Korean J Hematol.
2006 Mar;41(1):36-40. 10.5045/kjh.2006.41.1.36.
Pre-transplant Disease Status is Important for an Improved Outcome of the Second Stem Cell Transplantation in the Myeloma Patients Receiving the First Autologous Stem Cell Transplantation
- Affiliations
-
- 1Catholic Hemopoietic Stem Cell Transplantation Center, The Catholic University of Korea, Seoul, Korea. ckmin@catholic.ac.kr
- KMID: 2252325
- DOI: http://doi.org/10.5045/kjh.2006.41.1.36
Abstract
-
BACKGROUND: Double autologous stem cell transplantation (ASCT) seems to be superior to a single ASCT, at least in the patients who did not achieve a 90% response after the first transplant. An allogeneic SCT with a dose-reduced conditioning regimen after ASCT and as part of the initial therapy, might be a feasible and highly effective approach. The aim of this study was to determine the prognostic factors that are associated with the outcome of multiple myeloma (MM) patients who had received a second transplant.
METHODS
From April 1996 to December 2004, 38 MM patients, who had previously received high-dose melphalan (200 mg/m2) with autologous stem cell support, underwent a second transplant. Following the 1(st) ASCT, 24 patients received a second ASCT and 14 received a tandem reduced-intensity conditioning allogeneic stem cell transplantation (RIST) from their HLA-matched siblings.
RESULTS
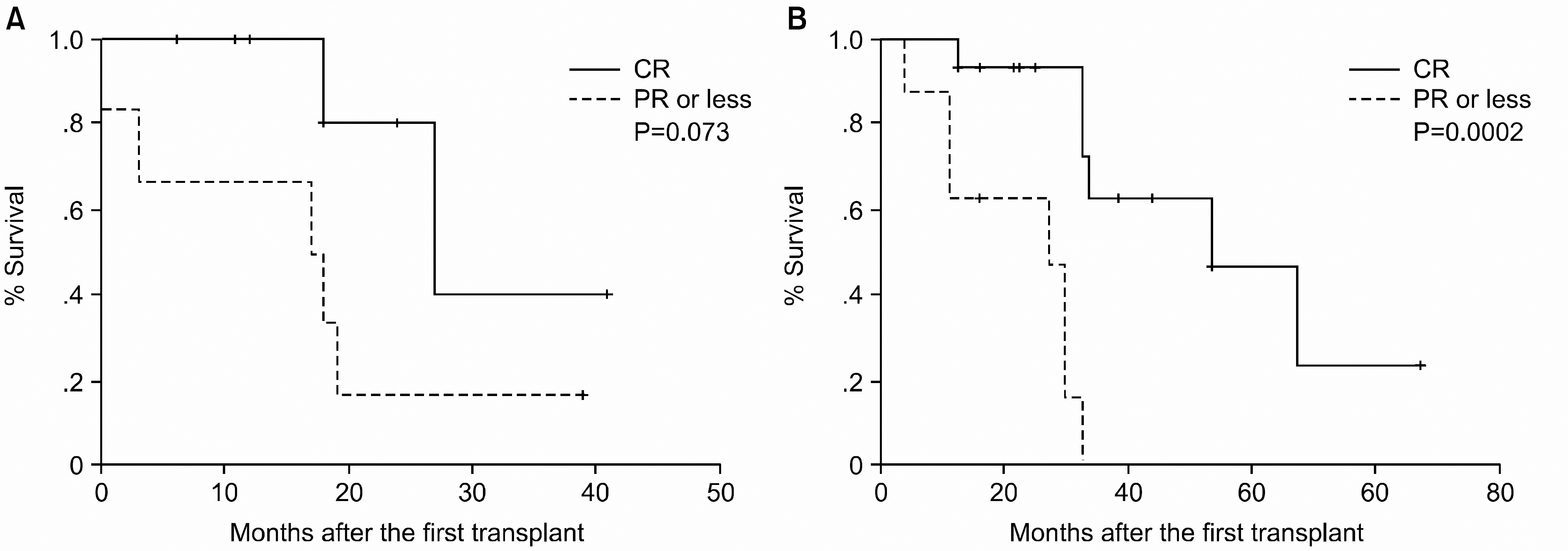
The 3-year estimated PFS and overall survival (OS) from the time of the first ASCT were 25.2% and 77.6%, respectively. The median PFS and OS were 26 months (95% CI, 23~29) and 60 months (95% CI, 44~76), respectively. The disease status (a CR vs. PR or less) at the second transplant was be the most powerful factor for improving the PFS (P=0.001, hazard ratio 5.8, 95% CI 2.1~16.1).
CONCLUSION
Patients whose disease is sensitive to chemotherapy and who obtain a CR after a single transplantation might benefit the most from a second transplant.
Keyword
MeSH Terms
Figure
Reference
-
1). Child JA., Morgan GJ., Davies FE, et al. Medical Research Council Adult Leukaemia Working Party. High-dose chemotherapy with hematopoietic stem-cell rescue for multiple myeloma. N Engl J Med. 2003. 348:1875–83.2). Harousseau JL., Milpied N., Laporte JP, et al. Double-intensive therapy in high-risk multiple myeloma. Blood. 1992. 79:2827–33.
Article3). Vesole DH., Barlogie B., Jagannath S, et al. High-dose therapy for refractory multiple myeloma: improved prognosis with better supportive care and double transplants. Blood. 1994. 84:950–6.
Article4). Maloney DG., Molina AJ., Sahebi F, et al. Allografting with nonmyeloablative conditioning following cytoreductive autografts for the treatment of patients with multiple myeloma. Blood. 2003. 102:3447–54.
Article5). Kroger N., Schwerdtfeger R., Kiehl M, et al. Autologous stem cell transplantation followed by a dose-reduced allograft induces high complete remission rate in multiple myeloma. Blood. 2002. 100:755–60.6). Attal M., Harousseau JL., Facon T, et al. InterGroupe Francophone du Myelome. Single versus double autologous stem-cell transplantation for multiple myeloma. N Engl J Med. 2003. 349:2495–502.
Article7). Neumann F., Graef T., Tapprich C, et al. Cyclosporine A and mycophenolate mofetil vs cyclosporine A and methotrexate for graft-versus-host disease prophylaxis after stem cell transplantation from HLA-identical siblings. Bone Marrow Transplant. 2005. 35:1089–93.
Article8). Glucksberg H., Storb R., Fefer A, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HLA-matched sibling donors. Transplantation. 1974. 18:295–304.
Article9). Shulman HM., Sullivan KM., Weiden PL, et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med. 1980. 69:204–17.10). Alyea E., Weller E., Schlossman R, et al. Outcome after autologous and allogeneic stem cell transplantation for patients with multiple myeloma: impact of graft-versus-myeloma effect. Bone Marrow Transplant. 2003. 32:1145–51.
Article11). Lahuerta JJ., Grande C., Martinez-Lopez J, et al. Grupo Espanol de Sindromes Linfoproliferativos/Trasplante Autologo de Medula Osea. Tandem transplants with different high-dose regimens improve the complete remission rates in multiple myeloma. Results of a Grupo Espanol de Sindromes Linfopro-liferativos/Trasplante Autologo de Medula Osea phase II trial. Br J Haematol. 2003. 120:296–303.12). Alexanian R., Weber D., Giralt S, et al. Impact of complete remission with intensive therapy in patients with responsive multiple myeloma. Bone Marrow Transplant. 2001. 27:1037–43.
Article13). Blade J., Esteve J., Rives S, et al. High-dose therapy autotransplantation/intensification vs continued standard chemotherapy in multiple myeloma in first remission. Results of a non-randomized study from a single institution. Bone Marrow Transplant. 2000. 26:845–9.
Article14). Lokhorst HM., Schattenberg A., Cornelissen JJ, et al. Donor lymphocyte infusions for relapsed multiple myeloma after allogeneic stem-cell transplantation: predictive factors for response and long-term outcome. J Clin Oncol. 2000. 18:3031–37.
Article15). Sarasquete ME., Garcia-Sanz R., Gonzalez D, et al. Minimal residual disease monitoring in multiple myeloma: a comparison between allelic-specific oligonucleotide real-time quantitative polymerase chain reaction and flow cytometry. Haematologica. 2005. 90:1365–72.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Scleroderma following Autologous Peripheral Stem Cell Transplantation
- A Case of Cerebral Toxoplasmosis Following Tandem Autologous Stem Cell Transplantation in a Multiple Myeloma Patient
- Emergence of chronic myeloid leukemia following autologous stem cell transplantation in a young woman with multiple myeloma
- Hematopoietic stem cell transplantation: overview for general pediatrician
- Clinical utilization of cord blood over human health: experience of stem cell transplantation and cell therapy using cord blood in Korea