An Educational Program That Contributes to Improved Patient and Parental Understanding of Atopic Dermatitis
- Affiliations
-
- 1Department of Dermatology, Incheon St. Mary's Hospital, The Catholic University of Korea, School of Medicine, Incheon, Korea. drchos@yahoo.co.kr
- 2Department of Dermatology, Kyungpook National University School of Medicine, Daegu, Korea.
- 3Department of Dermatology, Hallym University College of Medicine, Chuncheon, Korea.
- 4Department of Dermatology, Chung-Ang University College of Medicine, Seoul, Korea.
- 5Department of Dermatology, Soonchunhyang University College of Medicine, Cheonan, Korea.
- 6Department of Dermatology, Gachon University of Medicine and Science, Incheon, Korea.
- 7Department of Dermatology, Pusan National University School of Medicine, Yangsan, Korea.
- 8Department of Dermatology, Seoul National University College of Medicine, Seoul, Korea.
- 9Department of Dermatology, Hanyang University College of Medicine, Seoul, Korea.
- KMID: 2265699
- DOI: http://doi.org/10.5021/ad.2014.26.1.66
Abstract
- BACKGROUND
Providing an educational program as part of a health care program for the management of atopic dermatitis (AD) patients has rapidly become popular. AD educational programs can be of benefit in measured outcomes for both dermatology specialists and patients.
OBJECTIVE
To determine the effects of programmed education delivered by dermatology specialists on the management and knowledge of AD, we assessed the effectiveness of patient/parental education at improving AD knowledge, and determined the usefulness of the education.
METHODS
The program consisted of five, 20-minutes sessions which were prepared, discussed, reviewed, and delivered by professors of dermatology. At the end of the program, AD knowledge was assessed using a standardized questionnaire. A total of 148 people were included. Fifty-eight patients/parents received the programmed education and the remaining 90 did not receive the programmed education.
RESULTS
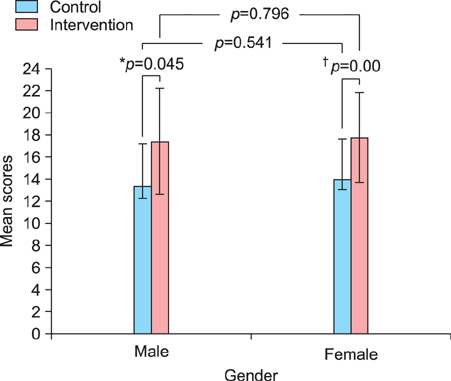
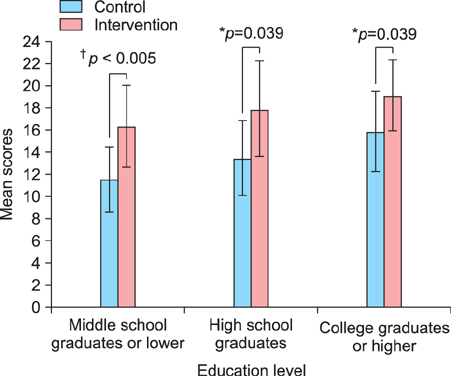
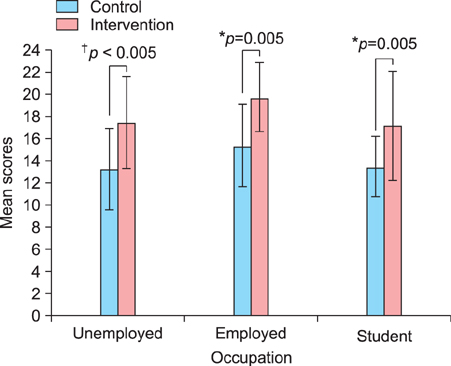
The mean questionnaire scores from both groups were compared. Mean knowledge scores were significantly higher for those who received the education (p=0.00). We analyzed the knowledge score according to factors such as gender, education level, marital status, and occupation. The data indicated that education level influences the subjects' knowledge level of AD, but gender, occupation, and marital status do not.
CONCLUSION
An educational program can be an effective tool to improve patient quality of life and treatment compliance by providing psychological support to the patients and their parents.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
Current Status of Patient Education in the Management of Atopic Dermatitis in Korea
Min Kyung Lee, Ju-Hee Seo, Howard Chu, Hyunjung Kim, Yong Hyun Jang, Jae Won Jeong, Hye Yung Yum, Man Yong Han, Ho Joo Yoon, Sang-Heon Cho, Yeong Ho Rha, Jin-Tack Kim, Young Lip Park, Seong Jun Seo, Kwang Hoon Lee, Chang Ook Park
Yonsei Med J. 2019;60(7):694-699. doi: 10.3349/ymj.2019.60.7.694.A Family-Engaged Educational Program for Atopic Dermatitis: A Seven-Year, Multicenter Experience in Daegu-Gyeongbuk, South Korea
Yong Hyun Jang, Jin Sub Lee, Sang Lim Kim, Chang Hyun Song, Hong Dae Jung, Dong Hoon Shin, Jae We Cho, Hyun Chung, Moo Kyu Suh, Do Won Kim
Ann Dermatol. 2015;27(4):383-388. doi: 10.5021/ad.2015.27.4.383.Consensus Guidelines for the Treatment of Atopic Dermatitis in Korea (Part II): Systemic Treatment
Jung Eun Kim, Hyun Jeong Kim, Bark-Lynn Lew, Kyung Ho Lee, Seung Phil Hong, Yong Hyun Jang, Kui Young Park, Seong Jun Seo, Jung Min Bae, Eung Ho Choi, Ki Beom Suhr, Seung Chul Lee, Hyun Chang Ko, Young Lip Park, Sang Wook Son, Young Jun Seo, Yang Won Lee, Sang Hyun Cho, Chun Wook Park, Joo Young Roh
Ann Dermatol. 2015;27(5):578-592. doi: 10.5021/ad.2015.27.5.578.Awareness of Atopic Dermatitis and Attitudes toward Different Types of Medical Institutions for Its Treatment among Adult Patients and the Parents of Pediatric Patients: A Survey of 500 Participants
Nam Kyung Roh, Song Hee Han, Min Jung Kim, Gyeong-Hun Park, Bark-Lynn Lew, Eung Ho Choi, Hyun Chang Ko, Young Lip Park, Sang Wook Son, Young Jun Seo, Yang Won Lee, Sang Hyun Cho, Chun Wook Park
Ann Dermatol. 2016;28(6):725-732. doi: 10.5021/ad.2016.28.6.725.A review on the role of moisturizers for atopic dermatitis
Yoke Chin Giam, Adelaide Ann Hebert, Maria Victoria Dizon, Hugo Van Bever, Marysia Tiongco-Recto, Kyu-Han Kim, Hardyanto Soebono, Zakiudin Munasir, Inne Arline Diana, David Chi Kang Luk
Asia Pac Allergy. 2016;6(2):120-128. doi: 10.5415/apallergy.2016.6.2.120.
Reference
-
1. Annesi-Maesano I, Mourad C, Daures JP, Kalaboka S, Godard P. Time trends in prevalence and severity of childhood asthma and allergies from 1995 to 2002 in France. Allergy. 2009; 64:798–800.
Article2. Eichenfield LF, Hanifin JM, Beck LA, Lemanske RF Jr, Sampson HA, Weiss ST, et al. Atopic dermatitis and asthma: parallels in the evolution of treatment. Pediatrics. 2003; 111:608–616.
Article3. Foley P, Zuo Y, Plunkett A, Marks R. The frequency of common skin conditions in preschool-age children in Australia: atopic dermatitis. Arch Dermatol. 2001; 137:293–300.4. Larsen FS, Hanifin JM. Epidemiology of atopic dermatitis. Immunol Allergy Clin North Am. 2002; 22:1–24.
Article5. Johnston GA, Bilbao RM, Graham-Brown RA. The use of complementary medicine in children with atopic dermatitis in secondary care in Leicester. Br J Dermatol. 2003; 149:566–571.
Article6. Cork MJ, Britton J, Butler L, Young S, Murphy R, Keohane SG. Comparison of parent knowledge, therapy utilization and severity of atopic eczema before and after explanation and demonstration of topical therapies by a specialist dermatology nurse. Br J Dermatol. 2003; 149:582–589.
Article7. Staab D, von Rueden U, Kehrt R, Erhart M, Wenninger K, Kamtsiuris P, et al. Evaluation of a parental training program for the management of childhood atopic dermatitis. Pediatr Allergy Immunol. 2002; 13:84–90.
Article8. Ben-Gashir MA, Seed PT, Hay RJ. Quality of life and disease severity are correlated in children with atopic dermatitis. Br J Dermatol. 2004; 150:284–290.
Article9. Atherton DJ, Sewell M, Soothill JF, Wells RS, Chilvers CE. A double-blind controlled crossover trial of an antigen-avoidance diet in atopic eczema. Lancet. 1978; 1:401–403.
Article10. Neild VS, Marsden RA, Bailes JA, Bland JM. Egg and milk exclusion diets in atopic eczema. Br J Dermatol. 1986; 114:117–123.
Article11. Mabin DC, Sykes AE, David TJ. Controlled trial of a few foods diet in severe atopic dermatitis. Arch Dis Child. 1995; 73:202–207.
Article12. Oranje AP, de Waard-van der Spek FB. Atopic dermatitis and diet. J Eur Acad Dermatol Venereol. 2000; 14:437–438.
Article13. Smith SD, Hong E, Fearns S, Blaszczynski A, Fischer G. Corticosteroid phobia and other confounders in the treatment of childhood atopic dermatitis explored using parent focus groups. Australas J Dermatol. 2010; 51:168–174.
Article14. Brown KL, Krejci-Manwaring J, Tusa MG, Camacho F, Fleischer AB Jr, Balkrishnan R, et al. Poor compliance with topical corticosteroids for atopic dermatitis despite severe disease. Dermatol Online J. 2008; 14:13.
Article15. Chamlin SL, Frieden IJ, Williams ML, Chren MM. Effects of atopic dermatitis on young American children and their families. Pediatrics. 2004; 114:607–611.
Article16. Armstrong AW, Kim RH, Idriss NZ, Larsen LN, Lio PA. Online video improves clinical outcomes in adults with atopic dermatitis: a randomized controlled trial. J Am Acad Dermatol. 2011; 64:502–507.
Article17. Moore EJ, Williams A, Manias E, Varigos G, Donath S. Eczema workshops reduce severity of childhood atopic eczema. Australas J Dermatol. 2009; 50:100–106.
Article18. Roehr B. Trend for US patients to seek health information from media and internet is stalling. BMJ. 2011; 343:d7738.
Article19. Broberg A, Kalimo K, Lindblad B, Swanbeck G. Parental education in the treatment of childhood atopic eczema. Acta Derm Venereol. 1990; 70:495–499.20. Beattie PE, Lewis-Jones MS. Parental knowledge of topical therapies in the treatment of childhood atopic dermatitis. Clin Exp Dermatol. 2003; 28:549–553.
Article21. Hughes R, Ward D, Tobin AM, Keegan K, Kirby B. The use of alternative medicine in pediatric patients with atopic dermatitis. Pediatr Dermatol. 2007; 24:118–120.
Article22. Artik S, Ruzicka T. Complementary therapy for atopic eczema and other allergic skin diseases. Dermatol Ther. 2003; 16:150–163.
Article23. Chin HW, Jang HS, Jang BS, Jo JH, Kim MB, Oh CK, et al. A study on utilization of alternative medicine for patients with atopic dermatitis. Korean J Dermatol. 2005; 43:903–911.24. Jensen P. Use of alternative medicine by patients with atopic dermatitis and psoriasis. Acta Derm Venereol. 1990; 70:421–424.25. Hauk PJ. The role of food allergy in atopic dermatitis. Curr Allergy Asthma Rep. 2008; 8:188–194.
Article26. Chong SJ, Kim KH, Kim DW, Kim SJ, Kim IJ, Kim CW, et al. Report from ADRG: a study on the clinical manifestations of childhood atopic dermatitis in Korea. Korean J Dermatol. 2005; 43:1497–1509.27. Shin HJ, Yoon SM, Oh SY, Oh JK. The analysis of the present status of the medical internet sites in Korea. J Korean Acad Fam Med. 2000; 21:792–800.28. Kwon HJ, Kim YJ, Park SB, Yu DS, Kim JW. Study of atopic dermatitis information on the internet in Korea. Korean J Dermatol. 2006; 44:137–140.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relationship between Child and Adolescent Atopic Dermatitis, Attachment and the Quality of Parental Life
- Measurement of Atopic Dermatitis Disability
- The Environment and Lifestyles of Atopic Dermatitis Patients
- Serum IgE Level in Patients of Atopic Dermatitis and Atopic Dermatitis with Molluscum Contagiosum
- Current Understanding of Atopic Dermatitis