Ann Rehabil Med.
2013 Oct;37(5):658-667. 10.5535/arm.2013.37.5.658.
Treatment Effects of Ultrasound Guide Selective Nerve Root Block for Lower Cervical Radicular Pain: A Retrospective Study of 1-Year Follow-up
- Affiliations
-
- 1Department of Rehabilitation Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 2Department of Health & Fitness Management, Namseoul University, Cheonan, Korea.
- 3Department of Radiology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 4Department of Family Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 5Department of Rehabilitation Medicine, Gachon University Gil Medical Center, Incheon, Korea. bduck@gachon.ac.kr
- KMID: 2266583
- DOI: http://doi.org/10.5535/arm.2013.37.5.658
Abstract
OBJECTIVE
To compare the long-term effects and advantages of ultrasound (US)-guided selective cervical nerve root block with fluoroscopy (FL)-guided transforaminal block.
METHODS
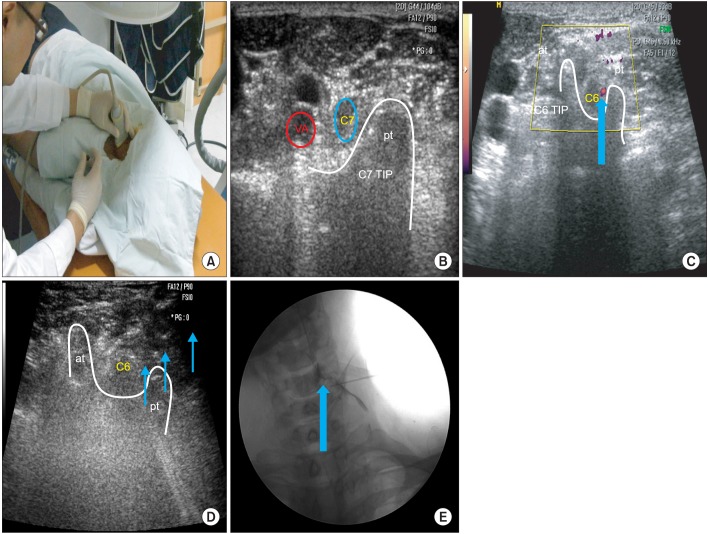
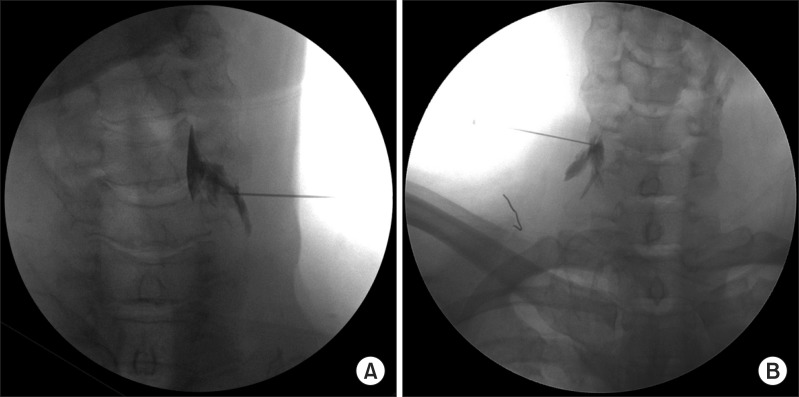
From March 2009 to November 2012, 162 patients received steroid injections for lower cervical radicular pain. A total of 114 patients fulfilled the inclusion criteria. All procedures were performed by using US or FL. We compared the intravascular injections during the procedure with the effects and functional scales at 3, 6, and 12 months after the procedure between the two groups. Successful treatments occurred when patients obtained significant pain reliefs (as measured by >50% improvements in the verbal numerical scale [VNS] score and >40% improvements in the neck disability index [NDI] score) and reported a patient satisfaction score of 3 or 4 points at 12 months after the injection. Image analysis of intravascular injection and chart review were performed. Logistic regression was performed to reveal the correlations between successful treatments and variables (patient's age, gender, duration of the disease, cause, injection method, and radiologic finding).
RESULTS
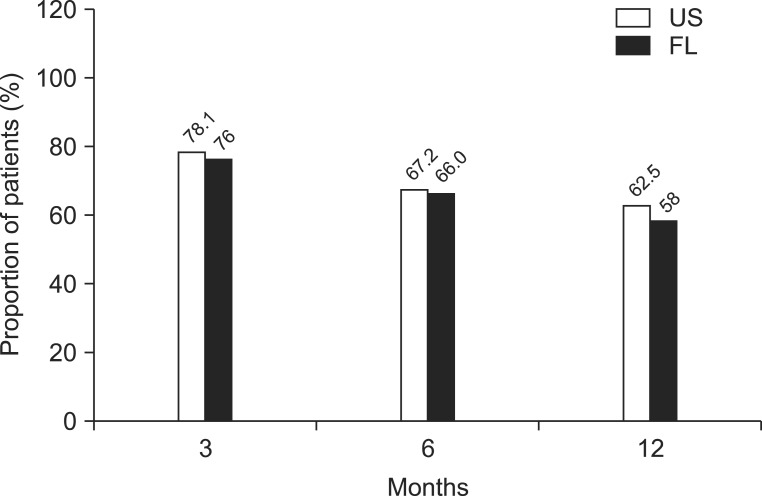
The VNS and NDI improved 3 months after the injection and continued to improve until 12 months for both groups. But there were no statistical differences in changes of VNS, NDI, and effectiveness between these two groups. The proportion of patients with successful treatment is illustrated as 62.5% in US-guided group and 58% in FL-guided group at 12 months. There were no significant differences between the groups or during follow-up periods. Three cases of the intravascular injections were done in FL-guided group.
CONCLUSION
The US-guided selective cervical nerve root blocks are facilitated by identifying critical vessels at unexpected locations relative to the foramen and to protect injury to such vessels, which is the leading cause of reported complications from FL-guided transforaminal blocks. On treatment effect, significant long-term improvements in functions and pain reliefs were observed in both groups after the intervention. However, significant differences were not observed between the groups. Therefore, the US-guided selective cervical nerve root block was shown to be as effective as the FL-guided transforaminal block in pain reliefs and functional improvements, in addition to the absence of radiation and protection vessel injury at real-time imaging.
MeSH Terms
Figure
Cited by 1 articles
-
When is the Optimal Time Point for Predicting the 1-Year Follow-up Outcome of Selective Nerve Root Block for Cervical Radiculopathy?
Whee Sung Son, Myun-Whan Ahn, Gun Woo Lee
J Korean Soc Spine Surg. 2019;26(2):40-49. doi: 10.4184/jkss.2019.26.2.40.
Reference
-
1. Slipman CW, Lipetz JS, Jackson HB, Rogers DP, Vresilovic EJ. Therapeutic selective nerve root block in the nonsurgical treatment of atraumatic cervical spondylotic radicular pain: a retrospective analysis with independent clinical review. Arch Phys Med Rehabil. 2000; 81:741–746. PMID: 10857517.
Article2. Boswell MV, Hansen HC, Trescot AM, Hirsch JA. Epidural steroids in the management of chronic spinal pain and radiculopathy. Pain Physician. 2003; 6:319–334. PMID: 16880879.3. Manchikanti L. Transforaminal lumbar epidural steroid injections. Pain Physician. 2000; 3:374–398. PMID: 16906179.
Article4. Narouze SN, Vydyanathan A, Kapural L, Sessler DI, Mekhail N. Ultrasound-guided cervical selective nerve root block: a fluoroscopy-controlled feasibility study. Reg Anesth Pain Med. 2009; 34:343–348. PMID: 19574867.5. Yamauchi M, Suzuki D, Niiya T, Honma H, Tachibana N, Watanabe A, et al. Ultrasound-guided cervical nerve root block: spread of solution and clinical effect. Pain Med. 2011; 12:1190–1195. PMID: 21692976.
Article6. Jee H, Lee JH, Kim J, Park KD, Lee WY, Park Y. Ultrasound-guided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: a randomized, blinded, controlled study. Skeletal Radiol. 2013; 42:69–78. PMID: 22609989.
Article7. Galiano K, Obwegeser AA, Bodner G, Freund MC, Gruber H, Maurer H, et al. Ultrasound-guided periradicular injections in the middle to lower cervical spine: an imaging study of a new approach. Reg Anesth Pain Med. 2005; 30:391–396. PMID: 16032592.
Article8. Smuck M, Maxwell MD, Kennedy D, Rittenberg JD, Lansberg MG, Plastaras CT. Utility of the anesthetic test dose to avoid catastrophic injury during cervical transforaminal epidural injections. Spine J. 2010; 10:857–864. PMID: 20692210.
Article9. Nahm FS, Lee CJ, Lee SH, Kim TH, Sim WS, Cho HS, et al. Risk of intravascular injection in transforaminal epidural injections. Anaesthesia. 2010; 65:917–921. PMID: 20645947.10. Hartrick CT, Kovan JP, Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract. 2003; 3:310–316. PMID: 17166126.
Article11. Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther. 1991; 14:409–415. PMID: 1834753.12. Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V. Lumbar facet joint nerve blocks in managing chronic facet joint pain: one-year follow-up of a randomized, double-blind controlled trial. Clinical Trial NCT00355914. Pain Physician. 2008; 11:121–132. PMID: 18354721.13. Baker R, Dreyfuss P, Mercer S, Bogduk N. Cervical transforaminal injection of corticosteroids into a radicular artery: a possible mechanism for spinal cord injury. Pain. 2003; 103:211–215. PMID: 12749976.
Article14. Houten JK, Errico TJ. Paraplegia after lumbosacral nerve root block: report of three cases. Spine J. 2002; 2:70–75. PMID: 14588291.15. McLain RF, Fry M, Hecht ST. Transient paralysis associated with epidural steroid injection. J Spinal Disord. 1997; 10:441–444. PMID: 9355063.
Article16. Muro K, O'Shaughnessy B, Ganju A. Infarction of the cervical spinal cord following multilevel transforaminal epidural steroid injection: case report and review of the literature. J Spinal Cord Med. 2007; 30:385–388. PMID: 17853663.
Article17. Narouze S, Peng PW. Ultrasound-guided interventional procedures in pain medicine: a review of anatomy, sonoanatomy, and procedures. Part II: axial structures. Reg Anesth Pain Med. 2010; 35:386–396. PMID: 20607896.18. Huntoon MA. Anatomy of the cervical intervertebral foramina: vulnerable arteries and ischemic neurologic injuries after transforaminal epidural injections. Pain. 2005; 117:104–111. PMID: 16055268.
Article19. Tiso RL, Cutler T, Catania JA, Whalen K. Adverse central nervous system sequelae after selective transforaminal block: the role of corticosteroids. Spine J. 2004; 4:468–474. PMID: 15246308.20. Derby R, Lee SH, Date ES, Lee JH, Lee CH. Size and aggregation of corticosteroids used for epidural injections. Pain Med. 2008; 9:227–234. PMID: 18298706.
Article21. Furman MB, Mehta AR, Kim RE, Simon JI, Patel R, Lee TS, et al. Injectate volumes needed to reach specific landmarks in lumbar transforaminal epidural injections. PM R. 2010; 2:625–635. PMID: 20659718.
Article22. Dreyfuss P, Baker R, Bogduk N. Comparative effectiveness of cervical transforaminal injections with particulate and nonparticulate corticosteroid preparations for cervical radicular pain. Pain Med. 2006; 7:237–242. PMID: 16712623.
Article23. Choi BI, Han JM, Kweon TD, Lee YW. The prognostic factors of selective transforaminal epidural block in patients with low back pain. Korean J Pain. 2007; 20:54–59.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Spinal Cord Injury after Cervical Nerve Root Block
- The Effect of Nerve Root Block on the Patients Who Are Considered as Surgical Candidates with Cervical Radicular Pain
- The Effectiveness of Ultrasound-Guided Selective Nerve Root Block for the Treatment of Radicular Pain in the Lower Cervical Spine: An Assessment of Sustainability and Side Effects
- The Efficacy and Persistence of Selective Nerve Root Block under Fluoroscopic Guidance for Cervical Radiculopathy
- Selective Spinal Nerve Root Block for the Treatment of Sciatica