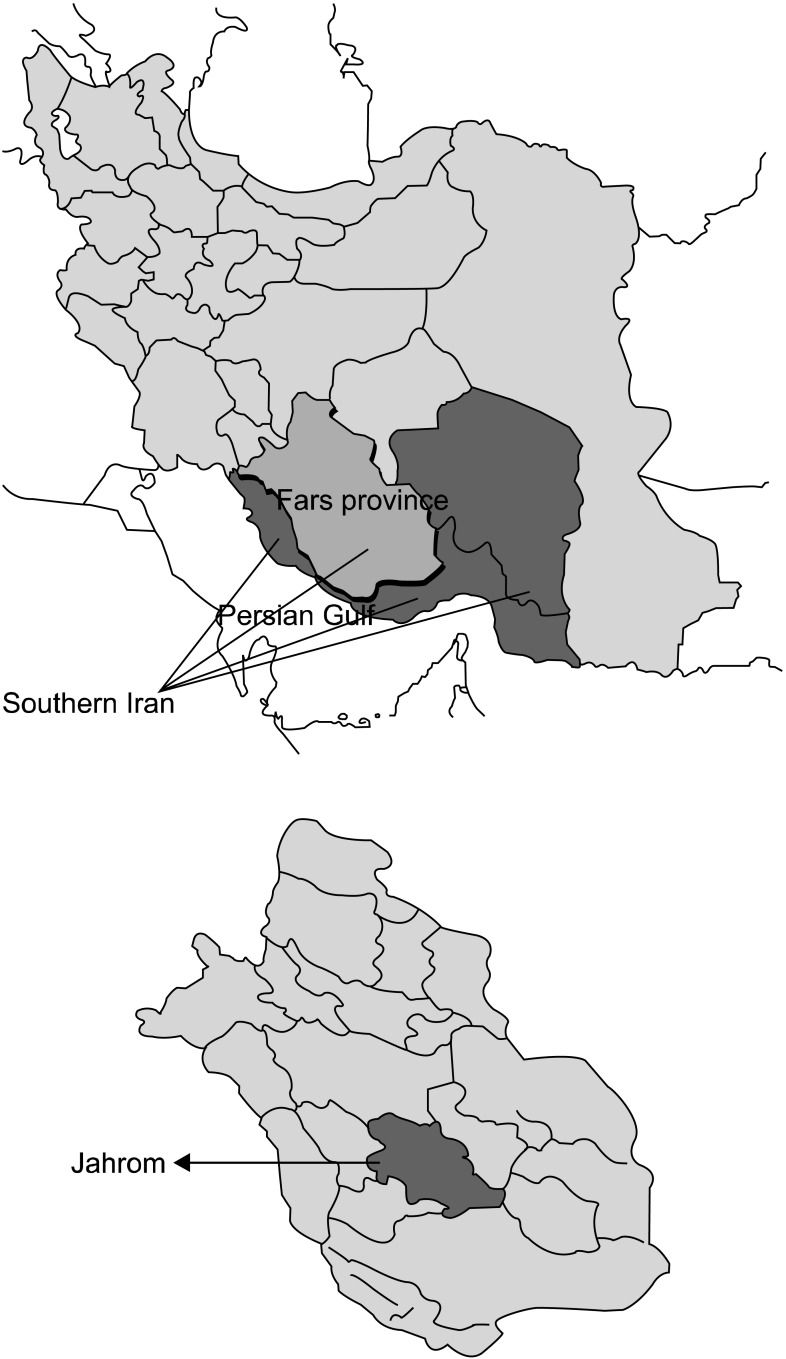
Chronic Pain and Its Determinants: A Population-based Study in Southern Iran
- Affiliations
-
- 1Department of Physiology, Medicine School, Jahrom University of Medical Sciences, Jahrom, Iran.
- 2Department of Statistics, Medicine School, Jahrom University of Medical Sciences, Jahrom, Iran.
- 3Department of Anatomy, Medicine School, Jahrom University of Medical Sciences, Jahrom, Iran.
- 4Department of Student Research Committee, Jahrom University of Medical Sciences, Jahrom, Iran. min_m505@yahoo.com
- KMID: 2278165
- DOI: http://doi.org/10.3344/kjp.2012.25.4.245
Abstract
- BACKGROUND
Prevalence of chronic pain and its association with demographic characteristics have been reported by different studies from different geographical regions in the world. However, data from many Middle East countries including Iran (especially southern Iran) are scare. The aim of the present study was to demonstrate the prevalence of chronic pain and its association with demographic, psychological and socioeconomic factors in an Iranian population.
METHODS
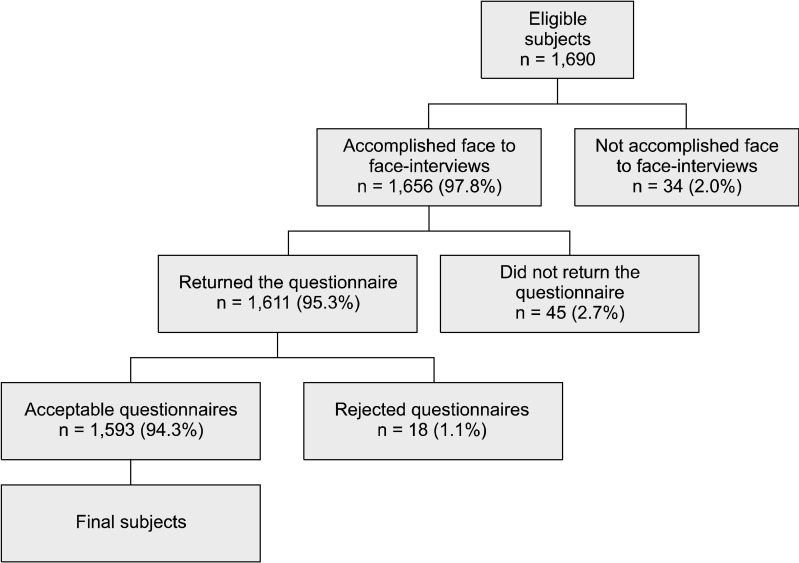
In this population-based survey, the target population was comprised of subjects aged 20 to 85 years residing in Jahrom, southern Iran during 2009-2011. All eligible subjects were invited to participate in the study. Before a detailed questionnaire was given; face to face interviews were done for each individual.
RESULTS
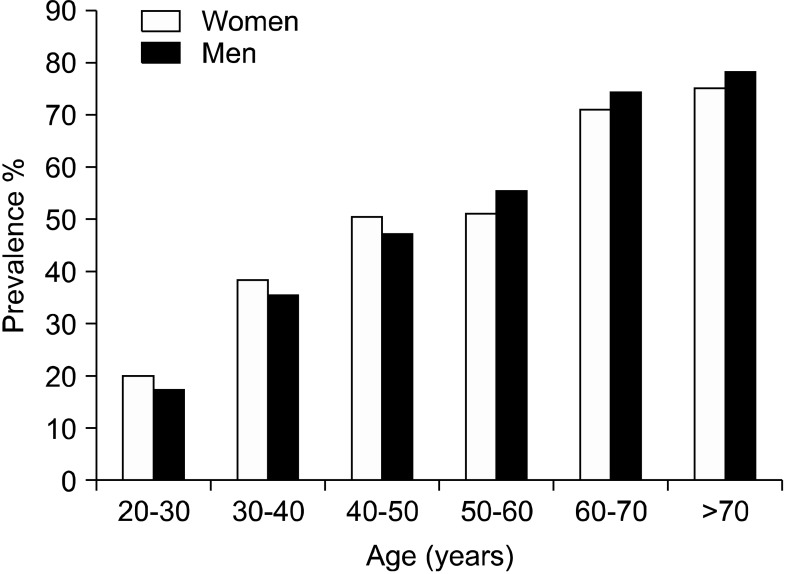
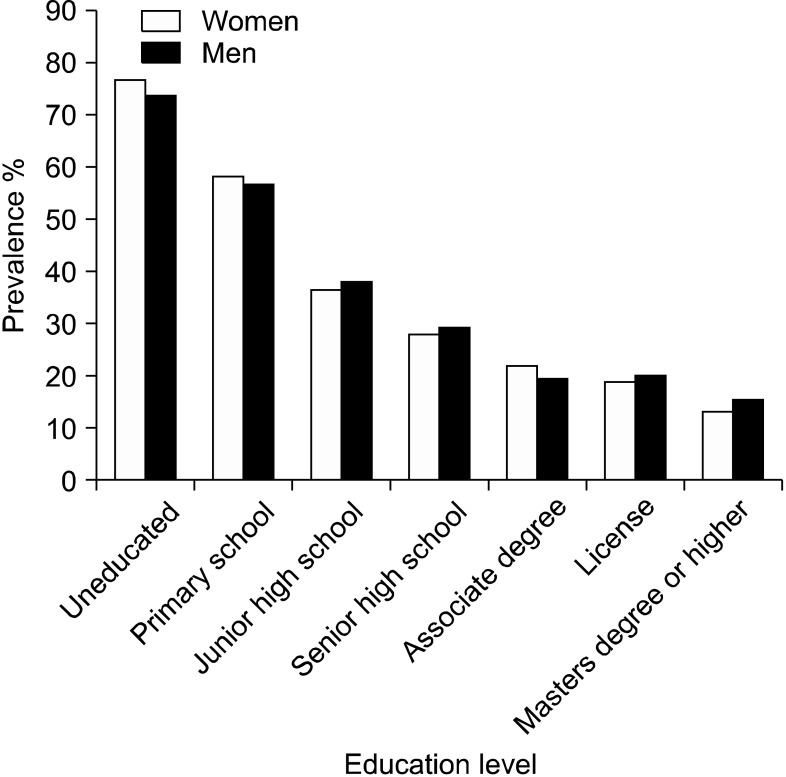
There were 719 men and 874 women with an average age of 40.5 years at the onset of the study. Among the study population, 38.9% (620/1,593) complained of chronic pain, of whom 40.8% (253/620) were men and 59.2% (367/620) were women. Foot and joint pain were observed in 31.9%. Hip and spine pain, migraine and tension headaches, heart pain, and abdomen pain were observed in 21.5%, 15.5%, 9.5%, and 8.0% of chronic pain cases, respectively. There was a significant association among the covariables age, sex, overweight, educational level, income, and type of employment with chronic pain as the dependent variable (P < 0.0001).
CONCLUSIONS
Our findings show the prevalence of chronic pain and its association with demographic, psychological and socioeconomic factors. Individuals with low incomes and less education became accustomed to pain due to a lack of knowledge.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
The antinociceptive effect of artemisinin on the inflammatory pain and role of GABAergic and opioidergic systems
Faraz Mahdian Dehkordi, Jahangir Kaboutari, Morteza Zendehdel, Moosa Javdani
Korean J Pain. 2019;32(3):160-167. doi: 10.3344/kjp.2019.32.3.160.Model Determination of Delayed Causes of Analgesics Prescription in the Emergency Ward in Arak, Iran
Ali Cyrus, Mehrdad Moghimi, Abolfazle Jokar, Mohammad Rafeie, Ali Moradi, Parisa Ghasemi, Hanieh Shahamat, Ali Kabir
Korean J Pain. 2014;27(2):152-161. doi: 10.3344/kjp.2014.27.2.152.Prevalence and trends of pain associated with chronic diseases and personal out-of-pocket medical expenditures in Korea
Sun Mi Shin
Korean J Pain. 2017;30(2):142-150. doi: 10.3344/kjp.2017.30.2.142.“I'm healthy, I don't have pain”- health screening participation and its association with chronic pain in a low socioeconomic status Singaporean population
Liang En Wee, David Sin, Wen Qi Cher, Zong Chen Li, Tammy Tsang, Sabina Shibli, Gerald Koh
Korean J Pain. 2017;30(1):34-43. doi: 10.3344/kjp.2017.30.1.34.
Reference
-
1. Cho SK, Heiby EM, McCracken LM, Moon DE, Lee JH. Daily functioning in chronic pain: study of structural relations with posttraumatic stress disorder symptoms, pain intensity, and pain avoidance. Korean J Pain. 2011; 24:13–21. PMID: 21390174.
Article2. van Dijk A, McGrath PA, Pickett W, VanDenKerkhof EG. Pain prevalence in nine- to 13-year-old schoolchildren. Pain Res Manag. 2006; 11:234–240. PMID: 17149456.3. Gagliese L, Melzack R. Chronic pain in elderly people. Pain. 1997; 70:3–14. PMID: 9106804.
Article4. Sjøgren P, Ekholm O, Peuckmann V, Grønbaek M. Epidemiology of chronic pain in Denmark: an update. Eur J Pain. 2009; 13:287–292. PMID: 18547844.
Article5. Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain. 2010; 11:1230–1239. PMID: 20797916.
Article6. Mohseni-Bandpei MA, Fakhri M, Ahmad-Shirvani M, Bagheri-Nessami M, Khalilian AR, Shayesteh-Azar M, et al. Low back pain in 1,100 Iranian pregnant women: prevalence and risk factors. Spine J. 2009; 9:795–801. PMID: 19574106.
Article7. Leighton DJ, Reilly T. Epidemiological aspects of back pain: the incidence and prevalence of back pain in nurses compared to the general population. Occup Med (Lond). 1995; 45:263–267. PMID: 7579302.
Article8. Palmer KT, Walsh K, Bendall H, Cooper C, Coggon D. Back pain in Britain: comparison of two prevalence surveys at an interval of 10 years. BMJ. 2000; 320:1577–1578. PMID: 10845966.
Article9. Blyth FM, March LM, Brnabic AJ, Jorm LR, Williamson M, Cousins MJ. Chronic pain in Australia: a prevalence study. Pain. 2001; 89:127–134. PMID: 11166468.
Article10. Hanna M. Pain in Europe: a public health priority. J Pain Palliat Care Pharmacother. 2012; 26:182–184.
Article11. Yeo SN, Tay KH. Pain prevalence in Singapore. Ann Acad Med Singapore. 2009; 38:937–942. PMID: 19956814.12. Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clin Geriatr Med. 2001; 17:417–431. PMID: 11459713.
Article13. Stronks K, van de Mheen H, van den Bos J, Mackenbach JP. The interrelationship between income, health and employment status. Int J Epidemiol. 1997; 26:592–600. PMID: 9222785.
Article14. Mäntyselkä PT, Turunen JH, Ahonen RS, Kumpusalo EA. Chronic pain and poor self-rated health. JAMA. 2003; 290:2435–2442. PMID: 14612480.
Article15. Green CR, Ndao-Brumblay SK, Nagrant AM, Baker TA, Rothman E. Race, age, and gender influences among clusters of African American and white patients with chronic pain. J Pain. 2004; 5:171–182. PMID: 15106130.
Article16. Saastamoinen P, Leino-Arjas P, Laaksonen M, Lahelma E. Socio-economic differences in the prevalence of acute, chronic and disabling chronic pain among ageing employees. Pain. 2005; 114:364–371. PMID: 15777862.
Article17. Poleshuck EL, Green CR. Socioeconomic disadvantage and pain. Pain. 2008; 136:235–238. PMID: 18440703.
Article18. Hagen K, Zwart JA, Svebak S, Bovim G, Jacob Stovner L. Low socioeconomic status is associated with chronic musculoskeletal complaints among 46,901 adults in Norway. Scand J Public Health. 2005; 33:268–275. PMID: 16087489.
Article19. Loisel P, Durand P, Abenhaim L, Gosselin L, Simard R, Turcotte J, et al. Management of occupational back pain: the Sherbrooke model. Results of a pilot and feasibility study. Occup Environ Med. 1994; 51:597–602. PMID: 7951791.
Article20. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006; 10:287–333. PMID: 16095934.
Article21. Gustorff B, Dorner T, Likar R, Grisold W, Lawrence K, Schwarz F, et al. Prevalence of self-reported neuropathic pain and impact on quality of life: a prospective representative survey. Acta Anaesthesiol Scand. 2008; 52:132–136. PMID: 17976220.
Article22. Park HJ, Moon DE. Pharmacologic management of chronic pain. Korean J Pain. 2010; 23:99–108. PMID: 20556211.
Article23. Oladeji BD, Makanjuola VA, Esan OB, Gureje O. Chronic pain conditions and depression in the Ibadan Study of Ageing. Int Psychogeriatr. 2011; 1–7. PMID: 21241528.
Article24. Meana M, Cho R, DesMeules M. Chronic pain: the extra burden on Canadian women. BMC Womens Health. 2004; 4(Suppl 1):S17. PMID: 15345080.
Article25. Maruta T, Osborne D. Sexual activity in chronic pain patients. Psychosomatics. 1978; 19:531–537. PMID: 704780.
Article26. Dunn KS. Testing a middle-range theoretical model of adaptation to chronic pain. Nurs Sci Q. 2005; 18:146–156. PMID: 15802747.
Article27. Katz JN. Lumbar disc disorders and low-back pain: socio-economic factors and consequences. J Bone Joint Surg Am. 2006; 88(Suppl 2):21–24. PMID: 16595438.
Article28. Deyo RA, Tsui-Wu YJ. Functional disability due to back pain. A population-based study indicating the importance of socioeconomic factors. Arthritis Rheum. 1987; 30:1247–1253. PMID: 2961343.
Article29. Pincus T, Callahan LF, Burkhauser RV. Most chronic diseases are reported more frequently by individuals with fewer than 12 years of formal education in the age 18-64 United States population. J Chronic Dis. 1987; 40:865–874. PMID: 3597688.
Article30. Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004; 50:3145–3152. PMID: 15476248.
Article31. Ghaffari M, Alipour A, Jensen I, Farshad AA, Vingard E. Low back pain among Iranian industrial workers. Occup Med (Lond). 2006; 56:455–460. PMID: 16837536.
Article32. Asghari A, Ghaderi N, Ashory A. The prevalence of pain among residents of nursing homes and the impact of pain on their mood and quality of life. Arch Iran Med. 2006; 9:368–373. PMID: 17061612.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of chronic pain and contributing factors: a cross-sectional population-based study among 2,379 Iranian adolescents
- An Update on the Management of Diabetic Neuropathic Pain: A Few Comments
- The effects of water-pipe smoking on birth weight: a population-based prospective cohort study in southern Iran
- Combined Use of Intrathecal Opioids and Dexmedetomidine in the Management of Neuropathic Pain
- Social determinants of adherence to COVID-19 preventive guidelines: a comprehensive review