J Korean Orthop Assoc.
2018 Apr;53(2):166-173. 10.4055/jkoa.2018.53.2.166.
The Effectiveness of Ultrasound-Guided Selective Nerve Root Block for the Treatment of Radicular Pain in the Lower Cervical Spine: An Assessment of Sustainability and Side Effects
- Affiliations
-
- 1Department of Orthopedic Surgery, Kosin University Gospel Hospital, Busan, Korea. mewha98@naver.com
- KMID: 2410065
- DOI: http://doi.org/10.4055/jkoa.2018.53.2.166
Abstract
- PURPOSE
The purpose of this study was to evaluate the sustainability and adverse effects of ultrasound-guided selective nerve root block in patients who complained of radiculopathy due to lower cervical disc herniation.
MATERIALS AND METHODS
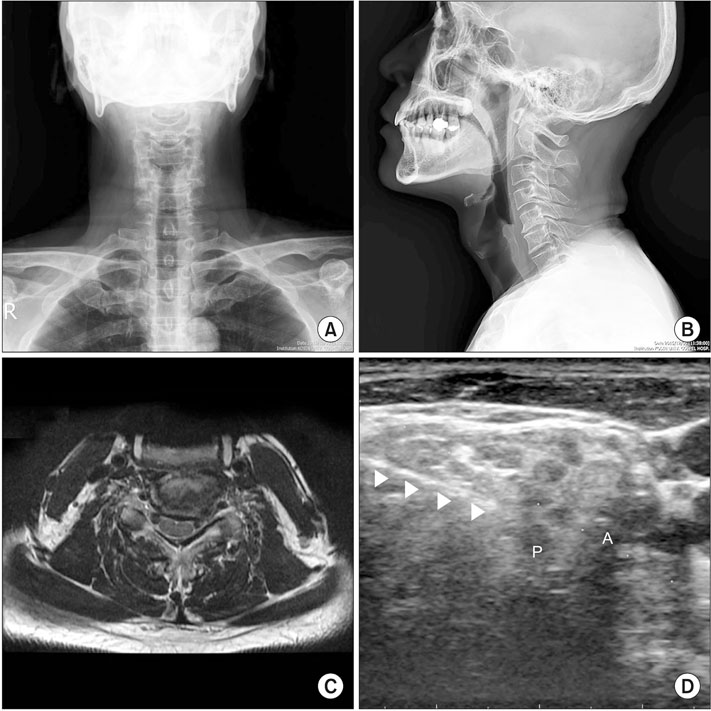
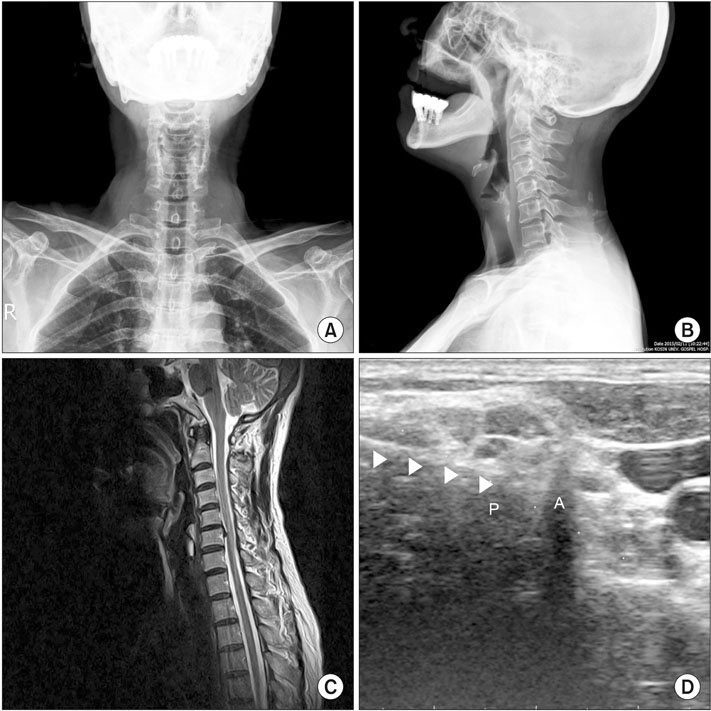
Between February 2014 and February 2016, 39 out of 60 patients who visited Department of Orthopedic Surgery, Kosin University Gospel Hospital with a chief complaint of radiculopathy due to lower cervical disc herniation were treated with an ultrasound-guided selective nerve root block. To evaluate the efficacy and sustainability of this treatment, the degree of pain relief and functional improvement were evaluated before and 3 months after the procedure. Patients were categorized into two groups: The soft disc group and the hard disc group. The safety of the procedure was evaluated by examining the side effects occurring immediately after the procedure and the following day.
RESULTS
Visual analogue scale and Neck Disability Index were improved from 6.00 to 3.02 and from 15.82 to 6.15, respectively (p < 0.05). There were 2 cases of headache and 2 cases of dizziness; however, they were resolved within 1 hour after the procedure. In 32 patients (82.1%), there was improvement in pain, which persisted for more than 3 months in 24 patients. Contrastinly, 7 patients (17.9%) showed no improvement and 6 patients (15.4%) experienced recurrence of pain or symptoms within 1 month after the procedure. In the soft disc group, there was a reduction in pain, from a score of 5.88 before the procedure to 2.64 twelve weeks after the procedure (p < 0.01). In the hard disc group, there was also a reduction in, from a score of 6.09 before the procedure to 3.22 at postoperative 12 weeks (p < 0.01). There was no significant difference between the two groups.
CONCLUSION
In patients with cervical disc herniation, an ultrasound-guided selective nerve root block appears to be an effective treatment option for outpatients due to its low risk of serious complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Rathmell JP, Aprill C, Bogduk N. Cervical transforaminal injection of steroids. Anesthesiology. 2004; 100:1595–1600.
Article2. Wallace MA, Fukui MB, Williams RL, Ku A, Baghai P. Complications of cervical selective nerve root blocks performed with fluoroscopic guidance. AJR Am J Roentgenol. 2007; 188:1218–1221.
Article3. Brouwers PJ, Kottink EJ, Simon MA, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001; 91:397–399.
Article4. Huston CW, Slipman CW, Garvin C. Complications and side effects of cervical and lumbosacral selective nerve root injections. Arch Phys Med Rehabil. 2005; 86:277–283.
Article5. Ma DJ, Gilula LA, Riew KD. Complications of fluoroscopically guided extraforaminal cervical nerve blocks. An analysis of 1036 injections. J Bone Joint Surg Am. 2005; 87:1025–1030.6. Shim DM, Kim YM, Oh SK, Lim CM, Kown BT. Radiation induced hand necrosis of an orthopaedic surgeon who had treated a patient with fluoroscopy-guided spine injection. J Korean Orthop Assoc. 2014; 49:250–254.
Article7. Nakagawa M, Shinbori H, Ohseto K. Ultrasound-guided and fluoroscopy-assisted selective cervical nerve root blocks. Masui. 2009; 58:1506–1511.8. Narouze SN, Vydyanathan A, Kapural L, Sessler DI, Mekhail N. Ultrasound-guided cervical selective nerve root block: a fluoroscopy-controlled feasibility study. Reg Anesth Pain Med. 2009; 34:343–348.9. Martinoli C, Bianchi S, Santacroce E, Pugliese F, Graif M, Derchi LE. Brachial plexus sonography: a technique for assessing the root level. AJR Am J Roentgenol. 2002; 179:699–702.
Article10. Galiano K, Obwegeser AA, Bodner G, et al. Ultrasound-guided periradicular injections in the middle to lower cervical spine: an imaging study of a new approach. Reg Anesth Pain Med. 2005; 30:391–396.
Article11. Yamauchi M, Suzuki D, Niiya T, et al. Ultrasound-guided cervical nerve root block: spread of solution and clinical effect. Pain Med. 2011; 12:1190–1195.
Article12. Jee H, Lee JH, Kim J, Park KD, Lee WY, Park Y. Ultrasound-guided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: a randomized, blinded, controlled study. Skeletal Radiol. 2013; 42:69–78.
Article13. Yamano Y. Soft disc herniation of the cervical spine. Int Orthop. 1985; 9:19–27.
Article14. Bush K, Chaudhuri R, Hellier S, Penny J. The pathomorphologic changes that accompany the resolution of cervical radiculopathy. A prospective study with repeat magnetic resonance imaging. Spine (Phila Pa 1976). 1997; 22:183–186. discussion 187.
Article15. McLain RF, Kapural L, Mekhail NA. Epidural steroid therapy for back and leg pain: mechanisms of action and efficacy. Spine J. 2005; 5:191–201.
Article16. Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am. 1971; 53:891–903.17. Razzaq AA, O'Brien D, Mathew B, Bartlett R, Taylor D. Efficacy and durability of fluoroscopically guided cervical nerve root block. Br J Neurosurg. 2007; 21:365–369.
Article18. Anderberg L, Annertz M, Rydholm U, Brandt L, Säveland H. Selective diagnostic nerve root block for the evaluation of radicular pain in the multilevel degenerated cervical spine. Eur Spine J. 2006; 15:794–801.
Article19. Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc. 1958; 166:23–28.
Article20. Saal JA, Saal JS. Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy. An outcome study. Spine (Phila Pa 1976). 1989; 14:431–437.21. Komori H, Shinomiya K, Nakai O, Yamaura I, Takeda S, Furuya K. The natural history of herniated nucleus pulposus with radiculopathy. Spine (Phila Pa 1976). 1996; 21:225–229.
Article22. Guinto FC Jr, Hashim H, Stumer M. CT demonstration of disk regression after conservative therapy. AJNR Am J Neuroradiol. 1984; 5:632–633.23. Narouze SN. Ultrasound-guided interventional procedures in pain management: evidence-based medicine. Reg Anesth Pain Med. 2010; 35:S55–S58.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Ultrasound-guided Selective Nerve Root Injections in the Lower Cervical Spines
- Ultrasound-Guided Selective Cervical Root Block in Spondylotic Radiculopathy: Advantages and Safety
- Essential Clinical Tips about Ultrasound Guided Cervical Intervention
- The Efficacy and Persistence of Selective Nerve Root Block under Fluoroscopic Guidance for Cervical Radiculopathy
- The Value of Selective Nerve Root Block to Predict Surgical Outcome for Spinal Surgery