 151:536–539.19. Verboven J, Ingels M, Delree M, Piepsz A. 99mTc-DMSA scintigraphy in acute urinary infection in children. Pediatr Radiol. 1990. 20:540–542.20. Merguerian PA, Jamal MA, Agarwal SK, McLorie GA, Bagli DJ, Shuchett B, et al. Utility of spect DMSA renal scanning in the evaluation of children with primary vesicoureteral reflux. Urology. 1999. 53:1024–1028.21. Blickman JG, Taylor GA, Lebowitz RL. Voiding cystourethrography: the initial radiologic study in children with urinary tract infection. Radiology. 1985. 156:659–662.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Ultrasonographic Follow up Results and the Prognosis of Prenatal Hydronephrosis
- The Diagnostic Efficacy of Abdominal Ultrasonography for Evaluation of Children with Urinary Tract Infection
- Urinary YKL-40 as a Candidate Biomarker for Febrile Urinary Tract Infection in Young Children
- Urinary Tract Infection in Children: Role of Ultrasonography
- Diagnosis and Treatment of the Urinary Tract Infection in Febrile Infants and Children