Ann Rehabil Med.
2014 Oct;38(5):702-706. 10.5535/arm.2014.38.5.702.
Locked-in Syndrome due to Central Pontine Myelinolysis: Case Report
- Affiliations
-
- 1Department of Rehabilitation Medicine, Chungnam National University School of Medicine, Daejeon, Korea. shapil21@cnuh.co.kr
- KMID: 2266507
- DOI: http://doi.org/10.5535/arm.2014.38.5.702
Abstract
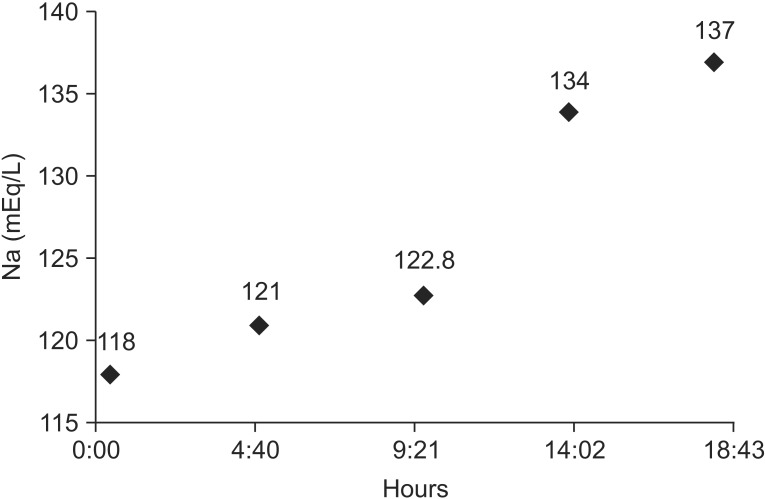
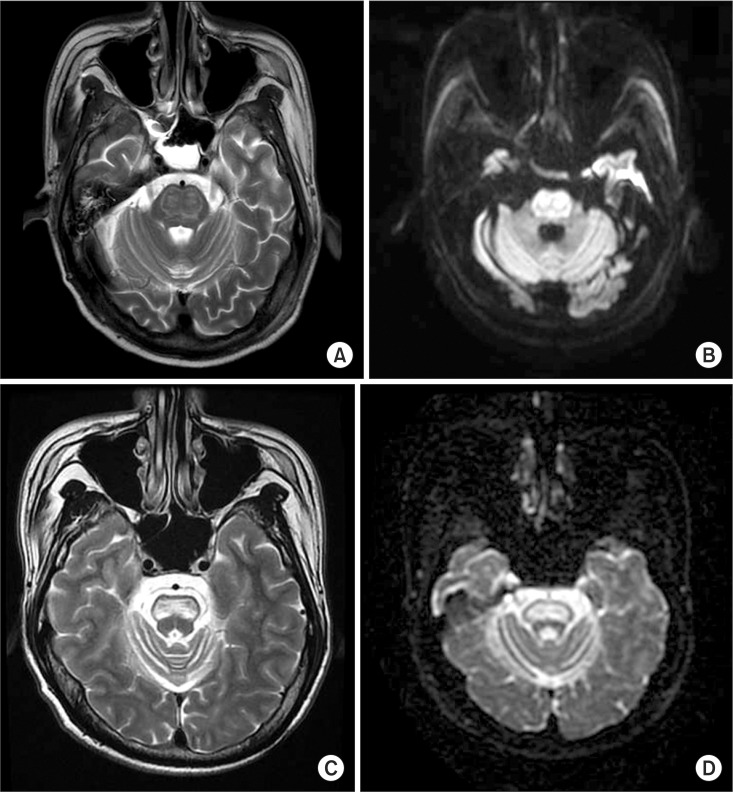
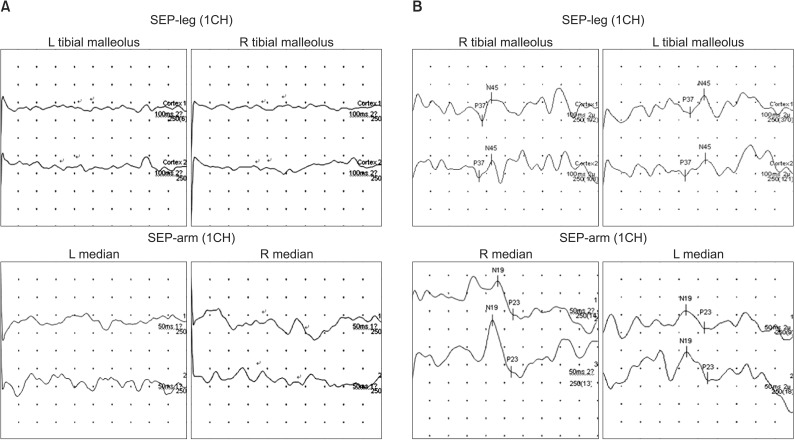
- Central pontine myelinolysis (CPM) classically occurs in alcoholics, malnourished individuals, chronic liver diseases, and rapid correction of hyponatremia. This report presents locked-in syndrome due to CPM following rapid correction of hyponatremia. A 44-year-old male came to the hospital due to a short period of loss of consciousness. He was alert and had no focal neurological abnormalities at admission. The serum sodium concentration was 118 mEq/L and was corrected to 134 mEq/L in the first 18 hours. One week later, progressive weakness in limbs developed and he progressed to a complete quadriplegic state and bulbar palsy, with only eye blinking preserved. Brain magnetic resonance imaging revealed a characteristic hyperintense signal abnormality in both pons, so he was diagnosed to locked-in syndrome caused by CPM. The patient gradually improved following continuous intensive rehabilitation for more than 2 years. He was able to move all joint muscles against gravity in generally and he could gait under supervision.
MeSH Terms
Figure
Reference
-
1. Adams RD, Victor M, Mancall EL. Central pontine myelinolysis. AMA Arch Neurol Psychiatry. 1959; 81:154–172.
Article2. Newell KL, Kleinschmidt-DeMasters BK. Central pontine myelinolysis at autopsy; a twelve year retrospective analysis. J Neurol Sci. 1996; 142:134–139. PMID: 8902733.
Article3. Lampl C, Yazdi K. Central pontine myelinolysis. Eur Neurol. 2002; 47:3–10. PMID: 11803185.
Article4. Casanova E, Lazzari RE, Lotta S, Mazzucchi A. Locked-in syndrome: improvement in the prognosis after an early intensive multidisciplinary rehabilitation. Arch Phys Med Rehabil. 2003; 84:862–867. PMID: 12808539.5. Huang WY, Weng WC, Peng TI, Ro LS, Yang CW, Chen KH. Central pontine and extrapontine myelinolysis after rapid correction of hyponatremia by hemodialysis in a uremic patient. Ren Fail. 2007; 29:635–638. PMID: 17654329.
Article6. Kwon HG, Jang SH. Motor recovery mechanism in a quadriplegic patient with locked-in syndrome. NeuroRehabilitation. 2012; 30:113–117. PMID: 22430576.
Article7. Sterns RH, Riggs JE, Schochet SS Jr. Osmotic demyelination syndrome following correction of hyponatremia. N Engl J Med. 1986; 314:1535–1542. PMID: 3713747.
Article8. Kallakatta RN, Radhakrishnan A, Fayaz RK, Unnikrishnan JP, Kesavadas C, Sarma SP. Clinical and functional outcome and factors predicting prognosis in osmotic demyelination syndrome (central pontine and/or extrapontine myelinolysis) in 25 patients. J Neurol Neurosurg Psychiatry. 2011; 82:326–331. PMID: 20826870.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of central pontine and extrapontine myelinolysis with early hypermetabolism on 18FDG-PET scan
- Central Pontine Myelinolysis Presenting With Cerebellar Ataxia
- Central Pontine and Extrapontine Myelinolysis in a Patient with Traumatic Brain Injury Following Not Rapid Correction of Hyponatremia: A Case Report
- A Case of Subacute Onset Choreoathetosis as Sequelae of Central Pontine and Extrapontine Myelinolysis
- Central Pontine Myelinolysis Induced by Alcohol Withdrawal: A Case Report