Allergy Asthma Immunol Res.
2012 Mar;4(2):85-91. 10.4168/aair.2012.4.2.85.
IgE Sensitization to Cephalosporins in Health Care Workers
- Affiliations
-
- 1Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- 2Department of Allergy & Clinical Immunology, Ajou University School of Medicine, Suwon, Korea. hspark@ajou.ac.kr
- 3Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea.
- KMID: 2260364
- DOI: http://doi.org/10.4168/aair.2012.4.2.85
Abstract
- PURPOSE
Cephalosporins can induce occupational allergies, such as asthma, urticaria, and anaphylaxis. We investigated the prevalence and risk factors of sensitization to cephalosporin.
METHODS
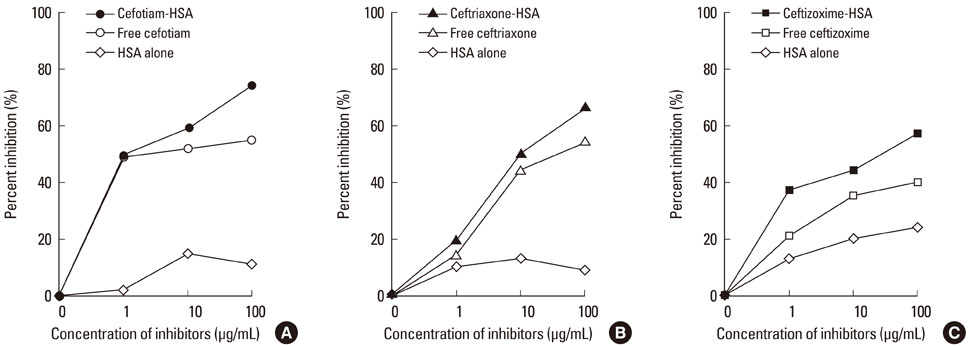
A total of 161 health care workers (HCW), including 138 nurses and 23 pharmacists, and 86 unexposed non-atopic healthy controls were recruited from a single tertiary hospital and the general population. A questionnaire regarding work-related symptoms was administered along with skin prick tests (SPT) to the three most commonly used cephalosporins (cefotiam, ceftriaxone, and ceftizoxime). Serum specific IgE antibodies to conjugates of the three cephalosporins and human serum albumin (HSA) were measured by enzyme-linked immunosorbent assay (ELISA). Binding specificities were confirmed by ELISA inhibition tests.
RESULTS
The prevalence of work-related symptoms in association with cephalosporins was 17.4%. The sensitization rate to any cephalosporin was 3.1% by SPT. Sensitization rates determined by measurement of serum specific IgE antibodies were 17.4% for any cephalosporin, 10.4% for cefotiam, 6.8% for ceftriaxone, and 3.7% for ceftizoxime. A personal history of any antibiotic allergy was a risk factor for work-related symptoms (OR, 24.93; 95% CI, 2.61-238), but not for the presence of serum specific IgE antibodies to cephalosporins (OR, 0.9; 95% CI, 0.18-4.53). A personal history of atopic dermatitis was a risk factor for the presence of serum specific IgE antibodies to cefotiam-HSA conjugate (OR, 6.30; 95% CI, 1.23-32.3).
CONCLUSIONS
A high cephalosporin sensitization rate (17.4%) was detected by ELISA in HCW exposed to cephalosporins. Monitoring of serum specific IgEs to cephalosporin-HSA conjugates will be useful for detecting sensitized subjects.
Keyword
MeSH Terms
-
Anaphylaxis
Antibodies
Asthma
Cefotiam
Ceftizoxime
Ceftriaxone
Cephalosporins
Delivery of Health Care
Dermatitis, Atopic
Enzyme-Linked Immunosorbent Assay
Humans
Hypersensitivity
Immunoglobulin E
Occupational Diseases
Pharmacists
Prevalence
Risk Factors
Serum Albumin
Skin
Tertiary Care Centers
Urticaria
Surveys and Questionnaires
Antibodies
Cefotiam
Ceftizoxime
Ceftriaxone
Cephalosporins
Immunoglobulin E
Serum Albumin
Figure
Cited by 1 articles
-
Immunologic Evaluation of Immediate Hypersensitivity to Cefaclor
Hye-Soo Yoo, Seung-Hyun Kim, Hyouk-Soo Kwon, Tae-Bum Kim, Young-Hee Nam, Young-Min Ye, Hae-Sim Park
Yonsei Med J. 2014;55(6):1473-1483. doi: 10.3349/ymj.2014.55.6.1473.
Reference
-
1. Suneja T, Belsito DV. Occupational dermatoses in health care workers evaluated for suspected allergic contact dermatitis. Contact Dermatitis. 2008. 58:285–290.2. Delclos GL, Gimeno D, Arif AA, Burau KD, Carson A, Lusk C, Stock T, Symanski E, Whitehead LW, Zock JP, Benavides FG, Antó JM. Occupational risk factors and asthma among health care professionals. Am J Respir Crit Care Med. 2007. 175:667–675.3. Kim JE, Kim SH, Choi GS, Ye YM, Park HS. Detection of specific IgE antibodies to cefotiam-HSA conjugate by ELISA in a nurse with occupational anaphylaxis. Allergy. 2010. 65:791–792.4. Tadokoro K, Niimi N, Ohtoshi T, Nakajima K, Takafuji S, Onodera K, Suzuki S, Muranaka M. Cefotiam-induced IgE-mediated occupational contact anaphylaxis of nurses; case reports, RAST analysis, and a review of the literature. Clin Exp Allergy. 1994. 24:127–133.5. Chiba Y, Takahashi S, Yamakawa Y, Aihara M, Ikezawa Z. Contact urticaria syndrome caused by patch testing with cefotiam hydrochloride. Contact Dermatitis. 1999. 41:234.6. Ryu HC, Park HS, Lee SM, Koo TH, Shin BC, Kim BK, Seo HR, Heo JH, Yang DK, Lee SK, Son CH. A case of occupational asthma caused by cefotiam (Fontiam®) in a nurse. Korean J Asthma Allergy Clin Immunol. 2008. 28:152–155.7. Gielen K, Goossens A. Occupational allergic contact dermatitis from drugs in healthcare workers. Contact Dermatitis. 2001. 45:273–279.8. Hur GY, Shin SY, Ye YM, Nahm DH, Park HS. Two cases of occupational rhinitis caused by biodiastase in hospital and pharmaceutical workers. Allergy. 2007. 62:1096–1097.9. Rudzki E, Rebandel P. Occupational contact urticaria from penicillin. Contact Dermatitis. 1985. 13:192.10. Suh YJ, Lee YM, Choi JH, Suh CH, Nahm DH, Park HS. Heterogeneity of IgE response to cefteram pivoxil was noted in 2 patients with cefteram-induced occupational asthma. J Allergy Clin Immunol. 2003. 112:209–210.11. Park HS, Kim KU, Lee YM, Choi JH, Lee JH, Park SW, Jang AS, Park CS. Occupational asthma and IgE sensitization to 7-aminocephalosporanic acid. J Allergy Clin Immunol. 2004. 113:785–787.12. Choi IS, Han ER, Lim SW, Lim SR, Kim JN, Park SY, Chae SK, Lim HH, Seol YA, Bae YI, Won YH. Beta-lactam antibiotic sensitization and its relationship to allergic diseases in tertiary hospital nurses. Allergy Asthma Immunol Res. 2010. 2:114–122.13. Cetinkaya F, Ozturk AO, Kutluk G, Erdem E. Penicillin sensitivity among hospital nurses without a history of penicillin allergy. J Adv Nurs. 2007. 58:126–129.14. Pearce N, Weiland S, Keil U, Langridge P, Anderson HR, Strachan D, Bauman A, Young L, Gluyas P, Ruffin D, Crane J, Beasley R. Self-reported prevalence of asthma symptoms in children in Australia, England, Germany and New Zealand: an international comparison using the ISAAC protocol. Eur Respir J. 1993. 6:1455–1461.15. Rose BG, Kamps-Holtzapple C, Stanker LH. Competitive indirect ELISA for ceftiofur sodium and the effect of different immunizing and coating antigen conjugates. Bioconjug Chem. 1995. 6:529–535.16. Torres MJ, Romano A, Mayorga C, Moya MC, Guzman AE, Reche M, Juarez C, Blanca M. Diagnostic evaluation of a large group of patients with immediate allergy to penicillins: the role of skin testing. Allergy. 2001. 56:850–856.17. Torres MJ, Blanca M, Fernandez J, Romano A, Weck A, Aberer W, Brockow K, Pichler WJ, Demoly P. Diagnosis of immediate allergic reactions to beta-lactam antibiotics. Allergy. 2003. 58:961–972.18. Demoly P, Bousquet J. Drug allergy diagnosis work up. Allergy. 2002. 57:Suppl 72. 37–40.19. Perez-Inestrosa E, Suau R, Montañez MI, Rodriguez R, Mayorga C, Torres MJ, Blanca M. Cephalosporin chemical reactivity and its immunological implications. Curr Opin Allergy Clin Immunol. 2005. 5:323–330.20. Choi HJ, Song JY, Park YM, Kim CW, Kim HO. Case reports: occupational contact urticaria syndrome induced by cefotiam dihydrochloride in a nurse. Ann Dermatol. 2003. 15:113–115.21. Lee JY, Kim GI, Park CW, Lee CH. Two cases of cefotiam-induced contact urticaria syndrome. Ann Dermatol. 2000. 12:119–121.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Identifying Genetic Susceptibility to Sensitization to Cephalosporins in Health Care Workers
- Exposure and Elevated Serum Total Immunoglobulin E Level are Major Risk Factors of Sensitization to Pancreatic Enzymes among Health Care Workers in a Single Hospital
- Occupational asthma and IgE sensitization in a pharmaceutical company processing cefteram pivoxil
- IgE-Mediated Hypersensitivity Reactions to Cephalosporins
- Diagnosis and Management of Immediate Hypersensitivity Reactions to Cephalosporins